Radiographic imaging comes as an essential tool in modern dentistry that helps clinicians visualize structures that are otherwise hidden from view during a clinical examination.
From diagnosing simple caries to identifying complex tumors, radiographs serve as an invaluable extension of the clinician’s diagnostic tools.
This visual guide explores the radiographic characteristics of common oral pathologies, empowering clinicians to interpret findings confidently and make informed decisions for their patients.
1. Dental Caries
Radiographic Appearance:
Dental caries is one of the most frequently diagnosed dental conditions. To identify dental caries radiographically check for radiolucent zones. These are due to the demineralization of enamel and dentin.
- Interproximal Caries: These usually commence at the contact area. They present a triangular radiolucency, with the base towards the enamel, and the apex at the DEJ.
- Occlusal Caries: These generally are not apparent externally on a radiograph until they are near the dental caries of the dentin. When there, they demonstrate as a soft radiolucency just deep to the occlusal enamel.
- Root Caries: Seen as poorly demarcated, saucer-shaped radiolucencies along root surfaces and are commonly identified where there is gingival recession.
Clinical Relevance:
Early detection is critical. Radiographs may reveal hidden lesions not evident clinically. However dentists will need to use minimally invasive intervention to clear them.
2. Periapical Lesions
Radiographic Appearance:
These lesions result from pulpal inflammation or necrosis and extend into the periapical tissues.
- Abscesses: They show a poorly defined radiolucent area, often with loss of lamina dura and widening of the periodontal ligament (PDL) space.
- Granulomas: These present as a round or oval, well-defined radiolucency smaller than 1.5 cm.
- Periapical (Radicular) Cysts: These are typically larger than granulomas with distinct corticated borders, that indicate a chronic process.
Clinical Relevance:
Differentiating among these lesions radiographically can be challenging. A pulp vitality test, history of symptoms, and follow-up imaging may aid in accurate diagnosis.
3. Periodontal Disease
Radiographic Appearance:
Periodontal disease leads to the destruction of the supporting structures around teeth. Radiographic signs include:
- Horizontal Bone Loss: Uniform reduction in bone height parallel to a line connecting adjacent CEJs (cementoenamel junctions).
- Vertical (Angular) Bone Loss: Shows irregular bone resorption forming angular defects adjacent to the roots.
- Furcation Involvement: These present as radiolucency in the furcation area of multi-rooted teeth, indicating advanced disease.
- Widening of the Periodontal Ligament (PDL) Space: Often an early sign of trauma from occlusion or inflammation.
Vertical bitewings and periapical radiographs are ideal for evaluating bone levels and detecting early periodontal changes.
Clinical Relevance:
Radiographs provide essential information about bone support and disease severity. Recognizing bone loss patterns helps with staging periodontitis, guiding treatment planning (e.g., scaling and root planing vs. surgery), and tracking disease progression over time.
4. Impacted Teeth
Radiographic Appearance:
Impacted teeth usually appear submerged below the normal eruption level and may be angulated or completely inverted. If you spot a surrounding follicular sac larger than 3–5 mm it may be a sign for cystic changes.
Complications:
Impacted teeth may lead to resorption of adjacent roots, infection, or development of pathologic lesions.
Clinical Relevance:
Impacted teeth can cause crowding, root resorption, cyst formation, or infection. Early radiographic detection aids in timely surgical planning and prevents complications.
5. Odontogenic Cysts
These are the most common cystic lesions in the jaws, often asymptomatic and found during a routine check up.
Radiographic Types:
- Dentigerous Cyst: Unilocular radiolucency surrounding the crown of an unerupted or impacted tooth, usually third molars or canines.
- Radicular Cyst: Arises from epithelial rests in response to chronic inflammation. It appears as a round, corticated radiolucency.
- Lateral Periodontal Cyst: Found between the roots of vital teeth, most commonly in the mandibular canine-premolar region.
Clinical Relevance:
Accurate diagnosis may require histopathologic confirmation following surgical enucleation.
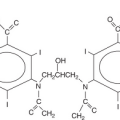
6. Odontogenic Tumors
Ameloblastoma:
Characterized by a multilocular “soap bubble” or “honeycomb” radiolucency. They typically affect the posterior mandible and cause significant expansion.
Odontoma:
- Compound Odontomas: Appear as a cluster of miniature tooth-like structures.
- Complex Odontomas: Present as an irregular radiopaque mass with no anatomical resemblance to teeth.
Cementoblastoma:
A rare benign tumor fused to the root of a tooth, presenting as a dense, round radiopacity with a radiolucent halo.
Clinical Relevance:
These require surgical removal, and in some cases, extraction of the involved tooth.
7. Maxillary Sinus Pathologies
Dentists often first detect sinus issues during routine imaging.
Common Radiographic Signs:
- Mucosal Thickening: Appears as a linear radiopacity along sinus walls.
- Sinusitis: Total opacification or air-fluid levels may be visible.
- Retention Pseudocyst: Dome-shaped radiopacity, not associated with bone destruction.
Clinical Relevance:
Dr Salo explains, “Maxillary sinus issues can mimic dental pain, especially in upper molars. Recognizing radiographic signs like mucosal thickening or fluid levels helps avoid misdiagnosis. It’s also essential for surgical planning—e.g., avoiding oroantral communication during extractions or implant placement.”
8. Developmental Anomalies
Supernumerary Teeth:
These may interfere with the eruption or cause crowding. The most common is the mesiodens, often seen between the upper central incisors.
Dens Invaginatus (Dens in Dente):
A radiolucent invagination into the crown or root, often in maxillary lateral incisors.
Taurodontism:
Teeth exhibit elongated pulp chambers and short roots; seen in molars on radiographs.
Clinical Relevance:
Developmental anomalies like supernumerary teeth can delay eruption or cause crowding. Others, like dens invaginatus or taurodontism, increase the risk of pulp exposure or complicate endodontic treatment. Early detection aids in timely intervention and treatment planning.
9. Trauma and Fractures
Dental trauma can be localized to the tooth, alveolar bone, or jaw.
Crown and Root Fractures:
These are seen as radiolucent lines or fragmentation of tooth structure.
Alveolar Fractures:
May present as discontinuities in the alveolar bone, altered PDL space, or displaced teeth.
Mandibular Fractures:
Common sites include the condyle, angle, and symphysis. Panoramic imaging is effective for screening, but CBCT is superior for evaluation.
Clinical Relevance:
Radiographs help assess the extent of dental and jaw trauma, guiding emergency care and long-term treatment. Undetected root or alveolar fractures can lead to tooth loss, while missed jaw fractures may affect occlusion and healing.
Conclusion
Radiographic examination is essential for diagnosing oral pathologies, many of which may be asymptomatic or difficult to detect clinically.
Clinicians must not only recognize common radiographic patterns but also interpret them in conjunction with clinical findings.
As imaging technology continues to evolve—particularly with the growing use of Cone Beam CT—dentists are better equipped than ever to detect disease earlier and plan more precise, effective treatments for their patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree