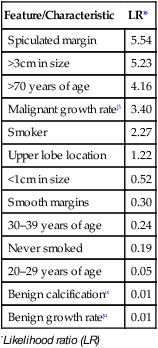
• This is defined as a solitary circumscribed pulmonary opacity with no associated pulmonary, pleural, or mediastinal abnormality • Many are discovered incidentally (but up to 40% may be malignant) • The two primary criteria are the rate of growth (or stability over time) and the attenuation of the nodule – Granular calcification is seen on CT in up to 7% of carcinomas (and can represent either tumour calcification or a granuloma engulfed by tumour) – A mixture of soft tissue and ground-glass attenuation nodules is more likely to be malignant than soft tissue nodules alone Simulants of solitary pulmonary mass* Extrathoracic artefacts Causes of a solitary pulmonary mass* Bronchial carcinoma Radiological features of solitary pulmonary nodules and the likelihood of malignancy *Likelihood ratio (LR) αBenign calcification: diffuse, central, popcorn or concentric µBenign growth rate: a volume doubling time < 1 month or > 2 years (approximately) βMalignant growth rate: a volume doubling time > 1 month or < 2 years (approximately) Adapted from Erasmus et al. Radiographics 2000; 20: 59–66. • SCLC: small (oat) cell carcinoma • NSCLC: non-small cell lung cancer • Risks: tobacco smoke (with a 20–30 fold increased risk) – this has the greatest association with squamous cell carcinomas and the weakest association with bronchoalveolar carcinomas • Asymptomatic (25%): asymptomatic peripheral tumours are more likely to be incidental findings and surgically resectable • Symptomatic: recurrent pneumonia • Paraneoplastic syndromes: inappropriate ADH secretion • Poor prognostic features: hoarseness • The majority are spherical or oval in shape • Ground-glass attenuation is associated with a higher risk of malignancy (and commonly seen with bronchoalveolar carcinoma) • This does not preclude surgical resection (although it adversely affects the prognosis) • CT: assessment is unreliable (with local chest wall pain remaining the most specific indicator) • MRI: this is better than CT in selected cases • Transthoracic ultrasound: this is an accurate technique • 99mTc radionuclide skeletal scintigraphy: this is sensitive (and may detect bone invasion before plain radiography) • CT/MRI indicators: visible tumour deep within the mediastinal fat (mediastinal contact alone is not enough to diagnose invasion) • Criteria for resectability: < 3cm of contact with the mediastinum • Irresectability: tumours obliterating fat planes or showing greater contact than that described above
Pulmonary neoplasms
EVALUATION OF THE SOLITARY PULMONARY NODULE
EVALUATION OF THE SOLITARY PULMONARY NODULE
DEFINITION
 it measures < 3cm in diameter
it measures < 3cm in diameter
DIFFERENTIATION BETWEEN BENIGN AND MALIGNANT MASSES
 the patient’s age is also a significant distinguishing feature (a carcinoma is only seen in < 1% of patients < 35 years old)
the patient’s age is also a significant distinguishing feature (a carcinoma is only seen in < 1% of patients < 35 years old)
 Rate of growth/stability over time: benign lesions invariably have a doubling time of < 1 month or > 18 months (bronchoalveolar carcinomas are an exception in that they may have very slow growth rates)
Rate of growth/stability over time: benign lesions invariably have a doubling time of < 1 month or > 18 months (bronchoalveolar carcinomas are an exception in that they may have very slow growth rates)  bronchial carcinomas usually have a doubling time of between 1 and 18 months
bronchial carcinomas usually have a doubling time of between 1 and 18 months
 Attenuation/enhancement: a dense central nidus or laminated calcification indicates a granulomatous process (e.g. tuberculosis, histoplasmosis)
Attenuation/enhancement: a dense central nidus or laminated calcification indicates a granulomatous process (e.g. tuberculosis, histoplasmosis)  irregular ‘popcorn’ calcification suggests a hamartoma
irregular ‘popcorn’ calcification suggests a hamartoma  fat is virtually diagnostic of a hamartoma
fat is virtually diagnostic of a hamartoma  a lack of enhancement (<15HU) following IV contrast medium is indicative of benignity
a lack of enhancement (<15HU) following IV contrast medium is indicative of benignity
 Size: this is of little diagnostic value
Size: this is of little diagnostic value
 Margins: a well-defined mass with a smooth pencil sharp margin is likely to be benign
Margins: a well-defined mass with a smooth pencil sharp margin is likely to be benign  carcinomas typically have ill-defined margins which are irregular, spiculated, or lobulated and may exhibit umbilication or a notch – unfortunately all these features can be seen with benign disease
carcinomas typically have ill-defined margins which are irregular, spiculated, or lobulated and may exhibit umbilication or a notch – unfortunately all these features can be seen with benign disease
Cutaneous masses
Bony lesions
Pleural tumours of plaques
Encysted pleural fluid
Pulmonary vessel
Bronchial carcinoid
Granuloma
Hamartoma
Metastasis
Chronic pneumonia or abscess
Hytadid cyst
Pulmonary haematoma
Bronchocele
Fungus ball
Massive fibrosis in coal workers
Bronchogenic cyst
Sequestration
Atriovenous malformation
Pulmonary infarct
Round atelectasis
Feature/Characteristic
LR*
Spiculated margin
5.54
>3cm in size
5.23
>70 years of age
4.16
Malignant growth rateβ
3.40
Smoker
2.27
Upper lobe location
1.22
<1cm in size
0.52
Smooth margins
0.30
30–39 years of age
0.24
Never smoked
0.19
20–29 years of age
0.05
Benign calcificationα
0.01
Benign growth rateµ
0.01
LUNG CANCER: RADIOLOGICAL FEATURES
LUNG CANCER: RADIOLOGICAL FEATURES
DEFINITION
 This originates from submucosal neuroendocrine cells
This originates from submucosal neuroendocrine cells  it rapidly spreads haematogenously and to the lymph nodes
it rapidly spreads haematogenously and to the lymph nodes  it behaves as a systemic disease and is usually disseminated at presentation
it behaves as a systemic disease and is usually disseminated at presentation
 Squamous cell carcinomas: arises from the proximal airway epithelium
Squamous cell carcinomas: arises from the proximal airway epithelium
 Large cell carcinomas: atypical cells that appear ‘large’ under the microscope
Large cell carcinomas: atypical cells that appear ‘large’ under the microscope
 Adenocarcinomas: arising from the bronchial glands
Adenocarcinomas: arising from the bronchial glands
 Bronchoalveolar carcinoma: an adenocarcinoma subtype arising from the alveoli and adjacent small airways (probably from type II pneumocytes)
Bronchoalveolar carcinoma: an adenocarcinoma subtype arising from the alveoli and adjacent small airways (probably from type II pneumocytes)  it presents as peripheral pulmonary opacities
it presents as peripheral pulmonary opacities
 asbestos exposure, interstitial pulmonary fibrosis and radiotherapy are additional risks
asbestos exposure, interstitial pulmonary fibrosis and radiotherapy are additional risks
CLINICAL PRESENTATION
 cough
cough  wheeze
wheeze  haemoptysis
haemoptysis
 Cushing’s syndrome (ACTH)
Cushing’s syndrome (ACTH)  carcinoid syndrome
carcinoid syndrome  hypercalcaemia (PTH)
hypercalcaemia (PTH)
 chest pain
chest pain  brachial plexus neuropathy or Horner’s syndrome (due to a Pancoast’s tumour)
brachial plexus neuropathy or Horner’s syndrome (due to a Pancoast’s tumour)  SVC obstruction
SVC obstruction  dysphagia
dysphagia
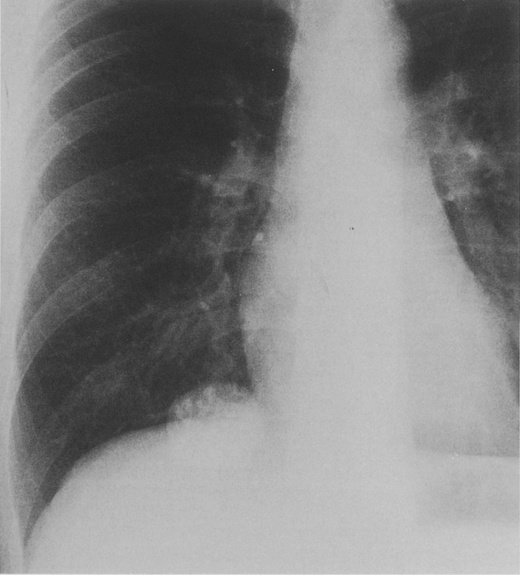
RADIOLOGICAL FEATURES
Peripheral tumours
 lobulated masses can occur due to uneven growth rates
lobulated masses can occur due to uneven growth rates  there may be a ‘corona radiata’ due to numerous fine strands radiating into the lung
there may be a ‘corona radiata’ due to numerous fine strands radiating into the lung  a bronchocele or mucoid impaction can be seen distal to an obstructing carcinoma
a bronchocele or mucoid impaction can be seen distal to an obstructing carcinoma  collapse and consolidation is less commonly seen than with central tumours
collapse and consolidation is less commonly seen than with central tumours
 Cavitation with irregular thick walls ± fluid levels (particularly squamous tumours)
Cavitation with irregular thick walls ± fluid levels (particularly squamous tumours)
 Calcification is rare (6–10%) and may represent engulfed granulomatous disease
Calcification is rare (6–10%) and may represent engulfed granulomatous disease
 Air bronchograms are rare but can be seen with bronchoalveolar carcinoma and adenocarcinoma
Air bronchograms are rare but can be seen with bronchoalveolar carcinoma and adenocarcinoma
Chest wall invasion (T3)
 contact with or a thickened pleura does not necessarily indicate invasion
contact with or a thickened pleura does not necessarily indicate invasion  a clear extrapleural fat plane is helpful but not definitive
a clear extrapleural fat plane is helpful but not definitive  reliable signs include clear-cut bone destruction or a large soft tissue mass
reliable signs include clear-cut bone destruction or a large soft tissue mass
 it is the optimal modality for demonstrating the extent of a superior sulcus tumour
it is the optimal modality for demonstrating the extent of a superior sulcus tumour
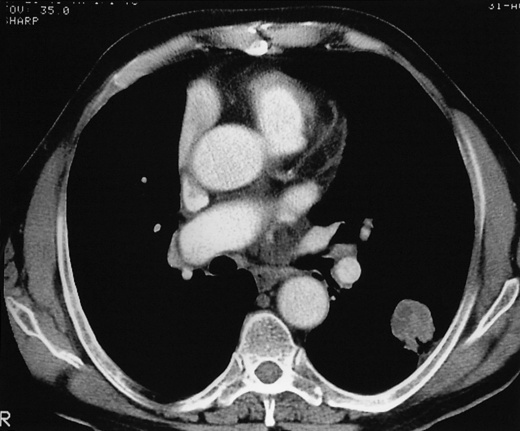
Mediastinal invasion (T4)
 encasement of the mediastinal vessels, oesophagus, or proximal mainstem bronchi
encasement of the mediastinal vessels, oesophagus, or proximal mainstem bronchi  SVC obstruction
SVC obstruction  an elevated hemidiaphragm (indicating phrenic nerve involvement)
an elevated hemidiaphragm (indicating phrenic nerve involvement)
 < 90° of circumferential contact with the aorta
< 90° of circumferential contact with the aorta  a visible mediastinal fat plane between the mass and any vital mediastinal structure
a visible mediastinal fat plane between the mass and any vital mediastinal structure
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 a positive result is 97% sensitive and 82% specific for malignancy
a positive result is 97% sensitive and 82% specific for malignancy it can also occur if the nodule is due to a carcinoid tumour or a slow-growing broncho-alveolar carcinoma
it can also occur if the nodule is due to a carcinoid tumour or a slow-growing broncho-alveolar carcinoma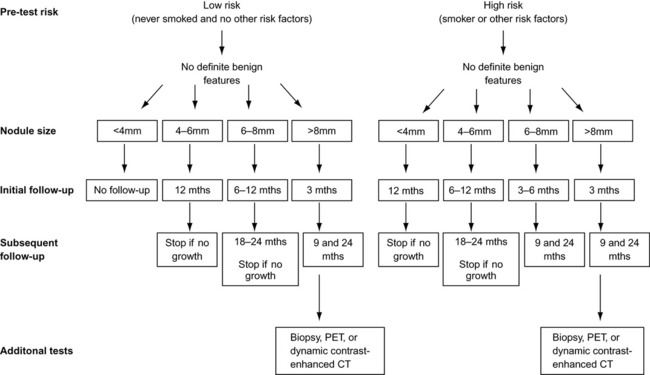
 a likelihood ratio < 1.0 typically indicates a benign lesion
a likelihood ratio < 1.0 typically indicates a benign lesion  a likelihood ratio > 1.0 typically indicates a malignant lesion
a likelihood ratio > 1.0 typically indicates a malignant lesion any peripheral collapsed lung will enhance more than a central tumour
any peripheral collapsed lung will enhance more than a central tumour  collateral air drift may prevent some post-obstructive changes
collateral air drift may prevent some post-obstructive changes
 extensive hilar and mediastinal lymphadenopathy is typical of small cell tumours
extensive hilar and mediastinal lymphadenopathy is typical of small cell tumours haematogenous osteolytic bone metastases
haematogenous osteolytic bone metastases  hypertrophic osteoarthopathy
hypertrophic osteoarthopathy






