Fig. 16.1
Coronal (a) and sagittal (b) trans-perineal scans performed in a 36-year old patient with severe perianal pain show a small abscess of the crypt at the level of the dentate line (arrows). The symptoms and the lesion disappeared following systemic antibiotic treatment
Treatment relies on local hygiene and systemic antibiotics. However, while in the pediatric population this approach, even without surgical drainage, can minimize the formation of fistula-in-ano, in adults surgical revision may be required to avoid fistula formation [1, 2].
16.2 Perianal Hidradenitis Suppurativa
Hidradenitis suppurativa is a chronic skin disorder affecting areas rich in apocrine glands. It is characterized by the occurrence of boils in the affected sites that gradually enlarge and rupture, with heavy purulence. Hidradenitis suppurativa has a point prevalence of up to 4.1% and is more common in females.
The pathogenesis of this disease is unknown, although genetic factors, hormones, and infection have been implicated. An association with Crohn’s disease and arthropathy has also been reported [3, 4].
The perineum is one of the most frequently affected sites, along with the axilla and groin, due to the high density of follicular structures in this area. Disease onset is insidious. Initially, individuals may experience slight discomfort or pruritus in the affected area. Subsequently, a tender papule or deep-seeded nodule develops. While this nodule may slowly resolve, it often expands and coalesces with surrounding nodules to form large, painful inflammatory abscesses that may rupture spontaneously, yielding a purulent discharge. The lesion then heals with fibrosis, dermal contractures, and rope-like elevation of the skin, and double-ended comedones. Sinus tracts may also develop.
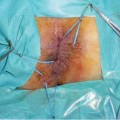
Therapy of hidradenitis suppurativa consists primarily of systemic antibiotics and topical antiseptics. Surgical removal of all involved tissue, beyond the clinically involved margins, is the most effective treatment strategy. However, postoperative recurrences are not uncommon. In such cases, ultrasonography can be useful in surgical planning. Ultrasound, performed with high-resolution 7- to 12-MHz linear transducers coupled with color Doppler, reveals hypoechoic areas reflecting edema and inflamed tissue not only of the skin but also of the subcutaneous tissue (Fig. 16.2). Vascularity and a resistance index (RI) typically > 0.40 characterize severe lesions. Usually, these changes are more widespread than expected from clinical examination and the changes visible on ultrasound always extend beyond the clinically identified borders of the lesions [5, 6].
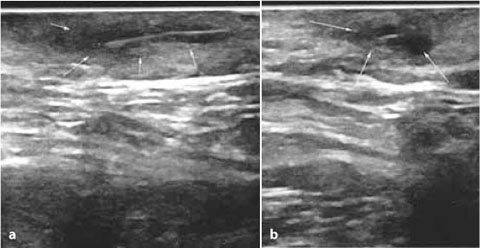
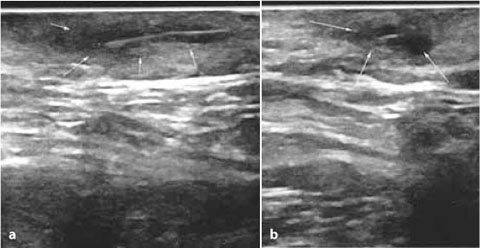
Fig. 16.2
Longitudinal (a) and transversal (b) scan of a circumscribed hypoechoic and vascularized lesion in the dermal layer (arrows), reflecting edema and inflamed tissue in a 32-year-old woman with recurrent perianal hidradenitis suppurativa
16.3 Anal Tuberculosis
Anoperineal tuberculosis (TB) is an exceedingly rare extrapulmonary form of the disease (1% of digestive tract incidence) that must be recognized because it requires specific treatment. Anoperineal TB is most common in men (77–100% of cases) and occurs secondary to a primary site in the lungs. Anal contamination is usually caused by the swallowing of respiratory secretions that contain a large quantity of Koch’s bacillus. A pre-existing anal lesion (fissure, erosion, fistula, pilonidal sinus, or scar) is often found [7].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree