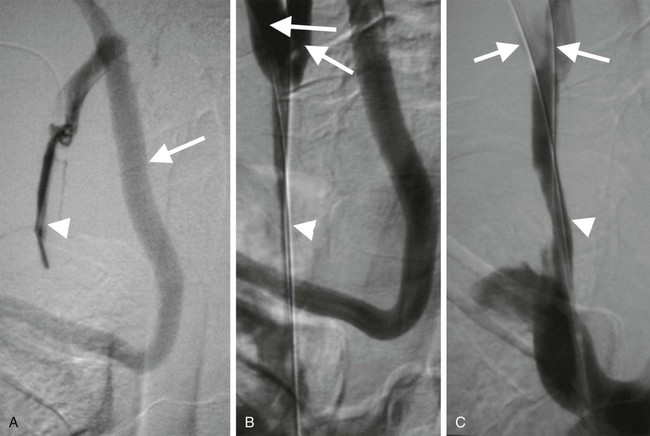
The National Institute of Clinical Excellence has recommended that ultrasound guidance should be used when inserting elective central venous lines.1 There is clear evidence that using imaging guidance increases success rates and reduces complications associated with jugular and subclavian vein puncture. Most of these routine procedures do not require interventional radiologic input, but interventional radiologists become indispensable in cases where central venous access is difficult, as is often the case in hemodialysis and cancer patients.2 Venous access is the starting point for a large number of diagnostic and therapeutic interventions in the systemic and portal venous circulations. Table 29-1 lists typical indications. TABLE 29-1 Interventional Procedures Requiring Venous Access It is sometimes necessary to predilate a stenosed or occluded vein prior to passage of a line (Fig. 29-1). Stents are generally unnecessary, however, if access rather than patency is the desired outcome. Several considerations may be relevant when planning the optimal approach for venous access. The general adage that the shortest, straightest route is best often applies, but this should be weighed against possible disadvantages of choosing a particular site. Typical approaches are outlined in Table 29-1, but there are also some esoteric routes typically reserved for cases wherein all other options have failed. These include utilizing collateral veins, transhepatic, translumbar, or transrenal access to the systemic veins and transsplenic or transmesenteric access to the portal venous system. There are occasions when dual access is helpful, especially when the most direct route is through a small vessel or via an artery. Central venous access is the starting point for many procedures (see Table 29-1). The most common points of access are the internal jugular and subclavian veins. The jugular vein is superior to the subclavian vein because it is less prone to symptomatic thrombosis.3 The right internal jugular vein also provides the shortest, straightest route and is the first-choice point of access. The left jugular approach is often possible, but it is important to be aware of any sharp bends in the mediastinum that may result in kinking of sheaths (Fig. 29-2). It is prudent to check the manufacturer’s instructions for use; there are sometimes caveats to using the left jugular approach for this reason.
Principles of Venous Access
Clinical Relevance
Indications
Procedure
Typical Approach
Diagnostic
Venography
Appropriate peripheral vein
Venous sampling
Femoral vein
Pulmonary angiography
Femoral vein
Therapeutic—Systemic
Venous angioplasty, stenting, and thrombolysis
Appropriate peripheral vein
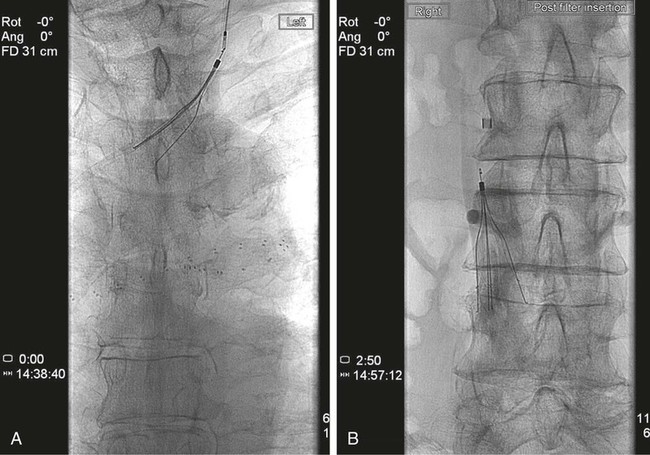
IVC filter placement
Jugular vein
Tunneled central line insertion
Jugular vein
Repositioning/stripping of lines
Femoral vein
Management of SVCO/IVCO
Jugular vein
Transjugular liver biopsy
Jugular vein
Varicocele and ovarian vein embolization
Femoral vein
Varicose vein ablation
Appropriate peripheral vein
Therapeutic—Portal
TIPS
Jugular vein
Portal vein embolization
Transhepatic
Post transplant portal vein intervention
Transhepatic
Equipment
Ultrasound
Angioplasty Balloons and Stents
Technique
Anatomy and Approach
Central Venous Access
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Principles of Venous Access