© Springer-Verlag Berlin Heidelberg 2015
Andor W.J.M. Glaudemans, Rudi A.J.O. Dierckx, Jan L.M.A. Gielen and Johannes (Hans) Zwerver (eds.)Nuclear Medicine and Radiologic Imaging in Sports Injuries10.1007/978-3-662-46491-5_88. Radiologic Imaging of Sports-Induced Brain Injuries
P. M. Parizel1 , J. Kremling2, C. Janssen1, S. Laurijssen1, J. Van Goethem1, J. Huyskens1, F. De Belder1, C. Venstermans1, L. van den Hauwe1 and W. Van Hecke1, 3
(1)
Department of Radiology, Antwerp University Hospital, University of Antwerp, Antwerp, Belgium
(2)
Faculty of Medicine and Health Sciences, Ruhr-University Bochum, Bochum, Germany
(3)
icoMetrix, Leuven, Belgium
Abstract
TBI can occur in a wide range of sports activities. Lesions are most commonly caused by impact (contact sports) or activities involving high velocity. Acute sports-related injuries are indistinguishable from head trauma sustained in other accidents. Recurring craniocerebral injuries, such as in sustained in contact sports, can lead to chronic traumatic encephalopathy (CTE). This condition is a tauopathy, which is caused by repetitive mild traumatic brain injury (mTBI). Players of contact sports, such as rugby, hockey, boxing, or American football, have an increased risk of acquiring this condition.
Imaging studies play an important role in the diagnosis, management, and follow-up of sports-related TBI. CT remains valuable for the detection of intracranial hemorrhage, skull fractures, and mass effect; unfortunately this technique is less sensitive for lesions such as diffuse axonal injury (DAI). Therefore, whenever there is a discrepancy between the clinical status of a patient and the CT findings, MRI should be used. MRI is becoming increasingly important for diagnosing parenchymal damage in sports-induced injuries. New sequences, such as susceptibility-weighted imaging (SWI), are very useful to detect microhemorrhagic foci. Diffusion-weighted imaging (DWI) and especially diffusion tensor imaging (DTI) provide quantitative measurements (such as FA, MD, ADC) which can be used as biomarkers for outcome prediction. Lower fractional anisotropy (FA) and high lesion count and volume have been related to poorer functional outcome. Other useful imaging modalities are 1H-magnetic resonance spectroscopy (1H-MRS), functional magnetic resonance imaging (fMRI), and positron emission tomography (PET).
8.1 Introduction
Given the increasing popularity of all kinds of sporting activities, it should not come as a surprise that the incidence of sports-related injuries is also rising.
Fortunately, injuries to the head and brain are not the most common lesions caused by playing sports, but they should be taken seriously, because they may lead to significant morbidity and/or mortality. In sports, injury to the head and brain is typically caused by physical contact with another person or with a stationary object. These sports may include activities involving high speeds (e.g., skiing, snowboarding, horse-riding, automobile or motorcycle racing, bicycling, roller blading, skateboarding, etc.) or contact sports (such as boxing, martial arts, rugby, American football, hockey, soccer, lacrosse, etc.).
In clinical terms, sports-related craniocerebral lesions can be subdivided into “acute injuries” and “chronic or repetitive injuries.”
Acute craniocerebral injuries, such as collisions which can occur in high-speed sports, basically present the same imaging characteristics as other types of traumatic brain injury, unrelated to sports; therefore, acute craniocerebral injuries will not be discussed in detail.
Conversely, in this chapter, we shall focus our attention on chronic or repetitive craniocerebral injuries, which are typically encountered in contact sports.
8.2 Definitions
Injury to the brain, due to chronic or repetitive trauma, has first been described by H. S. Martland in 1928 (Martland 1928); he used the expression “punch drunk,” which refers to the neuropsychiatric impairment caused by repetitive blows to the jaw and head (mainly occurring in rather poor boxers). Pathophysiologically these changes were attributed to recurrent concussions (Martland 1928).
Guidelines by the American Association of Neurology define concussion as “a trauma-induced alteration in mental status that may or may not involve loss of consciousness” (Quality Standards Subcommittee 1997), with amnesia and confusion being the most prominent symptoms of concussion (Report of the Quality Standards Subcommittee 1997; Giza et al. 2013; Mendez et al. 2005).
Typically, in these patients, no structural changes of brain tissue can be identified on standard radiological studies performed in the acute setting (McCrory et al. 2013). However, recurrent concussions can cause various neuropsychiatric sequelae including postconcussion syndrome, chronic traumatic encephalopathy, and dementia pugilistica (Dashnaw et al. 2012). Despite the fact that some authors consider these conditions to be different entities, the terms are often used interchangeably. Persistent postconcussion syndrome, or sometimes simply postconcussion syndrome, is an elusive and only vaguely defined syndrome, which is characterized by mild post-traumatic mental impairment with no clear pathological correlate. It is usually a self-limiting condition, with 80–90 % of patients showing full recovery within the first 10 days, which distinguishes it from chronic traumatic encephalopathy. However, in some patients the transition to chronic traumatic encephalopathy does occur and is usually assumed if symptoms last longer than 3 months (Mendez et al. 2005; Gandy et al. 2014; Larrabee and Rohling 2013; Hung et al. 2014; Henry et al. 2011a, b; Erlanger et al. 1999; Ryan and Warden 2003). For reasons of clarity and consistency, in this chapter we will use exclusively the term chronic traumatic encephalopathy (CTE); this concept was formerly known as “dementia pugilistica” (from the Latin noun “pugil” or “pugilator” meaning “fistfighter, boxer”) (Erlanger et al. 1999; Saulle and Greenwald 2012).
CTE is a condition of insidious onset causing emotional lability, cognitive impairment, and Parkinson-like symptoms. It usually starts with mild cognitive impairment, such as irritability, poor memory, and attention deficit. As the disease progresses, aggression and confusion become more prevalent, leading in some cases to depression and suicide. Ultimately, Parkinsonian symptoms, loss of cerebellar function, and dementia become apparent. Two thirds of athletes, who retire from sports during a symptom-free interval, do not experience any symptoms until later in life. Typical onset of CTE is between 30 and 65 years of age. The severity of the disease appears to be linked to the number of concussions or traumatic brain injuries sustained throughout the sports career; however, the role of the severity of impact on disease progression has yet to be determined. Young age has been found to be a protective factor, possibly because of the brain’s higher plasticity in comparison to older populations. Other risk or protective factors, especially the presence of ApoE4 as a negative risk factor, remain controversial (Gandy et al. 2014; Saulle and Greenwald 2012; Gavett et al. 2011; Karantzoulis and Randolph 2013; Levin and Bhardwaj 2014; Mez et al. 2013).
8.3 Epidemiology of Traumatic Brain Injury and Concussion in Athletes
Traumatic brain injury (TBI) has been estimated to affect 1.7–2.7 million people annually in the United States of America (USA) (Coronado et al. 2012; Faul et al. 2010). Men are more commonly involved than women. Males are reported to be more prone to sustain TBI through all age groups, with an annual rate of TBI that is up to 2.7 times higher than for females (Faul et al. 2010). However, in a study among children aged 5–18 years in the USA, the authors could not find evidence of differences in odds to be admitted to hospital due to sports-related concussion between sexes, though increased age was associated with an increase in odds (Yang et al. 2008).
In the USA more than 300,000 people suffer sports-related mild-to-moderate TBIs in any given year (Sosin et al. 1996). The annual incidence of sports-related TBI has experienced a steep increase from 19.7/100,000 population in 1998 to 45.6/100,000 population in 2011, which might reflect an increase of people involved in playing sports (Selassie et al. 2013). It has been estimated that 2.5 concussions per 100,000 athletic exposures occur across all sports in US high school students, with athletic exposures being the participation in one competition or practice (Guerriero et al. 2012). In the Canadian National Population Health Survey, more than 54 % of all concussions were sports-related, with a peak in the age group 16–34, where more than 85 % of all concussions were sports-related (Gordon et al. 2006). Sports-related severe concussional head injury in children has been found to be six times more likely to have been caused during an organized sports event than being attributable to other leisure physical activities (Browne and Lam 2006).
In a large epidemiological study on the incidence of sports-related craniocerebral injuries in South Carolina (USA), TBI resulted most commonly from having been kicked in football, followed by injuries due to falls (Selassie et al. 2013). Noble et al. reviewed the incidence of concussions in different sports, demonstrating an incidence of 0.86–1.45 concussions per 100 games among professional American football players. At college level, 2.5 concussions per 1,000 competition athletic exposures occurred; at high school level, the incidence of head injuries is lower, ranging from 3.1 (during practice) to 22.9 (during competitions) per 10,000 athletic exposures. The lowest incidence was observed in youth leagues with “only” 1.76–2.53 concussions per 1,000 athletic exposures, with age being a risk factor. In ice hockey and field hockey, the incidence is 0.72–1.81 per 1,000 athletic exposures, with a slightly higher incidence for females than males. Among soccer and European football players, 0.06 concussions per 1,000 player hours in men and women at professional level; 0.3–0.6 per 1,000 athletic exposures for males and 0.4 per 1,000 athletic exposures for females at college level; and 2.1 (males) to 3.4 (females) per 10,000 athletic exposures at high school level have been reported (Noble and Hesdorffer 2013). To summarize, these epidemiological data show that there is an increasing incidence of concussion across all sports, with American football having the highest incidence of concussion, followed by hockey and soccer.
Accurate figures are hard to obtain, because sports-related concussions are frequently underreported. The most likely reason for this is that the great majority of concussions are mild and might not even be recognized by the athletes themselves (Langlois et al. 2006). One study among high school American football players in the USA revealed that only 47.3 % reported their injury. Concussions were not reported when the athlete considered the injury unimportant, did not want to be withheld from competition, or was not aware of the likelihood of concussion (McCrea et al. 2004). In another study, among athletes exercising contact sports, the authors compared the answers given during a concussion symptom survey (CSS) with occurrence of self-reported previous concussions; 71 % of athletes reported symptoms, which were consistent with those experienced with concussion, yet had not given a history of previous concussion (LaBotz et al. 2005). Estimates by the British Columbia Amateur Hockey Association (BCAHA) for concussions among both elite and non-elite youth players demonstrated an incidence of concussion in official reports between 0.25 and 0.61 concussions per 1,000 player game hours (PGH) for male players. However, volunteers estimated that the incidence is significantly higher, ranging from 4.44 to 7.94 per 1,000 PGH, with actual players reporting an incidence between 6.65 and 8.32 (elite) and 9.72–24.30 (non-elite) per 1,000 PGH (Williamson and Goodman 2006). Additionally, many athletes continue to compete even when experiencing symptoms consistent with concussion (Kaut et al. 2003).
8.4 Pathophysiology of Sports-Induced Chronic Traumatic Encephalopathy
It is generally accepted that chronic traumatic encephalopathy (CTE) is caused by repetitive acceleration/deceleration injuries, more commonly by their milder forms and in particular without any open-head injuries. CTE is currently assumed to be a progressive tauopathy (Gandy et al. 2014; Saulle and Greenwald 2012; Gavett et al. 2011; Karantzoulis and Randolph 2013; Levin and Bhardwaj 2014; Mez et al. 2013; Bramlett and Dietrich 2014; Costanza et al. 2011; McKee et al. 2009, 2013; Omalu et al. 2011).
The modern concept of CTE was first described by the Boston (Massachusetts, USA) research group headed by A. C. McKee in 2009 (McKee et al. 2009). Since then, these authors have proposed a four-stage histopathological classification system (McKee et al. 2013). A similar, though not identical, classification was published by a Sacramento (California, USA) research group in 2011 (Omalu et al. 2011). While both classifications involve a four-stage grading system of disease severity, they mainly differ in the description of the extent and importance of the presence of neurofibrillary tangles, Aβ amyloid plaques, and brain atrophy (Gandy et al. 2014; Saulle and Greenwald 2012; Karantzoulis and Randolph 2013; McKee et al. 2013; Omalu et al. 2011). Unfortunately, these histopathological models remain under discussion and are not yet perfect. Most patients, in whom the diagnosis of CTE was established postmortem, did not die of the disease itself but of other causes, an observation which is very uncommon in other neurodegenerative diseases. At the same time, many patients met the pathological criteria for Alzheimer’s disease, which raises the issue if these changes are related to (ab)normal aging or if they are really caused by CTE. Inconsistent histological findings and a selection bias negatively influence its scientific value also (Gandy et al. 2014; Saulle and Greenwald 2012; Levin and Bhardwaj 2014; Bramlett and Dietrich 2014; McKee et al. 2013).
On a cellular level, mild traumatic brain injuries cause diffuse axonal injury (DAI), white matter loss, and microhemorrhages due to coup/contrecoup injuries and increase of traction and shearing forces on nerve fibers. The extent of DAI after traumatic brain injury is an important predictor of prognosis of post-traumatic cognitive impairment (Gandy et al. 2014; Saulle and Greenwald 2012; Levin and Bhardwaj 2014; Bramlett and Dietrich 2014; Sharp et al. 2014). Microtrauma to the brain has been postulated to lead to neurotoxicity from increased extracellular glutamate levels, causing subsequent demyelination. At the same time generation of reactive oxygen and nitrogen species can cause oxidative stress to neuronal membranes and irreversible damage of membranes (Gandy et al. 2014; Saulle and Greenwald 2012; Bramlett and Dietrich 2014; Byrnes et al. 2014; Henry et al. 2011a, b). Other factors that could further damage the brain include post-traumatic inflammation and apoptosis, though they could also be part of (benign) physiological repair mechanisms. Microglia cells, in particular, have the ability to switch between neuroreparative and neurodestructive states, even though this may be just another interpretation of the same process. Increased levels of inflammatory peptides and of proteins of neuroglial origin are frequently observed and might be used as biomarkers to assess severity of neurotrauma. However, at the current stage, scientific evidence is insufficient to support usage of biomarkers in clinical practice (Gandy et al. 2014; Saulle and Greenwald 2012; Bramlett and Dietrich 2014; Byrnes et al. 2014; Papa et al. 2013; Yokobori et al. 2013).
Histologically, areas of focal DAI and inflammation correspond to which has been described as progressive tauopathy. Currently, attempts are made to diagnose chronic traumatic encephalopathy, and its predecessors DAI and microhemorrhages in particular, by means of neuroimaging to possibly prevent further damage to the brain (Gandy et al. 2014; Saulle and Greenwald 2012; Gavett et al. 2011; Karantzoulis and Randolph 2013; Levin and Bhardwaj 2014; Mez et al. 2013; Bramlett and Dietrich 2014; Costanza et al. 2011; McKee et al. 2009, 2013; Omalu et al. 2011; Sharp et al. 2014; Papa et al. 2013; Yokobori et al. 2013).
John Grimsley – The man who brought us CTE (Boston University CTE Center John Grimsley; NFL Enterprises LLC John Grimsley; Schwarz 2008)
John Grimsley, a professional National Football League (NFL) player died at the age of 45 after he shot himself accidentally. During his career, from 1984 to 1993, he played a total of 133 games for the Houston Oilers and later for the Miami Dolphins. He donated his brain to the Center for the Study of Traumatic Encephalopathy (CSTE) at Boston University, where it was examined postmortem. Evidence of excessive CTE was found, and in particular there were large areas with tau protein depositions. His brain was the first being examined at CSTE in Boston. Ann C. McKee, MD, codirector of the CSTE and one of the key figures of the Boston CTE research group, publicly commented that the changes seen in Grimsley’s brain were consistent with dementia pugilistica. The last 4–5 years before his tragic death Grimsley had exhibited irritability and impairment of his short–term memory, according to his wife. He also admitted to her that he had sustained eight to nine concussions during his professional career.
8.5 What Is the Role of CT for Visualizing Chronic Traumatic Encephalopathy?
Computed tomography (CT) is known to underestimate the amount of traumatic brain damage, because of its low sensitivity in detecting subtle parenchymal changes. Since many years, we know that CT tends to severely underestimate the cerebral damage which occurs in diffuse axonal injury (DAI), white matter changes, and microhemorrhages (Parizel et al. 1998; Byrnes et al. 2014; Gonzalez and Walker 2011; Iverson et al. 2000; Lee et al. 2008; Mittl et al. 1994; Suskauer and Huisman 2009; Toledo et al. 2012). This was confirmed in the TRACK-TBI Pilot Study, where 27 % of all patients with mild TBI and an initially normal CT scan on admission later showed an abnormal magnetic resonance imaging (MRI) scan at an average of 12 days post-injury (Yuh et al. 2013).
Despite these important limitations, its wide availability and short acquisition time still make that CT remains the most frequently used imaging technique in the assessment of craniocerebral injuries. CT provides very accurate information on skeletal abnormalities (such as fractures), macroscopic hemorrhages, and other space-occupying lesions. The main role of CT in the emergency department is therefore to rule out major injuries, which require immediate attention (Byrnes et al. 2014; Gonzalez and Walker 2011; Lee et al. 2008; Suskauer and Huisman 2009; Toledo et al. 2012; Coles 2007; Dimou and Lagopoulos 2014; Johnston et al. 2001; Le and Gean 2009). In short, CT is extremely valuable for detecting skull fractures, macroscopic hemorrhage, and soft tissue injuries, but the method severely underestimates the true extent of parenchymal damage.
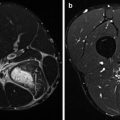
8.6 Magnetic Resonance Imaging Is Superior in Detecting Microhemorrhages
For imaging patients with TBI, T1-weighted, T2-weighted, gradient echo T2*-weighted, and/or susceptibility-weighted imaging (SWI) and fluid-attenuated inversion recovery (FLAIR) sequences are frequently employed (Aquino et al. 2015).
Susceptibility-weighted imaging (SWI) has been found to be a very sensitive MRI sequence to find microhemorrhages. It is well known that, intracranial hemorrhages present a variable signal intensity on T1- and T2-weighted images, depending on the time after injury (Parizel et al. 2001). In the chronic stage, hemosiderin deposits remain as the end product of the hemoglobin degradation process. Hemosiderin appears hypointense on gradient echo T2* and SWI (Kang et al. 2001; Liu et al. 2014; Moritani et al. 2009; Zhu et al. 2008). SWI is superior to T2-weighted, gradient echo T2*-weighted, and FLAIR imaging in detecting microhemorrhages, with gradient echo T2* being superior to T2-weighted and FLAIR sequences (Zhu et al. 2008; Geurts et al. 2012; Spitz et al. 2013). Especially in individuals with a history of high-speed acceleration/deceleration trauma and suspected DAI, SWI has a very high yield in detecting punctate microhemorrhages, which is the hallmark of DAI. The diagnostic yield for microhemorrhages is estimated to be 3–6 times higher than T2- or T2*-weighted imaging (Babikian et al. 2005; Mittal et al. 2009; Tong et al. 2004, 2008). However, it has yet to be determined if this increase in sensitivity alters clinical outcome (Yates et al. 2013).
Detection of microhemorrhages is important in sports-related TBI. Hasiloglu et al. demonstrated an increased lesion count in boxers on SWI in comparison to T2- and T2*-weighted imaging, confirming its superiority in sports-related mild TBI (Hasiloglu et al. 2011). In one study among university-level ice-hockey players over a season, SWI demonstrated an increase of the number of hypointensities, suggesting multiple microhemorrhages due to (sub)concussions (Helmer et al. 2014).
8.7 Proton (1H) Magnetic Resonance Spectroscopy in Head Trauma
Proton magnetic resonance spectroscopy (1H-MRS) is the most widely used form of MRS, though other nuclei, such as 13C and 31, have been studied and used as well. 1H-MRS is more easily performed than spectroscopy with other nuclei due to the prevalence of protons in biological tissues and in the human body. Currently, 1H-MRS can measure more than 20 different metabolites. Aspartate, choline, creatine, glutamate and glutamine, lactate, myoinositol, and N-acetyl-aspartate (NAA) are currently the most important metabolites used in the study of traumatic brain injury (TBI). In the absence of pathology, the concentration of these metabolites has been found to be very stable across individuals (Suskauer and Huisman 2009; Burtscher and Holtås 2001; Danielsen and Ross 1999; Lin and Rothman 2014; Mountford et al. 2010). 1H-MRS is a robust technique, and it appears likely that, in the future, it will be possible to broaden the neurobiochemical profile by using shorter echo times (Duarte et al. 2012). No significant differences in the results of biomarker levels have been found between 1.5 T and 3.0 T scanners (Kantarci et al. 2003).
N-acetyl-aspartate (NAA) is considered to be a marker of neural integrity and viability. Since it is found almost exclusively in neurons, it is a very sensitive marker for neuronal injury or loss (Suskauer and Huisman 2009; Burtscher and Holtås 2001; Lin and Rothman 2014; Gardner et al. 2014; Mountford et al. 2010). Choline (Cho), an umbrella term for different molecular components of fluid-mosaic cell membranes, can be used as marker for synthesis and degradation of membranes. Choline levels are positively related to cell membrane turnover and increase when neuroglial injury is present (Suskauer and Huisman 2009; Burtscher and Holtås 2001; Danielsen and Ross 1999; Lin and Rothman 2014). Phosphocreatine (Pcr) is a crucial component of ATP synthesis and is used together with creatine (Cr) as marker for brain metabolism and energy levels. Creatine is produced in the kidney and liver; it is transported through the bloodstream and is taken up by tissues with high metabolic rates, such as the brain and skeletal muscle. Metabolite/creatine ratios have been widely used to describe pathological conditions because of their relatively stable reproducibility (Suskauer and Huisman 2009; Danielsen and Ross 1999). Lactate (Lact) levels are increased in any condition that stimulates anaerobic metabolism and can therefore be used to determine if inflammation or tissue injury is present. Lactate is not found in the spectrum of healthy individuals (Byrnes et al. 2014; Suskauer and Huisman 2009; Burtscher and Holtås 2001; Danielsen and Ross 1999; 77). Myoinositol (mI) has been shown to be a marker for astrocytes; this metabolite tends to be increased in low-grade astrocytomas (Burtscher and Holtås 2001; Danielsen and Ross 1999; 77). Glutamate and glutamine are essential metabolites of the citric acid cycle and therefore their concentration can change in metabolic disorders (Burtscher and Holtås 2001; Danielsen and Ross 1999). It is important to know that, with the exception of creatine, the concentrations of these metabolites vary across different brain areas (Burtscher and Holtås 2001; Danielsen and Ross 1999; Baker et al. 2008).
Some distinct changes can be observed in the healthy aging brain. With aging, as the number and diameter of large neurons decreases, levels of NAA fall concordantly. At the same time mitochondrial metabolism increases by up to 30 %, causing a rise of mI (Lin and Rothman 2014; Esopenko and Levine 2015). Levels of NAA and NAA/Cr ratio also decrease in patients with Alzheimer’s disease (AD) and other dementias, faster than in elderly individuals without any cognitive impairment. Changes in biomarker levels can be related to clinical changes. This is an important finding, since chronic traumatic encephalopathy (CTE) shares some features with AD, as discussed above (Burtscher and Holtås 2001; Haga et al. 2009; Kantarci et al. 2007; Lin et al. 2003; Zhang et al. 2014). However, antipodal changes of Cho/Cr ratios in individuals who suffer from AD have been reported also (Burtscher and Holtås 2001; Haga et al. 2009; Kantarci et al. 2007; Zhang et al. 2014). Also, the NAA/mI ratio has been shown to decrease in patients with mild cognitive impairment (Burtscher and Holtås 2001; Haga et al. 2009; Kantarci et al. 2007; Lin et al. 2003; Zhang et al. 2014).
Several studies have shown that, in patients with mild traumatic brain injury (mTBI) or concussion, NAA concentrations are lower (in the acute phase) than in healthy controls (Chamard et al. 2012; Cimatti 2006; Davie et al. 1995; Henry et al. 2010, 2011a, b; Johnson et al. 2012a, b; Kirov et al. 2013; Vagnozzi et al. 2008, 2010, 2013). However, in one study among children aged 11 to 15 with sports-related concussion, the authors could not find any metabolic changes on 1H-MRS (Maugans et al. 2012). Also, other investigators have reported equivocal findings (Cimatti 2006). Additional changes observed in patients post-mTBI or postconcussion included decrease of glutamate levels, decrease of AA/CR ratio, decrease of NAA/Cho ratio, increase in the Cho/Cr ratio, and increase of mI/Cr ratio in the chronic phase (Henry et al. 2010, 2011a, b; Vagnozzi et al. 2010, 2013). Two studies (from the same group of authors) found that increased NAA/Cho and NAA/Cr ratios correlated with the number of mTBIs (Johnson et al. 2012a, b). In one study with concussed athletes, correlation between metabolic changes and self-reported symptom severity was documented, though neuropsychiatric assessment could not replicate these findings (Henry et al. 2010). These different and conflicting study results may be explained by the use of various echo times, low spectral resolution, the generally small number of subjects in many studies, and the variability of time that had elapsed between injury and scan (Duarte et al. 2012).
Metabolic abnormalities seem to outlast clinical symptoms. A longitudinal follow-up study on female ice-hockey players found remaining post-seasonal decrease of NAA/Cr ratio postconcussion; however, male players who had sustained a concussion during the season did not show any lasting changes of the metabolic spectrum (Chamard et al. 2012). One study performed diffusion tensor imaging (DTI) and 1H-MRS in healthy individuals, demonstrating a positive correlation between fractional anisotropy (FA) and concentrations of NAA (Cheng et al. 2014).
In summary, a decrease of NAA and the NAA/Cr ratio has been observed postconcussion in sports-induced injuries. These changes appear to be similar to those seen in individuals with AD.
8.8 Diffusion Tensor Imaging (DTI) Opens a Window on the Microstructural Environment of the Brain
In the middle 1980s, visionary MRI scientists predicted that magnetic resonance imaging (MRI) could be used to provide information about molecular diffusion in tissues. The practical implementation was initially hampered by hardware limitations, but by the late 1990s a workable diffusion-weighted imaging (DWI) sequence became available for routine brain imaging. In DWI images, the intensity of each voxel reflects the magnitude (or rate) of water diffusion in that specific location. Diffusion-weighted sequences measure the magnitude of free water diffusion in tissues, but do not yield directional information.
However, these images not only represent “true” diffusion, but also include other confounders such as perfusion effects or T2 shine-through phenomena. To eliminate such influences, the concept of the apparent diffusion coefficient (ADC) was introduced. This parameter can be expressed in parametric ADC maps, representing the observed (“apparent”) diffusion in a particular voxel. The degree to which a sequence is sensitive to diffusion is expressed by the “b-value,” expressed in s/mm2. The higher the “b-value,” the more the signal intensity reflects “true” tissue water diffusion changes. In DWI, the diffusion gradients are applied in three orthogonal directions; this allows an estimation of the “trace,” which is an indicator of the average diffusivity. Trace-weighted diffusion images initially found their main area of application in neurological disorders, especially for the early detection of the cytotoxic edema associated with acute ischemic stroke. Since about 15 years ago, DWI has become a crucial part of routine clinical MRI examinations of the brain and, increasingly, also other organs.
However, diffusion in white matter of the brain is known to be anisotropic and depends on the orientation of axonal fibers. This observation led to the development of a sequence that could measure, at a microstructural level, not only the magnitude of diffusion, but also the direction or path of diffusion. In this way diffusion tensor imaging (DTI) was born. In order to obtain the directional information, which is essential for DTI, diffusion gradients need to be applied in at least six directions and preferably more. This technique provides an insight into the internal microstructural organization of the brain. From the acquired DTI data, metrics such as fractional anisotropy (FA) and mean diffusivity (MD) can be derived; parametric images can be reconstructed which reflect the fraction of the diffusion tensor that is attributable to anisotropic diffusion. FA values are between zero and one, with higher values standing for a more uniform directionality of diffusion.
FA and ADC can be assessed using different analyzing methods. In a whole-brain distributional analysis, DTI parameters are created for every voxel of the brain. This approach calculates averaged values of changes in FA and ADC across the brain which might blur the overall picture, since spatial information might be lost. A second possibility is the employment of whole-brain voxel-based analysis. Hereby data sets are aligned to anatomical structures to increase spatial resolution. In region-of-interest (ROI)-based analysis, groups of voxels in specific regions are averaged and checked against each other. This allows an even better spatial resolution; however, it is a rather work-intensive process which might be confounded by preferences of the examiner. In vivo tractography allows to obtain data sets for specific white matter tracts, thereby raising specificity, validity, and spatial resolution of results (Dimou and Lagopoulos 2014; Moritani et al. 2009; Gardner et al. 2012).
In patients with TBI, it has been hypothesized that a decrease of FA represents anterograde degeneration, axonal injury, and demyelinization, whereas an increase is anticipated in the presence of cytotoxic edema. ADC values usually change in negative concordance with FA.
TBI has been associated with DAI and traumatic axonal injury, respectively, which can be visualized using DTI (Henry et al. 2011a, b; Moritani et al. 2009; Meythaler et al. 2001; Xu et al. 2007). These cellular injuries occur when shearing forces are applied to neurons as it occurs during concussion (Moritani et al. 2009; Meythaler et al. 2001; Slobounov et al. 2012). Trauma to axons causes disruption of axonal transport and therefore accumulation of metabolites leading to axonal edema. However, primary axostomy is rarely seen, though the subsequent swelling of axons can cause secondary axostomy which is much more common than primary anatomical disruption. It is therefore assumed that most of the damage occurs intra-axonal to the cytoskeleton while the outer membrane may still be intact. Later ionic imbalance, uncontrolled glutamate release, and oxidative stress are detrimental and may aggravate cytotoxic edema. Post-injury amyloid precursors accumulate which may be released in case of axonal lysis or apoptosis, having a theoretical potential to contribute to neurodegenerative diseases (Moritani et al. 2009; Meythaler et al. 2001; Johnson et al. 2013).
In the early stages after TBI, the most prominent findings are decreased FA and increased ADC values, representing damage to axons and mixed intra- and extracellular edema (Moritani et al. 2009; Xu et al. 2007). However, more recently those findings have been challenged suggesting there could be an increase of FA in the acute phase (Eierud et al. 2014). A decrease of ADC without any change of FA may be caused by edema without any physical disruption of axons. In the subacute phase a decrease of FA and increase of ADC represent progressive repair of nerve fibers (Slobounov et al. 2012; Inglese et al. 2005; Kumar et al. 2009a, b; Niogi and Mukherjee 2010; Sidaros et al. 2008). In mouse models, demyelination (which can be a feature of TBI as described above) presents as increased radial diffusion (RD) (Song et al. 2002). In humans decrease in FA and increase in mean diffusivity (MD) represent post-traumatic demyelination and gliosis (Kumar et al. 2009a, b). However, the differences in reported FA, ADC, and MD values could also be explained by the variability in research protocols across different studies and the disregard of the factor time in the healing process and its implication on repair-induced changes of diffusity. Other technical factors in the acquisition (number of DTI images, spatial resolution) may influence the validity of results and could explain the great variety of findings (Eierud et al. 2014; Dodd et al. 2014; Farbota et al. 2012; Shenton et al. 2012; Xiong et al. 2014).
Since the late 1990s a huge increase in interest on TBI has occurred and several meta-analysis and reviews have attempted to find a common spatial pattern of diffusivity alteration post-(m)TBI across all published studies. (Pre)frontal areas seem to be more vulnerable to TBI; however, the mechanism of injury might be a huge determinant of location of injury. Injury to the corpus callosum and in particular its anterior parts, rostrum and genu, have been reported frequently. Minor and less frequently reported injuries post-TBI have been demonstrated almost all over the brain. Though those data might appear to be random, they all support the presence of subtle post-TBI alterations (Eierud et al. 2014; Dodd et al. 2014; Shenton et al. 2012; Xiong et al. 2014).
Gardner et al. conducted a review of literature focusing specifically on postconcussional DTI findings in athletes (mostly boxers) (Gardner et al. 2012). In sports-related concussion (SRC) a tendency of increased ADC was observed with anatomical foci in the corpus callosum, internal capsule, and inferior and superior fasciculus. Nevertheless, not all studies included in this review supported these observations, and therefore, overly enthusiastic interpretation should be avoided (Gardner et al. 2012). However, increases in FA in the corpus callosum post-SRC have been reported also (Henry et al. 2011a, b). In soccer players increased axial diffusity (AD) in the corpus callosum and diffuse increase of radial diffusity (RD) in various brain regions have been shown (Koerte et al. 2012). Moreover, DTI has been proven to be more sensitive than MRI in diagnosing sports-related mTBI. Especially, in clinically asymptomatic patients post-mTBI with normal MRI or aspecific MRI findings, changes suggestive for mTBI can be demonstrated on DTI (Mendez et al. 2005; Henry et al. 2011a, b; Chappell et al. 2006; Green et al. 2010; Zhang et al. 2003, 2006, 2010a, b).
Looking at the prognosis of TBI, higher FA values have been associated with better functional outcome, whereas low MD predicted rather poor outcome (Bazarian et al. 2007; Betz et al. 2012; Ewing-Cobbs et al. 2008; Irimia et al. 2012; Kumar et al. 2009a, b; Ljungqvist et al. 2011; Messé et al. 2011; Sidaros et al. 2008; Strangman et al. 2012; Wilde et al. 2006; Yuh et al. 2014). However, no evidence has been found linking FA, ADC, or MD to the common phenomenon of post-TBI depression (Maller et al. 2010). In the future, diffusion kurtosis imaging (DKI) might supplement DTI, allowing even more precise outcome prediction. Mean kurtosis (MK) in particular has been related to chronic cerebral damage and permanent cognitive sequelae (Grossman et al. 2012).
8.9 Functional Magnetic Resonance Imaging (fMRI)
Blood oxygen level-dependent functional magnetic resonance imaging (BOLD fMRI) is used to visualize local distribution of oxyhemoglobin and deoxyhemoglobin levels in the brain, with oxyhemoglobin leading to higher signal intensity. Increase in neuronal activity requires more oxygen, and through the mechanism of neurovascular coupling, a higher BOLD signal represents areas of increased metabolism and therefore areas of increased neuronal activity (Slobounov et al. 2012). In postconcussion test subjects, who were asked to perform cognitive tasks, some authors have observed an increased BOLD signal, primarily in the frontal cortex, with the most reproducible results being seen in the dorsolateral prefrontal cortex, which plays an important role in activation and modulation of working memory (McAllister et al. 1999). Similar changes have been observed in retired professional football players of the National Football League (Hampshire et al. 2013). Longitudinal studies of high school football players have revealed increased activation of the dorsolateral prefrontal cortex in those without clinical symptoms in contrast to those players with clinically confirmed impairment, who showed an increased activation of the temporal lobe (Breedlove et al. 2012; Talavage et al. 2014). Generally, across several studies, the frontal areas of the brain appear to be more vulnerable to concussion than others (Slobounov et al. 2012; Eierud et al. 2014). These changes might be due to concussional damage, requiring increased activation to perform normal tasks, a theory termed neural insufficiency (Chang et al. 2004; Chiaravalloti et al. 2005; Hillary et al. 2003; Perlstein et al. 2004). Different explanations for the increased recruitment have been proposed, from brain reorganization, over neural compensation, to the latent support hypothesis (Slobounov et al. 2012; Eierud et al. 2014). However, contradicting results of decreased activation have been reported also, first by a research group around Chen et al. (Chen et al. 2007, 2008; Mayer et al. 2009).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree