Viral infections of the central nervous system in the tropical countries of Asia and the Indian subcontinent are different from those of the Western and developed world. Many of the endemic and epidemic encephalitides that are prevalent in these regions, such as Japanese encephalitis, have characteristic findings on imaging, especially on magnetic resonance imaging, allowing a rapid diagnosis and differentiation from clinically similar syndromes. Other emerging viral infections in the region in recent years have posed new challenges. The contribution of neuroimaging to the management of these emerging infections is also discussed.
Viral infections of the central nervous system (CNS) in humans are uncommon, not because viruses lack neuroinvasive potential, but because access to the CNS is prevented by various factors such as anatomic barriers and virus-specific and nonspecific host immunity. When they do invade the CNS, viruses have the potential to cause infections of any part of the CNS, namely the meninges, brain, or spinal cord, in combination or in isolation, many which have devastating consequences.
Although viruses with CNS-invading potential belong to all families of viruses, those that cause CNS infections in the tropics are different from those of nontropical regions, because of different geographic environments, different insect and animal vectors, frequently compounded by inadequate health care and sanitation facilities in many tropical countries. Ecologic changes of tropical habitats have led to CNS diseases due to emerging viruses in recent times. In an appropriate clinical setting, imaging can often help in establishing possible viral causes of a CNS disease and at times suggest the specific etiologic virus. Imaging becomes more relevant in epidemic encephalitis, where most often the viral cause can be suggested and differentiated from other causes of intracranial infection. As with all CNS infections, magnetic resonance (MR) imaging, with its superior contrast resolution, is preferred to computed tomography (CT) and should be the imaging modality of choice in viral infections of the CNS. This article discusses common causes of viral infections of CNS in the tropics, especially in relation to Asia and the Indian subcontinent, and how imaging can help in the management of these diseases.
Viral meningitis
Acute viral meningitis is usually a self-limited disease leading to complete recovery. Enteroviruses (Coxsackie and echoviruses) account for more than half of all cases. Other viruses that may also cause meningitis include mumps, herpes simplex viruses (HSV), and flaviviruses. Enterovirus meningitis may occur in sporadic or epidemic forms and epidemics have been reported from India. However, the etiologic profile of viral meningitides in the Indian subcontinent is largely unknown because the etiologic diagnosis of aseptic meningitis is rarely attempted due to costs, lack of infrastructure, and the self-limiting nature of the disease. One study from China showed meningeal enhancement in MR imaging in 9 out of 23 patients of viral meningitis, whereas CT showed no abnormalities. However, a normal imaging study does not exclude viral meningitis, because both contrast-enhanced MR imaging and fluid-attenuated inversion-recovery (FLAIR) sequences may fail to show any abnormalities.
Viral encephalitis
Encephalitis is the term used to refer to an infection of the brain, most commonly caused by viruses. Viral encephalitis most commonly presents as an acute illness with fever and altered sensorium with or without focal neurologic deficits. The term acute viral encephalitis or meningoencephalitis is then used; the latter term is used because most viral infections of the brain are accompanied by involvement of the meninges, causing associated aseptic meningitis. Less commonly, viral encephalitis presents as a slower indolent disease process referred to as slow viral infections. In addition, an encephalitic condition that is caused by alteration of immune function in response to a viral illness (acute disseminated encephalomyelitis [ADEM]) needs to be differentiated from acute viral encephalitis in the light of different management for the former condition. This article is limited to acute encephalitides that commonly occur in Asia and the Indian subcontinent, especially those that are endemic to the region and those that are caused by emerging viruses with distinct threat potential. Slow viral infection caused by measles is also discussed because this is a significant problem in Asia and the Indian subcontinent.
The annual incidence of acute encephalitis in the tropics is similar to that in the West, as recent meta-analytical data have shown. In the tropical and Western settings, the annual incidence of encephalitis is 6.34 and 7.4 per 100,000 respectively.
Pathologically, all encephalitides are accompanied by varying degrees of cell necrosis (neuronophagia) and inflammatory changes accompanied by edema. Both areas of cell necrosis and edema are reflected on imaging, especially MR imaging. Variable degrees of inflammation and edema in different encephalitides lead to variability in the diffusion characteristics of the inflamed tissue. For example, in herpes simplex encephalitis (HSE), restriction of diffusion on MR imaging is more marked than in Japanese encephalitis (JE), because the former is a more necrotizing inflammatory disease than the latter. The presence of virus-specific receptors in the cells of the CNS determines susceptibility of the cell to an invading virus. For example, poliovirus invades the anterior horn cells, binding to the CD155 receptor protein. This property lends some specificity to imaging of viral encephalitides. Late sequelae of encephalitis include focal or diffuse atrophy, shrinkage of white matter, and healing of encephalitic and edematous areas by glial reaction. These delayed changes can also be seen on imaging, with residual gliotic lesions of encephalitis tending to be located in the initial areas of involvement. Thus, JE residua may be detected in the thalami, substantia nigra, or basal ganglia.
JE
JE is the most important arboviral encephalitis in the world in terms of incidence, mortality, and morbidity, with more than 50,000 new cases and about 15,000 deaths occurring annually. JE is a mosquito-borne flaviviral encephalitis and is transmitted to man by culicine mosquitoes. It is a zoonosis and the basic cycles of transmission involve the mosquito, pig, and ardeid water birds, with man acting as an incidental dead-end host. Water birds such as herons, egrets, and other ardeid birds are the most important hosts for maintenance of JE virus (JEV), whereas pigs are the most important reservoir and amplifier of the disease. Man-to-man transmission does not occur because viremia in man is low and transient. The geographic area of JE prevalence has been increasing in the past 70 years. Since the first epidemic in Japan in the 1930s, the disease has now become prevalent across several tropical and temperate regions in countries in southern, southeastern, and eastern Asia, the Pacific rim, and recently in the Torres Straits of northern Australia and the Australian mainland. In developed Asian countries such as Japan, Taiwan, and South Korea, JE incidence has dropped considerably as a result of concerted immunization efforts, vector control, improved agricultural practices and animal husbandry, and overall improvement in sanitation. In India, JE is a major public health problem with approximately 2000 to 7000 new cases occurring annually across several Indian states involving almost the entire country. Currently, there are more than 10,000 cases being reported annually from China. JE is mostly a disease of children and young adults in endemic areas. In northern Thailand, the annual incidence of JE is estimated to be 40 per 100,000 for ages 5 to 25 years, declining to almost 0 after the age of 35 years. When epidemics first occur in new locations such as north and northeastern India, Nepal, and Sri Lanka, adults are also affected. Nonimmune travelers to endemic areas may be particularly susceptible to the disease. There are 2 recognized epidemiologic patterns of JE. In the northern areas such as northern Vietnam, northern Thailand, Korea, Japan, Taiwan, China, Nepal, and northern and northeastern India, large epidemics occur during the summer months. In southern areas such as southern Vietnam, southern Thailand, Indonesia, Malaysia, Philippines, Sri Lanka, and southern India, JE tends to be endemic, with peak cases appearing after the start of the rainy season. This variation seems to be related to the temperature rather than the amount of rainfall or different strains of the virus.
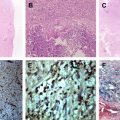
After the JEV gains entry through the bite of the mosquito, the virus multiplies locally and in regional lymph nodes. After a period of brief viremia, the virus enters the CNS through the vascular route. Subsequent spread of the virus possibly occurs along the dendrites and axonal processes. The pathologic changes of the brain in fatal cases of JE include vascular congestion, cerebral edema, and brain swelling. Histologically, the leptomeninges show variable degrees of mononuclear inflammation extending along the Virchow-Robin spaces into the brain parenchyma, with formation of perivascular cuffs. Two types of lesions are characteristic microscopically within the brain. The first type of lesion is the cell-rich gliomesenchymal nodule. These lesions are formed by aggregates of microglial cells and lymphocytes around degenerating neurons. They are invariably seen in the medulla. They are also seen in the thalamus, substantia nigra, pontine, and reticular nuclei of brainstem, cerebral cortex, dentate nuclei, and Purkinje cells of the cerebellum. They have also been described in the Ammon’s horn of the hippocampus. The second type of lesion is the cell-poor necrolytic lesion seen in the cerebral cortex, thalami, corpus striatum, midbrain, and pons. They are uncommon in the medulla oblongata.
JEV infections are mostly asymptomatic and the ratio of clinically apparent to asymptomatic infections may vary from 1:25 to 1:1000. The incubation period of JEV varies from 5 to 15 days. The course of the disease is divided into 3 stages: (1) a prodromal phase preceding CNS features, (2) an encephalitic phase of CNS symptoms, and (3) a late stage in which there is recovery or residual neurologic deficit. Some atypical presentations such as febrile seizures, aseptic meningitis, and acute flaccid paralysis have been described.
The laboratory diagnosis of JE is established by showing (1) a fourfold increase in serum antibody titer, (2) virus isolation, or (3) specific immunoglobulin M (IgM) antibody detection by enzyme immunoassay capture in cerebrospinal fluid (CSF) or serum (Mac-ELISA). The first 2 methods take time and the Mac-ELISA method has the advantage of providing the diagnosis with a single test. However, this test may be positive in CSF in only 50% of patients in the first week of the disease, although it is invariably positive beyond the first week.
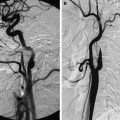
The imaging findings of JE reflect the pathologic changes of the brain. The typical imaging findings are lesions in the thalami, substantia nigra, basal ganglia, and hippocampi ( Fig. 1 ). Less commonly, lesions can also be found in the cerebral cortex, midbrain, pons, medulla, cerebellum, and white matter. MR imaging has been reported to be more sensitive than CT scan by several investigators and is the imaging investigation of choice. Thalamic lesions are the characteristic finding of JE and are seen in more than 87% to 94% of patients with JE with abnormal MR imaging. These can be bilateral or unilateral and are characteristically asymmetric with focal brain swelling in acute lesions (see Figs. 1–3 ). They appear hyperintense on T2-weighted and FLAIR MR images and slightly hypointense to gray matter on T1-weighted images. On CT, they may appear subtle and slightly hypodense with associated focal brain swelling. JE lesions typically do not enhance after intravenous contrast. Some investigators have reported hemorrhagic lesions, but, in our experience, hemorrhagic changes are rare. In a large series of 62 patients, 89% of the thalamic lesions were bilateral. In a retrospective study of a cohort of patients with CNS infections in a JE-endemic area in southern Vietnam, the presence of thalamic lesions on MR imaging had a sensitivity of 23%, specificity of 100%, positive predictive value of 100%, and a negative predictive value of 42.1% for diagnosis of JE. However, this study used low-field MR imaging (0.06 T), which may explain the low sensitivity found in the study. Our own figures of sensitivity and specificity of thalamic lesions on 1.5-T MR imaging for JE are 93.7% and 54.5% respectively in patients with meningoencephalitic syndrome. In the first week of the disease, the sensitivity and specificity are 90.9% and 50% respectively, which are comparable with Mac-ELISA tests (Handique SK, Deora P, unpublished data, 2011). The presence of thalamic lesions on MR imaging in a JE-endemic area can therefore be a rapid, sensitive, and fairly specific test for separating the patients with JE from those without JE, especially during the summer months when the number of cases of meningoencephalitis increases. Substantia nigra and basal ganglia lesions are the next most common lesions of JE and these too are asymmetric and accompanied by focal brain swelling in acute lesions (see Figs. 1–4 ). Cortical lesions are most commonly found in the hippocampi, although any part of the cerebral cortex may be involved. We found 17.7% hippocampal involvement in a large series of patients with JE. Hippocampal lesions have a characteristic appearance with predominant involvement of the body and tail with occasional involvement of the head and the amygdalae. Insular involvement is rare (see Fig. 1 B, C). The characteristic appearance and associated involvement of the thalami, substantia nigra, and the basal ganglia allow easy differentiation from HSE.
Diffusion-weighted (DW) MR imaging has been reported to help in the early diagnosis and characterize the duration of JE. In a study of 14 patients with JE, lesions appeared either hyperintense on DW imaging, when they were more than or equal to the number of lesions seen on T2-weighted images, or they were hypointense on DW images when more lesions were seen on T2-weighted images. This study found that 9 out of 14 patients showed more lesions on DW images compared with conventional T2-weighted images. Patients with longer disease duration showed significantly raised apparent diffusion coefficient (ADC) values. Others have found different results, however. In a study of 45 patients with JE (n = 38) and HSE (n = 7), patients with acute JE showed significantly less conspicuity of the lesions on DW images than on T2-weighted or FLAIR images. FLAIR images were found to be the best sequence for lesion detection of acute JE. In contrast, patients with acute HSE showed significantly more lesion conspicuity on DW images in comparison with T2-weighted or FLAIR images. Our experience has been similar. Our patients with acute JE tend to show more lesion conspicuity on conventional scans than on DW images. Often, acute JE lesions also show increased ADC values as well, with lesions appearing isointense on DW images and hyperintense on ADC map images. Less neuronal necrosis in acute JE in comparison with acute HSE and the presence of interstitial edema may explain these findings. DW imaging findings in acute JE are therefore variable, and this needs to be kept in mind while evaluating these patients (see Figs. 1, 2 and 4 ). Increased ADC values are not always seen in chronic JE lesions and must therefore be interpreted with caution (see Fig. 4 ). Other signs of chronic JE lesions such as better definition on T1-weighted and T2-weighted images resembling gliotic lesions and lack of mass effect with associated atrophy should be looked for.
JE rarely presents as a biphasic illness with early relapse of the disease within days or weeks of the first phase of the disease. The clinical manifestations of the second phase may be different from the first phase, but usually conform to the known features of the disease. MR imaging shows fresh areas of brain involvement in the second phase in addition to JE lesions seen in the first phase. We saw 1 such patient in a series of 62 patients with JE. Another study reported 6 patients in a series of 62 patients with JE.
Coinfection of JE with neurocysticercosis (NCC) has been reported from India and China. These diseases have several common epidemiologic and sociodemographic factors, including pig rearing, poor socioeconomic status and hygienic conditions, and malnutrition. More than a casual relationship between the 2 conditions has been suggested by several investigators, with coinfections being advocated as a prognosticator of poor outcome in JE. However, others have not found a significant relationship between the 2 infections. In a prospective study of 62 patients in our hospital, we observed a significantly high association of NCC with JE (19.3%) compared with the prevalence of NCC in controls (1.04%). Lesions of JE were significantly asymmetric with lateralization of the lesions to the side having maximum NCC or a cyst with edema (see Fig. 4 ). More florid JE lesions were seen in coinfections and this was reflected in the significantly higher number of abnormal CT scans in coinfections in contrast to abnormal CT scans in the group. Coinfections were significantly more common in children. We also found evidence of altered immune status in patients with coinfections, with these patients showing significantly lowered JEV IgM levels. Other imaging studies reported similar imaging findings in coinfections. NCC seems to have a synergistic effect on JE and probably facilitates the entry of the JEV into the brain because of the altered immune response.
JE has no specific treatment and the treatment is symptomatic and supportive. Because effective vaccines exist, vaccination of the population at risk is the method of choice for its prevention. Improved farming practices and sanitation, vector control, and reduction of man-mosquito contact are measures that have been effective in the control of the disease.
West Nile Encephalitis
West Nile virus (WNV) is a flavivirus that is closely related to other flaviviruses, such as JEV and dengue virus, and is transmitted to humans by mosquitoes from various species of birds that possibly act as both carriers and amplifiers of the disease. Various species of culicine mosquitoes have been identified to transmit the disease to man. Several birds that act as vertebrate reservoirs have been identified in WNV-prevalent areas. Since its first isolation in the West Nile district in Uganda in 1937, WNV has become widely distributed today throughout Africa, the Middle East, Europe, Asia, Canada, Central America, Mexico, the United States, and the Caribbean. It is endemic throughout Africa and the Middle East, whereas large outbreaks have occurred in several countries. In India, WNV was first reported in 1952. Presently it is widely prevalent in India in several states in the southern, eastern, and western parts of the country including Tamil Nadu, Karnataka, Andhra Pradesh, Maharashtra, Gujarat, Madhya Pradesh, Orissa, Rajasthan, and Assam. The disease usually presents as a mild febrile illness in this country. Sporadic cases of encephalitis have been reported in children. Despite the abundance of mosquito vectors and neuroinvasive strains of the virus in the country, no major epidemic has been reported to the scale of JE outbreaks. The reason for this is not clear, but may be because of the cross-protection provided by the presence of other flaviviruses in India.
After gaining entry into the blood stream, WNV from a mosquito bite replicates in the reticuloendothelial system. After a second phase of short-lived viremia, the CNS may be invaded, possibly through the hematogenous route, although other routes are possible, such as through the olfactory bulb, choroid plexus epithelial cells, infected immune cells, or retrograde axonal transport through infected peripheral neurons. Because of the rarity of encephalitis, little is known about the neuropathologic findings. Fatal cases show both meningoencephalitis and encephalitis. There is inflammatory change with formation of microglial nodules and neuronophagia with perivascular cuffs in the brain involving the gray and white matter. Brainstem involvement was typical, with involvement of the temporal lobes and basal ganglia. The anterior horns of the spinal cord are involved in patients presenting with spinal cord symptoms. Cranial nerve root involvement is also seen.
Seroprevalence studies suggest that most WNV infections are asymptomatic. A small proportion (20%–30%) of infected patients develops a mild febrile syndrome called WNV fever. A smaller subgroup (1 in 150) can develop neuroinvasive disease that may manifest as aseptic meningitis, encephalitis, acute flaccid paralysis, or Guillain-Barré syndrome. Definitive diagnosis of the disease is by showing the WNV-specific antibodies in the serum of CSF.
CT scan does not show any abnormalities in most cases of WNV infection. MR imaging may show abnormalities in more than one-third to more than one-half of the patients. Deep gray matter and brainstem involvement was found in 50% of cases in one study of 16 patients by MR imaging. The anatomic areas involved included the basal ganglia, thalami, mesial temporal lobe, midbrain, pons, and cerebellum. Thalamic involvement was seen in 3 (18.75%), a smaller proportion than JE. White matter involvement was seen in 2 patients. Others have reported a higher proportion of white matter disease, with 1 study reporting white matter involvement in as many as 50% ( Fig. 5 ). White matter abnormalities may mimic nonspecific demyelinating lesions and appear hyperintense on T2-weighted and FLAIR images. They show no mass effect or contrast enhancement and usually resolve on follow-up. Some may only be apparent on DW imaging, showing isolated restricted diffusion. Meningeal involvement is seen on contrast-enhanced MR imaging or as sulcal FLAIR hyperintensities (see Fig. 5 ). In patients presenting with acute flaccid paralysis, discreet spinal cord lesions are seen. These lesions may be nonspecific or at times show involvement of the anterior horns. Nerve root enhancement has also been reported. DW imaging has been reported to be helpful in lesion detection. In one study, diffusion abnormalities were noted in 50% of the patients. Both gray and white matter lesions may show restriction of diffusion. The reason for some lesions showing restricted diffusion is not clear. However, patients with lesions showing isolated restricted diffusion with no corresponding signal abnormality on FLAIR or T2-weighted imaging and patients with normal MR imaging scans have a better outcome than patients with abnormal signal intensity on FLAIR and T2-weighted images. This finding suggests that these areas of isolated restricted diffusion may not be representative of irreversible cell damage or death. Imaging findings of WNV encephalitis have not been reported from Asia or the Indian subcontinent.
There is no definitive treatment of the disease. Treatment is mainly symptomatic and supportive. No preventive vaccine exists. Disease control therefore is mainly through vector control.
Dengue Encephalitis
Dengue is the most common arboviral disease to infect man and is endemic in more than 100 countries. Approximately 2.5 billion people are at risk for infection. Estimated infections worldwide are 50 million to 100 million, out of which 25,000 die every year. In India, it is reported in more than 18 states of the country. It is caused by a flavivirus transmitted to man by the bite of the infected female Aedes mosquito. The infections may be:
- a.
Asymptomatic; or cause
- b.
Classic dengue fever or break-bone fever
- c.
Dengue hemorrhagic fever
- d.
Dengue shock syndrome
- e.
Other rarer manifestations like encephalopathy, hepatitis, or myocarditis.
The dengue virus is not generally neuroinvasive, but there is increasing evidence that it may cause encephalitis by direct invasion of the CNS. Isolation of the virus from the CSF, lymphocytic pleocytosis, and demonstration of virus-specific IgM in the CSF by some studies provide this evidence. In a series of 9 patients with dengue encephalitis examined by MR imaging in India, abnormality was seen in 1 with lesions in the globus pallidus. Other reports have described lesions in the thalami (like JE), hippocampi, temporal lobe, pons, and spinal cord.
Enterovirus Encephalitis
Enteroviruses (EV) include polio, Coxsackie, echo, and newer enteroviruses that are occasionally neuroinvasive in humans. Although poliovirus has the capability to cause infections of the spinal cord, echo and Coxsackie viruses usually cause aseptic meningitis. Newer EVs occasionally cause neurologic disease that includes aseptic meningitis, encephalitis, acute flaccid paralysis, or other CNS disorders. EV71 is an emerging virus that has shown expansion of its geographic range. It causes hand, foot, and mouth disease in children and, in the recent past, several outbreaks have been reported in southeast Asia and Pacific regions. Up to 30% of these patients may show CNS symptoms, although association with neurologic disease is variable. EV71, 76, and 89 encephalitis outbreaks have been reported from north India, whereas EV75 has been reported from the south. EV71 was the most common cause of viral encephalitis in children in a study from north India, causing 35.1% of all viral encephalitis. EVs are transmitted through the fecal-oral route, although respiratory-oral spread and spread by fomites is also possible. Invasion of the CNS is through the hematogenous route after viremia occurs. MR imaging findings of EV71 from Taiwan have been reported. Brainstem was the most common site of involvement. The posterior medulla was involved in 75%, posterior pons in 75%, midbrain in 50%, dentate nuclei of cerebellum in 45%, thalamus in 10%, putamina in 5%, and cervical spinal cord in 15% (see Fig. 6 ). In a study from north India, brainstem lesions were the most common and were seen in the midbrain and pons (43% each). Lesions were also noted in the thalamus (43%), cerebellum (28%), cerebral cortex, basal ganglia, and substantia nigra (14% each).
Nipah Virus Encephalitis
Nipah virus encephalitis (NVE) is caused by an emerging zoonotic virus first identified in Malaysia and Singapore in 1998. The Nipah virus (NV) is closely related to the Hendra virus. Both are members of the genus Henipavirus, a new class of virus in the Paramyxoviridae family. It is a neurotropic virus that causes severe encephalitis in humans, with case fatality varying from 40% to 75%. In Malaysia and Singapore, the virus was transmitted to man from infected pigs. The natural hosts of the virus are fruit bats of the Pteropotidae family. Farm animals such as pigs or horses possibly get infected from bat urine or saliva, passing on the disease to humans. Most of the infected in Malaysia were pig farm workers, possibly having contracted the disease from respiratory droplets, throat or respiratory secretions, or from handling infected tissue. Subsequently several NVE outbreaks have occurred in the sub-Himalayan region of the state of West Bengal in India and the adjoining areas of west central Bangladesh since 2001. In Bangladesh and India, infections most likely resulted from consumption of fruit or fruit products such as raw date palm juice contaminated by bat urine or saliva. Unlike in Malaysia and Singapore, man-to-man transmission has been documented in Bangladesh and India with the probable source of infection through handling excretions and secretions of infected patients. In North Bengal, transmission of the virus was reported in a health care setting, with 75% of cases occurring in staff and visitors to hospitals treating the patients. Pathologically, an unusual feature is vasculitis with thrombosis and parenchymal necrosis besides other features of encephalitis such as neuronophagia, microglial nodules, and perivascular cuffing. The incubation period varies from 4 to 45 days. Patients present with influenzalike symptoms followed by acute encephalitic syndrome. Survivors may completely recover; however, a small number may show a delayed relapse of encephalitis. In a study from Malaysia, CT scans of patients with NVE were usually normal, but almost all MR imaging scans were abnormal. The most common findings in the acute phase were focal subcortical and deep white matter lesions, and to some extent in the gray matter, that were hyperintense on T2-weighted and FLAIR images, usually without mass effect or edema. In another study from Singapore, patients with acute NVE showed small T2-hyperintense and FLAIR-hyperintense lesions less than 1 cm, mostly in the white matter. Restricted diffusion was observed in some of the larger lesions. Lesions were also seen in the cortex, pons, and cerebral peduncle. Some lesions showed contrast enhancement. These lesions possibly represented microinfarcts from vasculitis-induced thrombosis. Patients who were scanned 1 month after infection showed fresh, tiny foci of T1-hyperintense signal in the cerebral cortex primarily, with lesions also occurring in the white matter, pons, cerebellum, putamen, and thalamus. Only a few of these lesions showed susceptibility on gradient echo sequences. The pathologic correlates of these lesions are unclear but may represent laminar cortical necrosis. Most of the lesions resolved on follow-up in survivors ( Fig. 7 ). Imaging findings from India and Bangladesh have not been reported. No specific treatment or vaccines for NVE exist and treatment is mainly supportive.
Rabies
Rabies (or hydrophobia) is a zoonotic encephalomyelitis and is one of the oldest and most feared diseases known to man, with almost 100% fatality. The rabies virus is a single-stranded RNA virus of the genus Lyssavirus and family Rhabdoviridae. In the Indian subcontinent and other Asian countries, only genotype 1 out of 7 known genotypes is prevalent. It has a worldwide prevalence, although many countries that are geographically isolated, such as Australia and the United Kingdom, are free of the disease. In India, rabies occurs in all parts of the country with the exception of the islands of Andaman and Nicobar, and Lakshadweep. The estimated annual human mortality in the Indian subcontinent is approximately 30,000, but the figure may be 10 times more than that reported. More than 90% of human rabies in India is caused by bites of infected animals, mainly dogs. After inoculation, the virus ascends by retrograde axoplasmic spread to the spinal cord and then to the brain. The initial areas of involvement include the hypothalamus, hippocampus, and the limbic system, with eventual involvement of the entire brain. Despite widespread replication of the virus in the CNS, pathologic changes are minimal, probably because of neuronal apoptosis rather than necrosis and functional derangement of neurotransmitters playing a role in the pathogenesis.
After a variable incubation period that may last for days to several years, patients present clinically with the more common classic encephalitic or furious rabies, or the less common paralytic or dumb rabies. Both forms ultimately lead to coma and death. Although the diagnosis of the furious form can be made from the typical clinical symptoms and signs that include the classic hydrophobia (from which rabies gets its other name) and aerophobia, the dumb form can present a diagnostic dilemma because these patients present with ascending paralysis and may lack the classic symptoms of rabies.
There is a lack of imaging literature of rabies, possibly because of difficulty in imaging these patients. CT may show diffuse or focal areas of hypoattenuation in the basal ganglia, hippocampus, periventricular white matter, and brainstem. In a study of 5 patients with both furious and paralytic types of rabies, MR imaging showed nonenhancing, ill-defined, subtle T2-hyperintense lesions in the brainstem, hippocampi, hypothalami, deep and subcortical white matter, and deep and cortical gray matter in noncomatose patients. Gadolinium contrast-enhancing lesions were noted in the hypothalami, brainstem nuclei, spinal cord gray matter, and intradural cervical nerve roots only when the patients became comatose. There was no difference in the lesion pattern between furious and paralytic rabies. Differential functional impairment rather than a direct process of virus infection in certain regions of the CNS has been suggested as a possible explanation.
Measles
Measles is an acute, highly infectious disease of childhood and is characterized by fever, upper respiratory symptoms, and the development of a characteristic rash. It is caused by an RNA paramyxovirus and transmission occurs by respiratory droplet infection. Measles is endemic in virtually all parts of the world, but is rare in the developed world because of effective vaccination. An estimated 30 million children are infected worldwide with measles and about 1 million die. In India, the number of measles cases has decreased from about 0.2 million cases in 1987 to about 50,000 cases in 2005. CNS infections by the measles virus can result in acute measles encephalitis (AME), subacute measles encephalitis (SME), or subacute sclerosing panencephalitis (SSPE). SME is a recently recognized condition that occurs in the immunocompromised host and is caused by wild-type measles virus. SSPE is a slow virus infection of the brain caused by measles and characteristically manifests after several years from the initial infection. CNS complications are rare and approximately 1 in 1000 cases results in acute encephalitis. In a study of 155 patients with viral encephalitis from north India, 7% of acute encephalitis was caused by measles virus. SSPE is even rarer and the frequency of occurrence is approximately 1 to 4 cases in 1 million in developed countries, with a possible incidence of up to 21 cases in 1 million in developing countries like India. With the introduction of a mass immunization program for measles in India in 1986, the incidence of SSPE is decreasing in this country. No reports of SME are available from the Indian subcontinent.
AME is caused by direct invasion of the brain by the measles virus and symptoms usually develop within 8 days of onset of measles during the period of measles exanthema. CSF analysis reveals mild pleocytosis, usually mononuclear, mildly increased protein level, and normal glucose level. Detection of specific viral genome in the CSF suggests direct viral invasion of the CNS. Some investigators have not been able to show specific viral RNA in the brain of infected patients, leading to the belief that AME may be caused by autoimmune mechanisms. AME has a mortality of approximately 10% to 20%. MR imaging studies in AME from Korea have shown T2-hyperintense lesions in patients diffusely involving the cortex, corpus striatum, and white matter, with areas of petechial hemorrhage. DW imaging showed restricted diffusion and contrast-enhanced imaging showed cortical and leptomeningeal enhancement.
SSPE is a slow virus infection that is a result of persistent measles virus in the CNS. Most patients with SSPE have a history of primary measles infection at an early age. Onset of disease occurs 6 to 8 years after the initial measles attack. Because the incubation period is less than a decade, the disease commonly occurs in childhood but young adults may be affected. Boys are most commonly affected (male/female = 3:1), although measles shows no sex predilection. A close temporal relationship with other viruses, such as Epstein-Barr virus or parainfluenza type 1 virus, has also been suggested as a risk factor for SSPE.
The exact pathogenesis of SSPE is unknown. Measles virus probably gains entry into the brain by infection of the endothelial cells or by circulating inflammatory cells. Despite the long latency period, there is evidence that the measles virus gains entry into the brain soon after the acute infection and subsequently spreads throughout the brain. In the early stages, there is variable inflammation of the meninges, cortical and deep gray matter, and white matter. There is neuronophagia, gliosis, proliferation of astrocytes, perivascular cuffing, lymphocytic and plasma cell infiltration, demyelination, and inclusion bodies in the neurons and glial cells. In the late stages, there is scanty inflammation with severe neuronal loss in the cortex and deep gray matter with thinning of white matter and severe gliosis. Inclusion bodies are scarce. Clinically, the disease starts as minor behavioral and intellectual changes in a previously healthy child. There is development of motor dysfunction and characteristic myoclonic jerks. Within months to years, there is deterioration of sensorium followed by coma. Four stages of the disease have been described, comprising stage I, which includes patients with mild behavioral changes, progressing to stage IV, which includes patients in the vegetative state with loss of cerebral cortical function. Diagnosis is established by clinical presentation, abnormal electroencephalogram findings, increased measles antibodies in serum and CSF, and brain biopsy.
Imaging with CT and MR in SSPE shows white matter changes that appear hyperintense on T2-weighted MR imaging and hypoattenuated on CT scans. These changes are more apparent on MR imaging. In the early stages, white matter changes are asymmetric and more commonly seen in the parietooccipital than in the frontal region. Gray matter changes may also be observed that are more apparent on MR imaging and appear hyperintense on T2-weighted and hypointense on T1-weighted scans. Involvement of the brainstem, cerebral and cerebellar peduncles, and cerebellum may also be seen. The progression of MR imaging findings seems to follow a pattern with focal white matter changes appearing first followed by atrophic changes. In advanced stages, atrophy is more severe and diffuse white matter involvement with thinning of corpus callosum is noted. However, despite lesions on conventional MR imaging following a set pattern, MR imaging changes do not correlate well with clinical stages of the disease. DW imaging shows facilitated diffusion within the lesions of SSPE with raised ADC values.
Although conventional MR imaging findings and clinical stages of SSPE are not well correlated, newer MR techniques such as DW imaging, MR spectroscopy, and diffusion tensor imaging (DTI) and diffusion tensor tractography (DTT) have been reported to be of more help in detecting early disease and helping in clinical staging. One study found a significant difference in the ADC values between patients with clinical stage II and stage III of the disease with highest ADC values in stage III disease. Both single and multivoxel MR spectroscopy have been reported to detect early disease and differentiate between stage II and stage III disease. In one study, children with stage II disease showed no abnormalities on conventional MR imaging, but showed increased choline and myoinositol (MI) levels with normal N -acetyl aspartate (NAA) levels in the frontal subcortical white matter and parietooccipital white matter in comparison with controls. Higher choline levels were observed in the parietooccipital region than in the frontal regions, reflecting the early pathologic changes seen in the former area. However, decreased NAA, increased choline and MI, and increased lactate and lipid peaks were seen in stage III SSPE in relation to controls. These findings probably reflect inflammation in stage II, and demyelination, gliosis, cellular necrosis, and anaerobic metabolism in stage III. DTI has also been reported to detect changes in the early stage of SSPE with normal conventional MR imaging. In a study of 21 patients with stage II SSPE from India, DTI revealed abnormal fractional anisotropy (FA) values in both normal-appearing and abnormal-appearing white matter on T2-weighted images compared with controls. Mean diffusivity (MD) values were significantly increased in the frontal and parietooccipital periventricular white matter ( Fig. 8 ) of patients with both normal-appearing and abnormal-appearing white matter on T2-weighted images. In another study from India by the same group of investigators, tract-specific FA values in some of the major white matter tracts were shown to correlate inversely with clinical grades II to IV.