• An infection developing within the distal airspaces (and adjacent to the visceral pleura) • As the airways are not primarily involved and remain patent there is little or no volume loss gh • An anaerobic, Gram-positive bacterium (Actinomyces israelii): this is a mouth commensal, causing infection when it accesses devitalized tissues (particularly within the cervicofacial region and abdomen) • Chlamydia psittaci: this causes psittacosis (ornithosis) and is usually seen following direct bird contact • A multifocal infection centred within and along the course of the distal airways • Bronchial spread results initially in large heterogeneous scattered opacities • Air bronchograms are usually absent as the disease primarily affects the bronchi (filling them with inflammatory fluid) • This usually affects debilitated hospitalized or institutionalized patients (following aspiration from the upper respiratory tract) • Pleural effusions, empyemas, and cavitation are common • Septicaemic infections (e.g. drug addicts, infective endocarditis): can cause disseminated, poorly marginated and peripheral multifocal nodules which can cavitate • These are usually caused by hospital acquired enterobacteria in debilitated patients (e.g. Proteus, E. coli, Pseudomonas, and Haemophilus) • The lower lobes are predominantly affected with an appearance similar to S. aureus infection • Infection with Mycobacterium tuberculosis (95%)
Pulmonary infection
LOBAR PNEUMONIA
LOBAR PNEUMONIA
DEFINITION
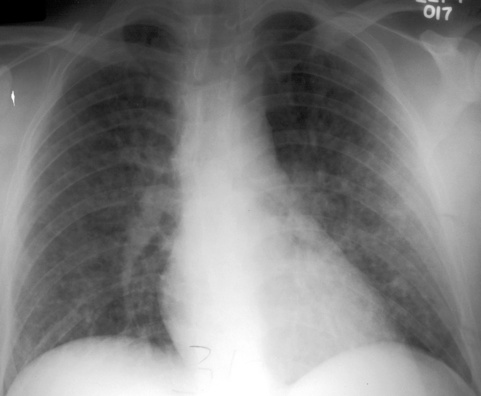
 it spreads via collateral air drift, producing homogeneous opacification of partial or complete lung segments (and occasionally an entire lobe)
it spreads via collateral air drift, producing homogeneous opacification of partial or complete lung segments (and occasionally an entire lobe)  any lung opacification is limited by the fissures and is usually unifocal
any lung opacification is limited by the fissures and is usually unifocal
 there is also associated air bronchogram formation
there is also associated air bronchogram formation
STREPTOCOCCUS PNEUMONIAE (PNEUMOCOCCAL PNEUMONIA)
ACTINOMYCOSIS
 it generates a chronic inflammatory reaction, causing abscess and fistula formation (which contain tiny sulphur granules)
it generates a chronic inflammatory reaction, causing abscess and fistula formation (which contain tiny sulphur granules)
CHLAMYDIAL PNEUMONIA
BRONCHOPNEUMONIA, ANAEROBIC AND ATYPICAL PNEUMONIA
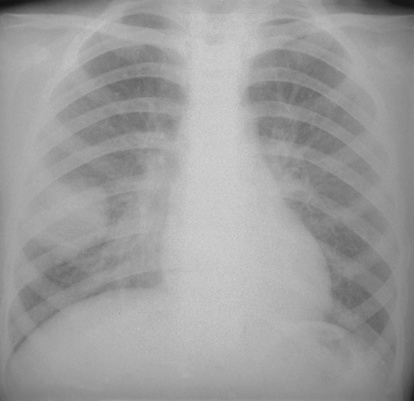
BRONCHOPNEUMONIA
DEFINITION
SPECIFIC INFECTIONS
Staphylococcus aureus
 pneumatoceles may form (particularly in children)
pneumatoceles may form (particularly in children)
Gram-negative pneumonias
 the bacteria are aspirated from a colonized upper respiratory tract
the bacteria are aspirated from a colonized upper respiratory tract
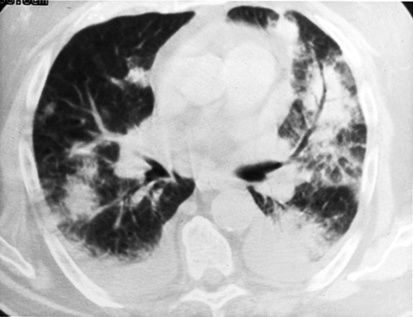
PULMONARY TUBERCULOSIS
PULMONARY TUBERCULOSIS
DEFINITION
 it is acquired via droplet inhalation
it is acquired via droplet inhalation
 Primary TB: this is commonly seen in infants and children if previously unexposed to TB (hypersensitivity is absent)
Primary TB: this is commonly seen in infants and children if previously unexposed to TB (hypersensitivity is absent)  the patient is immunologically able to kill the organism and heals with fibrosis (± calcification)
the patient is immunologically able to kill the organism and heals with fibrosis (± calcification)
 Post-primary TB: if hypersensitivity is present (e.g. due to previous infection or BCG vaccination) a greater inflammatory reaction and caseous necrosis results
Post-primary TB: if hypersensitivity is present (e.g. due to previous infection or BCG vaccination) a greater inflammatory reaction and caseous necrosis results  this is usually due to reactivation of a quiescent lesion (and occasionally due to a new exogenous infection)
this is usually due to reactivation of a quiescent lesion (and occasionally due to a new exogenous infection)
 Progressive primary TB: direct transition from primary to post primary disease
Progressive primary TB: direct transition from primary to post primary disease


 alcoholism
alcoholism  sickle-cell disease
sickle-cell disease  splenectomy
splenectomy it is commonly basal and solitary (but may be multifocal)
it is commonly basal and solitary (but may be multifocal)  the lobar volume is usually unchanged (and rarely increases)
the lobar volume is usually unchanged (and rarely increases)  there is a fairly rapid XR resolution (total resolution usually occurs within 2–6 weeks)
there is a fairly rapid XR resolution (total resolution usually occurs within 2–6 weeks) it can demonstrate a rapid change in size and shape
it can demonstrate a rapid change in size and shape  it may simulate a lung mass
it may simulate a lung mass
 Streptococcus
Streptococcus  pneumococcus
pneumococcus
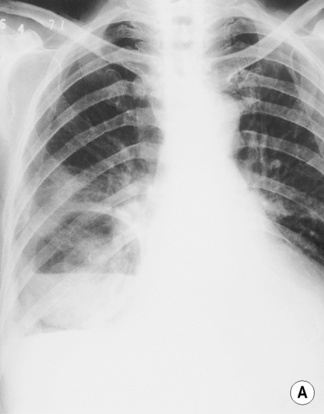
 there is rapid cavitation of any lobar consolidation
there is rapid cavitation of any lobar consolidation there is rapid progression (with up to a 30% mortality rate)
there is rapid progression (with up to a 30% mortality rate)
 COPD
COPD  heart failure
heart failure there is rapid spread of the initial consolidation to the other lobes
there is rapid spread of the initial consolidation to the other lobes  cavitation can be seen in immunocompromised and post renal transplant patients
cavitation can be seen in immunocompromised and post renal transplant patients  pleural effusions are present in 10–35% of cases
pleural effusions are present in 10–35% of cases
 cavitation is common and can mimic the appearance of a bronchogenic carcinoma
cavitation is common and can mimic the appearance of a bronchogenic carcinoma  focal fibrosis (± contraction) may be severe
focal fibrosis (± contraction) may be severe  there are associated pleural effusions, pleural thickening, empyema formation and disease extension into the contiguous soft tissues or bones (the resultant periostitis sets this apart from other infections)
there are associated pleural effusions, pleural thickening, empyema formation and disease extension into the contiguous soft tissues or bones (the resultant periostitis sets this apart from other infections) the initial pulmonary focus may disseminate to other organs (notably the brain)
the initial pulmonary focus may disseminate to other organs (notably the brain) there can be single or multiple pulmonary nodules (which can mimic a primary lung cancer or metastatic disease)
there can be single or multiple pulmonary nodules (which can mimic a primary lung cancer or metastatic disease)  there may be lymphadenopathy and chest wall involvement
there may be lymphadenopathy and chest wall involvement  cavitation and pleural effusions are frequent
cavitation and pleural effusions are frequent there are occasionally enlarged hilar nodes and small effusions
there are occasionally enlarged hilar nodes and small effusions  any radiographic opacities clear slowly
any radiographic opacities clear slowly

 small or moderate pleural effusions (up to 50%)
small or moderate pleural effusions (up to 50%)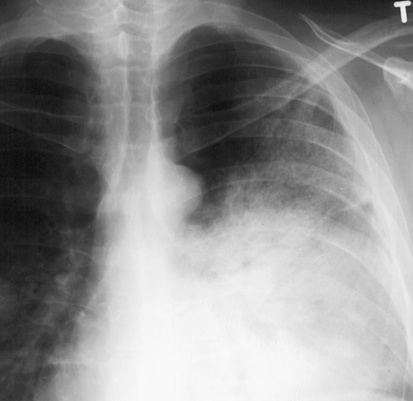


 it is associated with altered consciousness and mechanical ventilation
it is associated with altered consciousness and mechanical ventilation heterogeneous opacities are seen in the dependent lung segments (uni- or bilaterally)
heterogeneous opacities are seen in the dependent lung segments (uni- or bilaterally)  multiple cavities (reflecting severe lung necrosis) may be seen 1–3 weeks following aspiration
multiple cavities (reflecting severe lung necrosis) may be seen 1–3 weeks following aspiration this is a common complication of anaerobic infections (and may occur without any XR evidence of pneumonia)
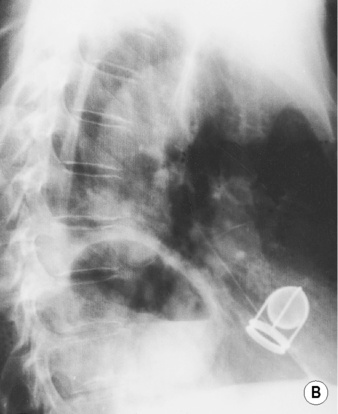
this is a common complication of anaerobic infections (and may occur without any XR evidence of pneumonia) displaced lung and vessels (± gas within the empyema collection)
displaced lung and vessels (± gas within the empyema collection) sheet-like pleural calcification (especially following TB)
sheet-like pleural calcification (especially following TB) it resembles a viral infection with spread from the upper to lower respiratory tract
it resembles a viral infection with spread from the upper to lower respiratory tract  it is usually self-limiting
it is usually self-limiting pleural effusions and nodal enlargement are uncommon
pleural effusions and nodal enlargement are uncommon bronchiolitis with centrilobular nodules
bronchiolitis with centrilobular nodules  bronchovascular thickening (80%)
bronchovascular thickening (80%) they predispose to secondary bacterial infection
they predispose to secondary bacterial infection pleural effusions are rare
pleural effusions are rare  clinical relapse may be due to a secondary bacterial pneumonia
clinical relapse may be due to a secondary bacterial pneumonia nodules
nodules  a ‘tree-in-bud’ appearance
a ‘tree-in-bud’ appearance there is an increased risk with lymphoma, pregnancy and steroid therapy
there is an increased risk with lymphoma, pregnancy and steroid therapy  pulmonary involvement follows a skin rash by 1–6 days
pulmonary involvement follows a skin rash by 1–6 days the nodules usually resolve in 1–2 weeks but can persist for months
the nodules usually resolve in 1–2 weeks but can persist for months  numerous residual small irregular calcified nodules may remain
numerous residual small irregular calcified nodules may remain




 malaise
malaise  fever
fever  night sweats
night sweats  cough (productive with haemoptysis)
cough (productive with haemoptysis)






