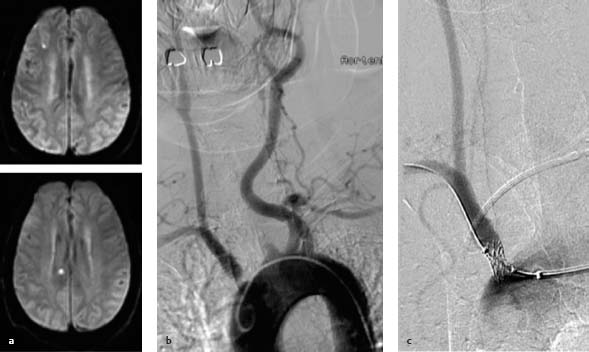
15 Proximal Stenosis of Supra-aortic Vessels Much less attention has been paid to proximal supraaortic stenoses than to the more common stenoses of the carotid bifurcation. This is partly because atherosclerotic plaques in the brachiocephalic trunk, proximal common carotid artery, and subclavian artery are less common than bifurcation stenoses. Moreover, the supraaortic stenoses are probably less often embolic and are less likely to cause neurologic symptoms. Based on epidemiologic estimates, subclavian stenosis is present in 2% of the population and in 7% of patients in medical institutions. Smoking, hypertension, hypercholesterolemia, and the presence of peripheral arterial occlusive disease are considered the main risk factors (Shadman et al. 2004). According to recent data, proximal stenoses cause ~5% of severe life-threatening strokes and thus play a minor role compared with the more dangerous carotid and proximal vertebral artery stenoses (Mazighi et al. 2009). Although the risk of stroke is relatively low, subclavian stenosis has been identified as a risk factor for significantly increased mortality from cardiovascular disease (Aboyans et al. 2007). Besides embolic ischemia, subclavian or innominate stenosis also gives rise to steal phenomena such as flow reversal in the vertebral artery and flow diversion to the arm, which may cause hemodynamic problems in the posterior circulation during exercise (see Chapter 13). The stroke risk in patients with steal phenomena is not precisely known. Based on observations in older case series, transient ischemia is relatively common although strokes appear to be rare (Moran et al. 1988). Atherosclerosis is by far the most dominant cause of proximal stenoses and rare aneurysmal vascular dilatations. Nonatheromatous stenoses may result from an inflammatory process (e.g., Takayasu arteritis), aortic dissections spreading into the origins of the cervicobrachial arteries, traumatic vascular injuries, and compression syndromes involving more distal portions of the subclavian artery. Long-segment stenoses of the common carotid artery have also been observed following radiation to the neck. It is sometimes difficult to appreciate the relationship between clinical manifestations and a proximal stenosis. Of course, there are patients who manifest neurologic symptoms in the form of transient ischemic attacks or stroke. Because most patients have subclavian stenosis, it is more common to find symptoms relating to the posterior circulation such as rotary or staggering vertigo, dysarthria, diplopia, and visual field defects rather than hemispheric symptoms with hemiplegia or aphasia. Caution Many patients with subclavian stenosis complain of nonspecific dizziness, and even neurologists may find it difficult to establish a cause. Imaging studies, preferably MRI, can make it easier to appreciate the clinical significance of a stenosis by demonstrating infarctions in the territory of the stenosed vessel. Diffusion-weighted MRI showing new lesions consistent with the patient’s symptoms may even be diagnostic and aid in therapeutic decision-making (Fig. 15.1.) Most recent publications on proximal stenoses are aimed more at cardiologists than neurologists and contain little information on neurologic deficits. Stenoses that cause steal phenomena may present clinically with exercise-dependent syncope, vertigo, and impaired consciousness (Khurana et al. 2009). Some patients complain of pulsatile tinnitus due to the collateral recruitment of external carotid artery branches (Lehmann et al. 2005). Subclavian and innominate stenoses may also present with nonneurologic symptoms such as exercise-dependent arm pain. There have been recent reports of proximal subclavian stenosis and acute coronary syndrome in patients with a mammary artery bypass graft as well as steal phenomena induced by the stenosis (Lelek et al. 2008). Fig. 15.1a–c Diagnostic imaging and intervention in a 67-year-old man with recurrent right hemispheric transient ischemic attacks. a Two fresh microembolic infarctions are detected in the right carotid territory. b Survey angiogram of the aortic arch demonstrates a stenosis of the brachiocephalic trunk. c The stenosis is recanalized with a balloon-expandable stent delivered through a long transfemoral sheath Note Side-to-side comparison of blood pressures and pulses is an important screening aid for stenoses involving the subclavian artery. Blood pressure differences > 15 mmHg are suggestive of stenosis (Shadman et al. 2004). A strong radial artery pulse tends to exclude the presence of a high-grade ipsilateral subclavian stenosis. Noninvasive screening with Doppler ultrasound is not as well standardized for proximal stenoses as it is for carotid bifurcation stenosis. Stenoses close to the aortic arch are difficult to evaluate with ultrasound. Accurate localization of the stenosis is difficult, and poststenotic flow changes such as decreased flow velocity or flow reversal are often the only demonstrable findings. Moderately severe stenoses that are not hemodynamically significant are difficult to detect with ultrasound (Widder and Göortler 2004). Accordingly, equivocal cases should additionally be evaluated by another vascular imaging modality. The standard method for this purpose is contrast-enhanced MRA. Although the degree of stenosis is occasionally distorted by flow artifacts arising near the aortic arch, contrast-enhanced MRA is still preferred to the less artifact-prone CTA owing to the lack of radiation exposure and greater ease of image postprocessing (Cosottini et al. 2003). It appears that high-field imaging at 3 T and parallel image acquisition can largely offset the disadvantages of contrast-enhanced MRA, allowing stenoses to be evaluated as accurately as with CTA or conventional DSA (Nael et al. 2007). Catheter angiography is performed in doubtful cases and to aid the planning of surgical and interventional procedures. Note Clinical manifestations and diagnostic studies: • Usually generalized atherosclerosis with localized arterial occlusive disease • Transient ischemic attacks or stroke, often in the posterior circulation • Exercise-dependent syncopal attacks due to stenosis causing a steal phenomenon • Acute coronary syndrome in patients with stenosis proximal to a mammary artery bypass • Caution: nonspecific dizziness • Side-to-side comparison of blood pressures and pulses, and Doppler ultrasound for screening • Diagnosis best confirmed by contrast-enhanced MRA including MRI (for detection of infarction) Although data with a high level of evidence are not currently available for the balloon angioplasty and stenting of proximal supraaortic stenoses, interventional treatment is generally preferred for these lesions because it is effective and much less invasive than operative treatment. Nevertheless, a carotid-subclavian bypass and other vascular surgical reconstructions are still available as alternatives in patients who are difficult to treat by interventional therapy, and these techniques have yielded better long-term patency rates than stenting (AbuRahma et al. 2007). The proximal arterial trunks are elastic vessels that can offer significant resistance to balloon angioplasty when lined by fibrous or calcified plaque. The results of percutaneous transluminal angioplasty alone are often disappointing as a result of elastic recoil forces or intimal dissection. Primary stent placement yields better initial results and 1 -year patency rates of —90%, and has therefore become the preferred option at most centers (Sixt et al. 2009). Balloon-expandable stents approved for use in peripheral vessels are most commonly used. They provide an effective scaffold for rigid plaques and can be accurately deployed at the desired location. Self-expanding stents, which conform better to changing vascular diameter, have also been used in selected cases (Pulido-Duque et al. 2005). Most stenoses can be treated via femoral access. Retrograde recanalization via brachial access may be used for subclavian obstructions that are difficult to negotiate by the transfemoral route. Note Combined procedures involving surgical exposure of the carotid bifurcation and retrograde stent insertion into the common carotid artery are rarely necessary nowadays and are recommended only in exceptional cases, because there are differences in antithrombotic management for surgical and interventional procedures.
Epidemiology and Risk of Stroke
Clinical Presentation and Diagnosis
Interventional Treatment Options
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine