Protocol ID
Study design
Dose fractionation (GyE/fractions/weeks)
Materials
Period
Number of patients (~13.3)
9402
Dose escalation
54.0–72.0/20/5
T2b–T3N0M0
95.6–97.12
35
9703
Dose escalation
60.0–66.0/20/5
T1–T3N0M0
98.1–00.2
61
9904 (1)
Phase II
66.0/20/5
T1–T3N0M0
00.4–03.11
175
9904 (2)
AM*
66.0, 63.0/20/5
T1–T3N0M0
03.12–07.8
291
9904 (3)
AM
57.6/16/4
T1–T3N0M0
07.9
1,107
1002
Dose escalation
51.6/12/3
T1–T3N0M0
10.7–12.2
64
Total
95.6
1,733
27.3 Methods of C-Ion RT at NIRS
27.3.1 Patient Immobilization
For patient immobilization, the patient is placed in a supine position and devices for immobilizing the feet and pelvis are fabricated. First, using customized cradles (Moldcare; Alcare, Tokyo, Japan), the feet are immobilized to avoid inter-fractional variation in the position and angle of the feet and toes. Next, the pelvis is tightly immobilized with a low-temperature thermoplastic (Shellfitter; Keraray Co., Ltd., Osaka, Japan). The effects of respiration on prostate motion were evaluated based on the analysis of 4-dimensional CT images [5, 24]. It was confirmed that, with these immobilization devices, the prostate movement with respiration was almost negligible so that we decided not to employ respiratory-gated irradiation in C-ion RT of prostate cancer at NIRS.
When the irradiation is applied from the anterior direction, the bladder is filled with a known volume (e.g., 100 mL) of sterilized water both at the time of CT acquisition and at each treatment session. However, when only the lateral fields are used (e.g., a treatment of 12 fractions with scanning irradiation at NIRS), it is not needed to fill the bladder with sterilized water, and the bladder volume is just measured with planning CT images.
A rectal balloon is not used. Instead, the patients are instructed to empty the rectum in his/her daily effort and to use a laxative or enema, if necessary.
27.3.2 Target Delineation
With the patient lying in the immobilization devices, a set of 2.5-mm-thick CT images is taken for treatment planning. The clinical target volume (CTV) is defined as comprising the prostate and seminal vesicle (SV), as demonstrated on CT images, irrespective of T-stage and risk factors (Fig. 27.1a). However, the whole SV is not always included in the CTV for patients with a low risk. For example, the CTV of patients staged T1 or T2a does not cover the SV tips. Furthermore, anterior and lateral safety margins of 10 mm and a posterior margin of 5 mm are added to the CTV to create the initial planning target volume (PTV1). For reducing the dose to the anterior rectal wall, a rectum-sparing target volume (PTV2) is used for the latter half of the C-ion RT, with the posterior margin reduced to the anterior boundary of the rectum (Fig. 27.1b). A compensation bolus is fabricated for each patient to make the distal configuration of the SOBP similar to the PTV. The collimator defines the outline of the PTV.


Fig. 27.1
(a) Clinical target volume is the prostate and seminal vesicle in principle, but the whole seminal vesicle is not always included, mainly depending on clinical stage. The initial planning target volume, PTV-1, is defined as the CTV plus 10-mm margins in all directions except for posterior margins of 5 mm. (b) For the latter half of the treatment at the NIRS, the posterior margin is reduced to the anterior boundary of the rectum to form the secondary planning target volume, PTV-2, for reducing the risk of rectal toxicity
27.3.3 Dose Prescription at NIRS
For passive beam irradiation at NIRS, C-ion RT was performed with five irregularly shaped ports: (1) one anterior-posterior port, (2) a pair of lateral ports for the PTV1, and (3) a pair of lateral ports for the PTV2. One port was used at each treatment session. One hundred percent of the prescribed dose was given at the maximum dose point of each portal. The PTV2 was covered with at least 90 % of the prescribed dose. The minimum dose of the PTV1 was more than 50 % of the maximum dose and depended on the volume spared by PTV2. Figure 27.2 shows the representative dose distribution of the passive beam delivery.
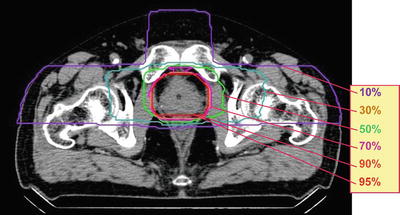
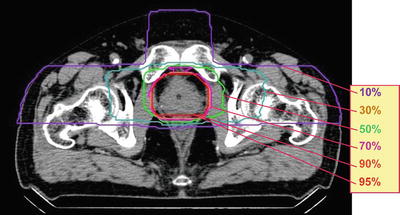
Fig. 27.2
Representative dose distribution of passive irradiation at the NIRS. Prescribed dose is a 66 or 63 GyE at the isocenter for the treatment of 20 fractions and 57.6 GyE for 16 fractions
A dose-volume histogram (DVH) is calculated to evaluate the planned dose distribution, particularly for the rectum [25]. A reference DVH of the rectum has been obtained from the initial toxicity study on C-ion RT at NIRS, which is the average DVH of patients with grade 1 or less rectal toxicity in the first and second dose-escalation trials (Fig. 27.3). A plan for a new patient is then compared with the reference DVH to avoid the rectal DVH from exceeding the reference DVH, especially at the high-dose level.
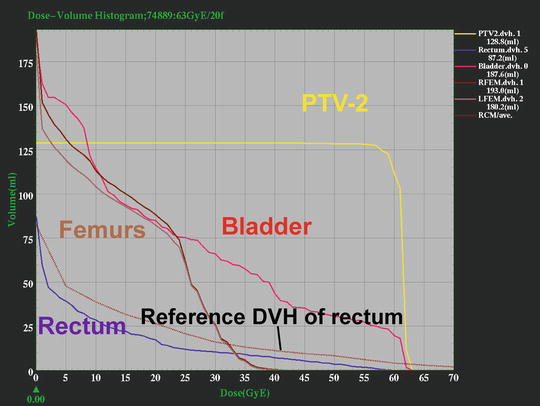
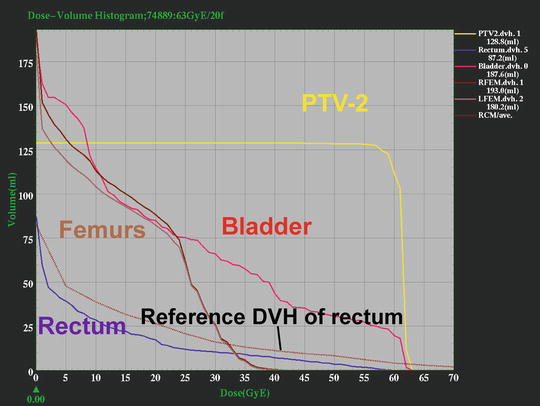
Fig. 27.3
Dose constraints at the NIRS by using a dose-volume histogram. The reference DVH, brown dotted line in the graph, is an average DVH of the patients with grade 0 or 1 rectal complication in the early dose-escalation studies. A new plan is made in order that the rectal DVH is below the reference line particularly at high-dose level
From the experience of treating pelvic tumors, including prostate cancer, gynecological cancer, and recurrent rectal cancer, at the NIRS, the dose constraints of the digestive tract in the C-ion RT were established (Table 27.2). According to these constraints, the percent rectal volume receiving 56.0 GyE in 16 fractions should not exceed 5 %, and this agrees well with the constraint using the DVH (Fig. 27.3).
Table 27.2
Dose constraints of digestive tract in carbon-ion radiotherapy
Dose limits | |||
|---|---|---|---|
20 Fractions | 16 Fractions | EDa in 2 GyE/f | |
Rectum | |||
D max(GyE) | 66.0 | 60.8 | 83.2 |
D 5%(GyE) | 60.0 | 56.0 | 72.0 |
D 10%(GyE) | 50.0 | 46.4 | 55.0 |
D 20%(GyE) | 30.0 | 28.8 | 27.0 |
Small intestine | |||
D max(GyE) | 50.0 | 48.0 | 52.0 |
27.3.4 Field Positioning
At NIRS, the C-ion RT is carried out once a day, with four fractions per week (from Tuesday to Friday). When the treatment is given from the anterior port, the bladder is filled with the sterilized water each time just before the patient setup. Verification of the field is carried out at every treatment session with a computer-aided online positioning system to maintain a positioning error within less than 2 mm [5, 6]. A rectal balloon and respiratory-gated irradiation were not used in this treatment.
27.3.5 Scanning Irradiation and Passive Irradiation in Prostate Cancer
At NIRS, beam delivery with spot scanning became available in 2011. Currently, almost all of the patients with prostate cancer are treated with this spot scanning method. This is based on our judgment that spot scanning could provide an even better dose distribution than the passive beam method in the treatment of prostate cancer. Figure 27.4 shows the dose distributions of passive beam (a) and scanning beam (b). The plan using passive beam irradiation is calculated for the anterior and two lateral directions. The plans for scanning beam irradiation are made using only two lateral beams. The dose to the hip joint is apparently reduced in the plan for scanning beam irradiation with two ports when compared to the one using passive beam irradiation with three ports.
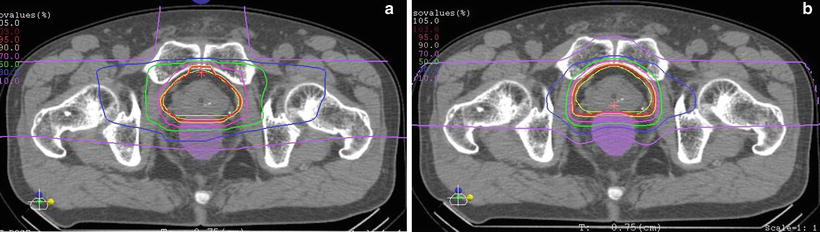
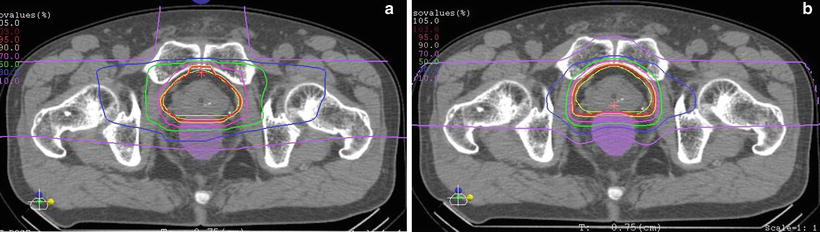
Fig. 27.4
(a) Dose distribution of the passive irradiation with three ports. (b) Dose distribution of the scanning irradiation with two ports. Dose to the hip joint can be reduced with scanning technique of two ports compared to 3-port passive irradiation
In addition, the irradiated volume of the rectum can be a little smaller in the plan using scanning irradiation than the one using passive irradiation, as demonstrated by the DVH (Fig. 27.5). Filling the bladder with sterilized water is needed for irradiation from the anterior port, while the treatment using only the lateral ports is more comfortable for the patient. From this point of view, it is important that the two lateral ports of scanning irradiation do not deliver a higher dose to the rectum and the hip joint as compared to the three ports of passive irradiation.
Fig. 27.5
Comparison between dose-volume histograms of the rectum by beam delivery method. Irradiated volume of the rectum is slightly smaller with scanning than passive
Since the intra-treatment motion of the prostate immobilized using the method at NIRS was confirmed to be very small [24], scanning irradiation can be safely applied to prostate cancer.
27.3.6 Androgen Deprivation Therapy (ADT)
The use of ADT combined with RT is still controversial. ADT consisting of medical or surgical castration with or without antiandrogen is administered according to the risk group for prostate cancer at NIRS. Before the start of C-ion RT, neoadjuvant ADT is given to patients in the intermediate and high-risk groups for 2–6 months. Adjuvant ADT is continued for a duration of 6 months for intermediate-risk patients and for 2 years for high-risk patients. Neither neoadjuvant nor adjuvant ADT is given to patients in the low-risk group [5, 6, 26].
27.4 Up-to-Date Results of C-Ion RT at NIRS
As of February 2013, 1,733 patients have received C-ion RT for prostate cancer at NIRS (Table 27.1). Of them, 1,479 patients were treated during or after the phase II trial started in 2000 and were followed up for at least 6 months. The overall survival rate of this entire group was 95.1 % at 5 years and 79.6 % at 10 years by a Kaplan-Meier estimation (Fig. 27.6




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree