Pyomyositis is the primary infection of the skeletal muscle. It is common in the tropics, but is increasingly being reported worldwide. It can affect immunocompromised and immunocompetent individuals. Staphylococcus aureus is the most common causative organism. Muscle histology and its culture remain the gold standard for diagnosis. However, among noninvasive methods, MR imaging is highly sensitive and can image large areas of the body and detect subclinical involvement. Early diagnosis, institution of appropriate antibiotic therapy, and drainage of pus lead to favorable outcome.
- •
Pyomyositis is the primary infection of the skeletal muscle/s.
- •
It is more common in tropical countries, but is increasingly being reported worldwide.
- •
It can affect immunocompromised and immunocompetent individuals.
- •
Staphylococcus aureus is the most common causative organism.
- •
Ultrasound is a simple, readily available, good technique for diagnosis, but it may miss early lesions.
- •
MR imaging is the preferred imaging technique for detection.
- •
MR imaging is highly sensitive, can image large areas of the body, and detect subclinical involvement. It has the added advantage of detecting adjacent bone and joint involvement and excluding other soft tissue disorders, such as tumors and lymphedema.
Pyomyositis (also known as tropical myositis , temperate myositis , pyogenic myositis , suppurative myositis , myositis purulenta tropica , and epidemic abscess ) is a primary infection of skeletal muscle and often associated with abscess formation. Intermuscular abscesses, abscesses extending into muscles from adjoining tissues such as bone or subcutaneous tissues, and those secondary to previous septicemia are not classified as pyomyositis.
In the 1800s, both Virchow and Osler reported cases of “diffuse purulent infiltration of the muscles”; however, the first detailed description of pyomyositis is attributed to Scriba in 1885. Pyomyositis was entirely thought to be confined to tropical areas predominantly affecting young and healthy populations. Levin and colleagues described a case in the United States for the first time in 1971. Since then increasingly more cases are being described from temperate areas where the incidence seems to mirror the increase in the number of immunocompromised persons, particularly those with HIV infection, diabetes, organ transplantation, malignancies, chemotherapy, and rheumatologic diseases (temperate pyomyositis). These immunosuppressed states account for three-fourths of cases in temperate areas, with HIV being responsible for nearly a quarter of all these cases. Because of these differences, tropical and temperate pyomyositis were considered separate entities, but this distinction is more or less superficial, and therefore suggestions were made to rename this entity more appropriately as pyomyositis (which we will be used in this article), infectious myositis , or spontaneous bacterial myositis.
Prevalence
Exact prevalence and incidence rates are not known because of the lack of epidemiologic studies. Information in the literature is restricted to case reports and case series from individual hospitals or Medline searches. Studies from Africa estimate that pyomyositis is responsible for 1% to 4% of all hospital admissions in tropical countries. A Medline database search in the United States from 1981 to 2002 revealed 84 cases of pyomyositis in people infected with HIV, 119 in those who had non-HIV underlying immunosuppressive states, and 127 in normal healthy individuals. Unnikrishnan and colleagues reported 13 cases of pyomyositis in children younger than 16 years from a large tertiary orthopedic center in the United Kingdom between 1998 and 2007. A study from Australia estimates annual incidence of 0.5 cases per 100 000 person-years. In a retrospective analysis conducted by Tanir and colleagues, among 242 patients who were hospitalized with a soft tissue diagnosis, pyomyositis accounted for 6 (2.5%) cases.
Etiology
Staphylococcus aureus is the causative organism in up to 90% of cases from tropical areas and 75% from temperate areas, detected in either blood cultures or surgical specimens. A recent spurt has occurred in community-acquired, methicillin-resistant Staphylococcus aureus (MRSA) causing pyomyositis. The second most common type of bacteria implicated in causing pyomyositis is group A streptococci. Streptococci (groups B, C, and G), Pneumococcus , Neisseria , Haemophilus , Aeromonas , Pseudomonas , Klebsiella , and Escherichia have also been implicated, albeit uncommonly. Mycobacteria ( M avium complex, M Tuberculosis , and M haemophilium) , fungi ( Blastomycosis, Cryptococcus neoformans , Aspergillus, Candida, Fusarium, Pneumocystis Jiroveci) , and anaerobes ( Salmonella , Vibrio, Enterococci, Capnocytophaga sputigena, Stenotrophomonas maltophilia , and Burkholderia cenocepacia ) remain subjects of anecdotal case reports. Chiu and colleagues reported a higher incidence of gram-negative bacterial pyomyositis in patients with underlying diseases. Crum had similar findings in a retrospective analysis from the United States. However, Staphylococcus , Bartonella , and Salmonella species were the causative agents most commonly isolated with the diagnosis in patients with HIV.
Etiology
Staphylococcus aureus is the causative organism in up to 90% of cases from tropical areas and 75% from temperate areas, detected in either blood cultures or surgical specimens. A recent spurt has occurred in community-acquired, methicillin-resistant Staphylococcus aureus (MRSA) causing pyomyositis. The second most common type of bacteria implicated in causing pyomyositis is group A streptococci. Streptococci (groups B, C, and G), Pneumococcus , Neisseria , Haemophilus , Aeromonas , Pseudomonas , Klebsiella , and Escherichia have also been implicated, albeit uncommonly. Mycobacteria ( M avium complex, M Tuberculosis , and M haemophilium) , fungi ( Blastomycosis, Cryptococcus neoformans , Aspergillus, Candida, Fusarium, Pneumocystis Jiroveci) , and anaerobes ( Salmonella , Vibrio, Enterococci, Capnocytophaga sputigena, Stenotrophomonas maltophilia , and Burkholderia cenocepacia ) remain subjects of anecdotal case reports. Chiu and colleagues reported a higher incidence of gram-negative bacterial pyomyositis in patients with underlying diseases. Crum had similar findings in a retrospective analysis from the United States. However, Staphylococcus , Bartonella , and Salmonella species were the causative agents most commonly isolated with the diagnosis in patients with HIV.
Pathogenesis
The exact pathogenesis is currently poorly understood, causing tropical pyomyositis to be difficult to differentiate from temperate pyomyositis. Factors such as preceding viral and protozoal infections and nutritional deficiencies have been proposed, but evidence in this regard is sketchy. The pathogenesis involves the presence of transient bacteremia in a setting of muscle injury.
Skeletal muscles are intrinsically very resistant to infections. In 1904, investigators showed that pyomyositis could only occur in S aureus– inoculated animal muscles that had been initially traumatized by electric shock, pinching, or ischemia. Even direct inoculation of staphylococcus in skeletal muscles failed to produce an abscess. More evidence comes from the fact that pyomyositis was seen is fewer than 1% cases of fatal Staphylococcal septicemia.
In addition to blunt trauma, muscular injuries from overuse may be a risk factor for the development of pyomyositis. Cases of pyomyositis have been documented in young healthy individuals after vigorous exercises concurrent with asymptomatic episodes of bacteremia possibly from skin abrasions. In 20% to 50% of cases, patients had a history of blunt trauma or rigorous exercise. The most plausible explanation seems to be that sequestered iron is released from myoglobin in traumatized muscles. This released iron provides a nutrient that is essential for rapid growth and proliferation of organisms in an appropriate circumstance (transient bacteremia), hence leading to the development of pyomyositis. In addition, formation of small hematomas around the site may provide a favorable site for the binding of staphylococci and other bacteria, and the surrounding damaged and devitalized tissue might also impede the host immune response.
Conflicting studies by Bickels and colleagues and Scharschmidt and colleagues have added more to the already prevalent confusion. In their review of 676 patients, Bickels and colleagues reported trauma in fewer than 5% of cases, thereby ruling out muscle trauma as a prerequisite for myositis. This observation was also supported by Scharschmidt and colleagues. Furthermore, in 11 cases of pyomyositis from Australia, none had history of antecedent muscle trauma. Therefore, given the infrequency of pyomyositis compared with the number of athletic events, muscle injury may have some role, but evidence is still inconclusive.
Other mechanisms postulated, though not fully substantiated, include lack of immunity against staphylococcus, as evidenced by defective T-lymphocyte responses. Patients with HIV have an increased incidence of pyomyositis compared with the general population. The reasons could be multifactorial (higher colonization rates with S aureus , neutropenia, defective immune responses, use of intravenous lines, direct damage to the muscle [HIV myopathy],or reactions to antiretroviral medications, such as mitochondrial myopathy associated with zidovudine).
Histopathology
Microscopically, patchy myocytolysis with inflammatory infiltrate is seen, with areas of complete disintegration and edematous separation of muscle fibers with interfiber infiltration. The process is not diffuse, and is followed by either a reparative process or complete degeneration with suppuration. The pathologic hallmark of pyomyositis is myositis without abscess in biopsied muscle specimens.
Clinical features
Pyomyositis is seen more commonly in young men, with a male-to-female ratio of 1.5:1. No age group is immune, and increasingly more cases are being reported in pediatric age groups. Falesi and colleagues reported pyomyositis in a neonate. Commonly, a single muscle is affected, but involvement of multiple muscles is not unusual (12%–40% of cases). Although the most common site of pyomyositis is the thigh, it commonly affects other bulky muscles, such as the gastrocnemius, glutei, pectorals, and biceps, with a propensity for lower limbs. Involvement of the muscles of forearm, abdominal wall, sternocleidomastoid, intercostals muscles, paraspinal, and pelvic muscles, and even extraocular muscles, has been anecdotally reported.
The evolution of myositis can be clinically divided into three discrete stages.
Invasive Stage
The invasive stage is subacute, occurring over 1 to 3 weeks, and characterized by local painful swelling with a wooden consistency with or without erythema (because infection is deep-seated). Fever and leukocytosis are invariably present. Aspiration at this stage will not yield pus because the bacterial seeding has just begun and purulent collection has not developed. This stage may resolve, remaining undiagnosed in most patients, or can progress to the next stage. It is often overlooked, and differentials vary from hematoma to thrombosis to osteomyelitis.
Suppurative Stage
The suppurative stage is the one at which the diagnosis of pyomyositis is usually established. High spiky swinging temperatures herald the onset, which usually occurs between the second and third weeks. The area is extremely painful and tender. An abscess is seen on imaging studies. Aspiration, if attempted at this stage, will yield pus. However, because the infection is deep-seated, classical characteristics of abscess, such as erythema and fluctuation, are generally absent. The presence of regional lymphadenopathy suggests an alternative diagnosis.
Late Stage
If the suppurative stage remains undiagnosed and untreated, the infection disseminates, leading to multiple abscesses, septicemia, septic shock, and multiorgan system failure, marking the late stage.
Differential Diagnosis
Pyomyositis may have myriad presentations besides the typical one (only local symptoms, only fever and leukocytosis, acute fever with chills, pyrexia of unknown origin [in absence of local symptoms], compartment and compression syndromes, and septic shock). A review of the literature showed that the diagnosis of pyomyositis has been missed; for instance, pyomyositis of iliopsoas muscle presented like appendicitis. Likewise, septic arthritis of the hip, epidural abscess or sciatica, osteomyelitis, and inflammatory myositis have been erroneously diagnosed in the presence of pyomyositis.
Therefore, lest the diagnosis be missed, resulting in adverse outcomes for a potential treatable entity, physicians in all spheres must maintain a high degree of vigil for this entity. Other conditions, such as deep vein thrombosis, cellulitis, muscle contusion, muscle hematoma, muscle or tendon rupture, septic arthritis, osteomyelitis, osteosarcoma, polymyositis, spontaneous gangrenous myositis trichinosis, cysticercus cellulose, and leptospirosis, may often have similar presentations to pyomyositis, especially in the invasive stage, often leading to a diagnostic dilemma.
Diagnosis
Early diagnosis is the key to success but is commonly missed. The reasons include lack of awareness, nonspecific features in the invasive stage, atypical manifestations, and a wide range of differential diagnoses.
Leukocytosis is variable, especially in the invasive stage, but a shift to left occurs with suppurative stage leukocytosis. Half of the HIV-positive patients will not have leukocytosis. Keeping up with inflammation, inflammatory markers such as erythrocyte sedimentation rate and C-reactive protein are also elevated but are nonspecific. Some clues can be obtained from blood tests; for instance, the presence of eosinophilia suggests parasitic infection, and deranged liver and renal functions favor the diagnosis of leptospirosis. Muscle enzymes such as creatinine kinase and aldolase are not raised despite evidence of muscle inflammation and destruction.
Blood cultures are sterile in approximately 90% of patients from tropical areas and up to 70% patients from temperate regions. Even if positive, blood cultures support the diagnosis in an appropriate clinical setting but are not diagnostic for pyomyositis. Poor yield in blood cultures may occur because bacteremia is usually transient in pyomyositis. Better yields are from temperate countries, probably because of better microbiological techniques. Despite the poor yield, blood cultures should be taken to test for aerobic and anaerobic bacteria, mycobacteria, and fungi, especially in immunocompromised patients.
Aspiration and culture of the pus remains the standard diagnostic method, but in the early stages minimal or no suppuration occurs, and therefore pus may not be aspirated. Pus cultures may not yield any organism in up to 30% of cases.
Muscle biopsy with culture of tissue remains the gold standard. In addition to confirming the diagnosis of pyomyositis, other diagnosis such as polymyositis, osteosarcoma, and intermuscular abscesses can be confidently excluded.
Imaging
Noninvasive radiologic methods, such as ultrasound, CT, or MR imaging, are useful in confirming the diagnosis and monitoring patients during follow-up. Plain radiographs are not sensitive, but in a few cases may suggest muscle enlargement, loss of muscle definition, obliteration of deep fat planes, gas in soft tissues, and reactive changes in adjacent bone. Plain radiographs are more useful in excluding other processes, such as osteomyelitis or bone tumor.
Ultrasound remains the preferred initial screening tool because it is easily available and cost-effective. It shows hypoechoic areas with increased muscle bulk, but the early invasive stage may be missed. CT can visualize pyomyositis as areas of low attenuation with loss of muscle plain surrounded by a rim of contrast enhancement, but it cannot differentiate abscess from swollen muscles.
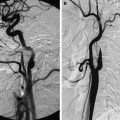
MR imaging is more specific and sensitive compared with CT. It usually presents as ill-defined muscle enlargement with hyperintensity on T2-weighted images, which may be associated with swelling of fascial planes, abnormal signal intensity of the nearby bone, or fluid in the joint. Reactive bone edema is difficult to differentiate from osteomyelitis even after contrast study. Occasionally, fluid collection within the muscle may be visible as hyperintense on T2-weighted images and isointense to hypointense on T1-weighted images ( Figs. 1 and 2 ). Postcontrast T1-weighted imaging study shows rim enhancement, suggesting an abscess along with uniform enhancement of the involved muscles. Diffusion-weighted imaging (DWI) has been reported to help in differentiating abscess from tumor in various body locations; however, its role in pyomyositis is unknown. DWI shows a hyperintense signal from the involved muscles, which shows a hypointense signal on an apparent diffusion coefficient trace and is referred to as restriction of diffusion (see Figs. 1 and 2 ), similar to the description of the abscess anywhere else in the remainder of the organs. The authors routinely use DWI as part of their imaging protocol in suspected cases of pyomyositis, and have found it to be extremely useful. Moreover, because the disease process may be patchy and widespread at times, MR imaging may have an additional advantage of showing the exact extent of the disease noninvasively, and is useful in monitoring the response to therapy. MR imaging is also useful in detecting pyomyositis in the pelvic region and ruling out other pathologies effectively. Gallium scintigraphy may also help to localize inflammation, but it is nonspecific and expensive.