CHAPTER 101 Pulmonary Hemorrhage and Vasculitis
A large number of conditions may result in pulmonary hemorrhage (Table 101-1). Broadly speaking, pulmonary hemorrhage may originate in the airways or lung parenchyma. Airway-related pulmonary hemorrhage is commonly the result of bronchitis, bronchiectasis, or malignancy, whereas parenchymal hemorrhage may result from pulmonary infarction, necrotizing pneumonias, toxic inhalational injury, malignancy, or causes of diffuse alveolar hemorrhage, with or without pulmonary vasculitis.
TABLE 101-1 Differential Diagnosis of Pulmonary Hemorrhage
| Cause | Features |
|---|---|
| Airway | |
| Parenchyma | |
| Diffuse alveolar hemorrhage with capillaritis | |
| Diffuse alveolar hemorrhage without capillaritis | |
| Other | Pulmonary arteriovenous malformation |
DIFFUSE ALVEOLAR HEMORRHAGE
Etiology and Pathophysiology
Diffuse alveolar hemorrhage (DAH) is present when the cause of the hemorrhage primarily affects the alveolar capillary surface. Causes of DAH may be divided into conditions associated with inflammation of the pulmonary capillaries, referred to as capillaritis, and those without capillaritis, so-called bland DAH (see Table 101-1). Pulmonary capillaritis refers to alveolar interstitial inflammation consisting of neutrophil accumulation associated with fibrinoid necrosis, producing injury to the basement membrane and resulting in leaky capillaries. Repeated bouts of inflammation and hemorrhage result in the deposition of hemosiderin-laden macrophages. In patients with bland DAH, red blood cells fill the alveoli in the absence of capillary inflammation. Note that there is occasionally some overlap in this classification system; Goodpasture syndrome, collagen vascular disease, and systemic lupus erythematosus may be associated with pulmonary hemorrhage with or without pulmonary capillaritis. For DAH with capillaritis, autoantibodies directed against the alveolar basement membrane produces direct damage or basement membrane injury results from immune complex deposition.
Imaging Techniques and Findings
CT
CT and high-resolution CT (HRCT) typically show multifocal or diffuse bilateral ground-glass opacity and consolidation. Ground-glass attenuation poorly defined nodules (Fig. 101-1) may occur. Often, a network pattern of smooth interlobular septal thickening is superimposed in the regions of ground-glass opacity.
VASCULITIS
The histopathologic hallmark of vasculitis is the presence of angiocentric inflammation, usually extending through all layers of blood vessel walls. Fibrinoid necrosis and perivascular fibrosis are also commonly present, and may ultimately lead to vascular obliteration and occlusion. Both leukocytoclastic (neutrophil-predominant) and granulomatous (lymphocyte-predominant) vasculitic patterns may occur. Most pulmonary vasculitides share the common pathogenesis of immune complex deposition in the vessel wall, with activation of complement and cellular chemotaxis, leading to an enzymatic and inflammatory cascade that ultimately produces vascular damage. The whole process may be antigen-driven, which may explain the association of a number of vasculitides with viral infections and collagen vascular disorders. However, some granulomatous vasculitides may be the result of cell-mediated immunity rather than immune complex deposition. A number of vasculitides may affect the thorax, the lung in particular. The main histopathologic derangement of vasculitides affecting the lung is capillaritis, perhaps associated with inflammation of slightly larger vessels (Table 101-2).
TABLE 101-2 Common Causes of Pulmonary Vasculitis
| Location | Cause |
|---|---|
| Large vessels (aorta and major branch vessels) | |
| Medium-sized vessels (visceral arteries)*† | |
| Small vessels (arterioles, capillaries, venules, distal intraparenchymal small arteries leading to arterioles) |
* Some overlap in level of involvement may occur, particularly with either large or small vessel vasculitides involving medium-sized vessels.
† Visceral arteries = coronary, hepatic, mesenteric, and renal arteries
WEGENER’S GRANULOMATOSIS
Imaging Techniques and Findings
Radiography
Chest radiographs are abnormal in up to 85% of patients with WG at some point during the course of the illness. The most characteristic imaging manifestation of WG is multiple, usually bilateral, nodules or masses typically measuring 2 to 4 cm, often associated with cavitation (Fig. 101-2). Pulmonary opacities and cavities in patients with WG may occasionally be much larger. WG-related pulmonary cavities often have a rather thick, irregular internal wall, and air-fluid levels are occasionally seen. Ground-glass opacity surrounding the cavities is a frequent finding and is usually caused by adjacent alveolitis or pulmonary hemorrhage.
CT
Thoracic CT scanning in patients with WG also typically shows multiple bilateral nodules and/or masses,1 and is far more sensitive for the detection of cavitation than chest radiography. In fact, most nodules measuring more than 2 cm in patients with WG will show cavitation on CT (Fig. 101-3). Nodules and cavities in patients with WG have no particular zonal predilection, and are somewhat randomly distributed throughout the lungs.
Patchy multifocal or diffuse ground-glass opacities, often with areas of consolidation,1 is the second most common thoracic imaging manifestation of WG, and may occur in the absence of pulmonary nodules. These opacities are usually the result of pulmonary hemorrhage. Occasionally, areas of consolidation may be subpleural or peribronchiolar in distribution, simulating organizing pneumonia; the so-called atoll or reverse halo sign may also be seen (Fig. 101-4).
Tracheobronchial wall thickening and narrowing may be present in patients with WG,1 and may even lead to atelectasis. Typically, airway involvement in patients with WG predominates in the subglottic region and extends a variable distance caudally (Fig. 101-5). The airway wall thickening is circumferential and often nodular and irregular, occasionally resulting in tracheobronchial stenosis. The tracheobronchial thickening may occasionally calcify.
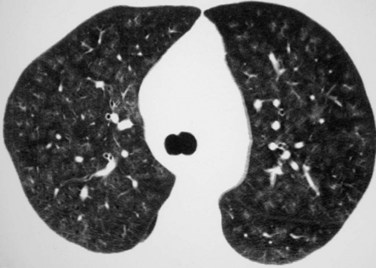
 FIGURE 101-1
FIGURE 101-1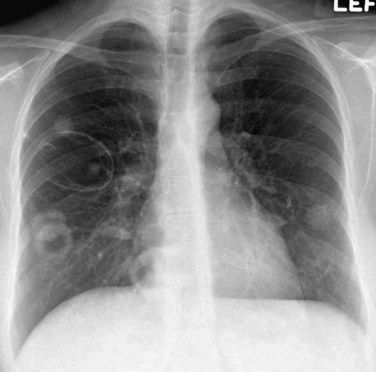
 FIGURE 101-2
FIGURE 101-2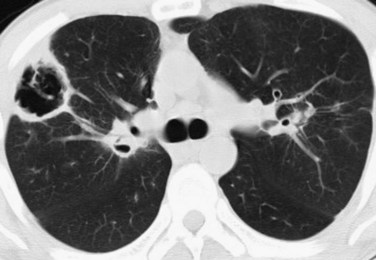
 FIGURE 101-3
FIGURE 101-3
 FIGURE 101-4
FIGURE 101-4
 FIGURE 101-5
FIGURE 101-5


