Chapter 25 Recognizing Some Common Causes of Intracranial Pathology
 Advances in neuroimaging have had a remarkable impact on the diagnosis and treatment of neurologic diseases ranging from earlier detection and treatment of stroke to a more timely diagnosis of dementia, from the rapid detection and treatment of cerebral aneurysms to the ability to diagnose multiple sclerosis after a single attack.
Advances in neuroimaging have had a remarkable impact on the diagnosis and treatment of neurologic diseases ranging from earlier detection and treatment of stroke to a more timely diagnosis of dementia, from the rapid detection and treatment of cerebral aneurysms to the ability to diagnose multiple sclerosis after a single attack. Both CT and MRI are utilized for studying the brain and spinal cord, but MRI is the study of first choice for most clinical scenarios (Table 25-1). Conventional radiography has no significant role in imaging intracranial abnormalities.
Both CT and MRI are utilized for studying the brain and spinal cord, but MRI is the study of first choice for most clinical scenarios (Table 25-1). Conventional radiography has no significant role in imaging intracranial abnormalities.TABLE 25-1 IMAGING STUDIES OF THE BRAIN FOR SELECTED ABNORMALITIES
| Abnormality | Study of First Choice | Other Studies |
|---|---|---|
| Acute stroke | Diffusion-weighted MR imaging for acute or small strokes, if available | Noncontrast CT can differentiate hemorrhagic from ischemic infarct |
| Headache, acute and severe | Noncontrast CT to detect subarachnoid hemorrhage | MR-angiography (MRA) or CT-angiography (CTA) if subarachnoid hemorrhage is found |
| Headaches, chronic | MRI without and with contrast | CT without and with contrast can be substituted |
| Seizures | MRI without and with contrast | CT without and with contrast can be substituted if MRI not available |
| Blood | Noncontrast CT | Ultrasound for infants |
| Head trauma | Nonenhanced CT is readily available and the study of first choice in head trauma | MRI is better at detecting diffuse axonal injury but requires more time and is not always available |
| Extracranial carotid disease | Doppler ultrasonography | MRA excellent study |
| Hydrocephalus | MRI as initial study | CT for follow-up |
| Vertigo and dizziness | Contrast-enhanced MRI | MRA if needed |
| Masses | Contrast-enhanced MRI | Contrast-enhanced CT if MRI not available |
| Change in mental status | MRI without or with contrast | CT without contrast is equivalent |
Normal Anatomy
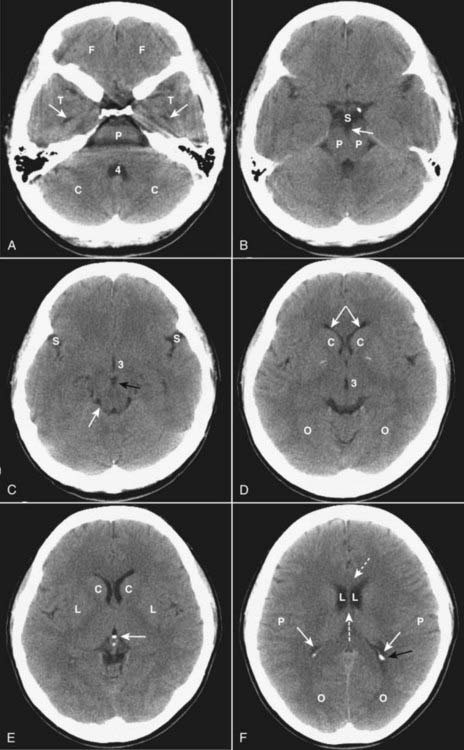
 In the posterior fossa, the 4th ventricle appears as an inverted U-shaped structure. Like all cerebrospinal fluid (CSF) containing structures, it normally appears black. Superior to the 4th ventricle are the cerebellar hemispheres, inferiorly lie the pons and medulla oblongata. The tentorium cerebelli separates the infratentorial components of the posterior fossa (medulla, pons, cerebellum, and 4th ventricle) from the supratentorial compartment.
In the posterior fossa, the 4th ventricle appears as an inverted U-shaped structure. Like all cerebrospinal fluid (CSF) containing structures, it normally appears black. Superior to the 4th ventricle are the cerebellar hemispheres, inferiorly lie the pons and medulla oblongata. The tentorium cerebelli separates the infratentorial components of the posterior fossa (medulla, pons, cerebellum, and 4th ventricle) from the supratentorial compartment. The interpeduncular cistern lies in the midbrain and separates the paired cerebral peduncles (which emerge from the superior surface of the pons). The suprasellar cistern is anterior to the interpeduncular cistern and usually has a five-point or six-point starlike appearance.
The interpeduncular cistern lies in the midbrain and separates the paired cerebral peduncles (which emerge from the superior surface of the pons). The suprasellar cistern is anterior to the interpeduncular cistern and usually has a five-point or six-point starlike appearance. The sylvian fissures are bilaterally symmetrical and contain CSF. They separate the temporal from the frontal and parietal lobes.
The sylvian fissures are bilaterally symmetrical and contain CSF. They separate the temporal from the frontal and parietal lobes. The lentiform nucleus is composed of the putamen (laterally) and globus pallidus (medially). The 3rd ventricle is slitlike and midline. At the posterior aspect of the 3rd ventricle is the pineal gland. Farther posterior is the quadrigeminal plate cistern.
The lentiform nucleus is composed of the putamen (laterally) and globus pallidus (medially). The 3rd ventricle is slitlike and midline. At the posterior aspect of the 3rd ventricle is the pineal gland. Farther posterior is the quadrigeminal plate cistern. The corpus callosum connects the right and left cerebral hemispheres and forms the roof of the lateral ventricle. The anterior end is called the genu and the posterior end is called the splenium.
The corpus callosum connects the right and left cerebral hemispheres and forms the roof of the lateral ventricle. The anterior end is called the genu and the posterior end is called the splenium. The basal ganglia are represented by the subthalamic nucleus, substantia nigra, globus pallidus, putamen, and caudate nucleus. The putamen and caudate nucleus are called the striatum.
The basal ganglia are represented by the subthalamic nucleus, substantia nigra, globus pallidus, putamen, and caudate nucleus. The putamen and caudate nucleus are called the striatum. The frontal horns of the lateral ventricles hug the head of the caudate nucleus. The two frontal horns are separated by the midline septum pellucidum. The temporal horns, which are normally very small, are more inferior and contained in the temporal lobes. The posterior horns of the lateral ventricle (occipital horns) lie in the occipital lobes. The most superior portion of the ventricular system is formed by the bodies of the lateral ventricles.
The frontal horns of the lateral ventricles hug the head of the caudate nucleus. The two frontal horns are separated by the midline septum pellucidum. The temporal horns, which are normally very small, are more inferior and contained in the temporal lobes. The posterior horns of the lateral ventricle (occipital horns) lie in the occipital lobes. The most superior portion of the ventricular system is formed by the bodies of the lateral ventricles. The falx cerebri lies in the interhemispheric fissure, which separates the two cerebral hemispheres, and is frequently calcified in adults.
The falx cerebri lies in the interhemispheric fissure, which separates the two cerebral hemispheres, and is frequently calcified in adults. The surface or cortex of the brain is made up of gray matter convolutions, which in turn are composed of sulci (grooves) and gyri (elevations). The medullary white matter lies below the cortex.
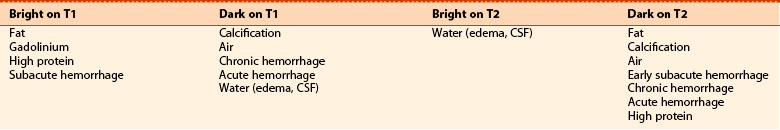
The surface or cortex of the brain is made up of gray matter convolutions, which in turn are composed of sulci (grooves) and gyri (elevations). The medullary white matter lies below the cortex.![]() On an unenhanced CT scan of the brain, anything that appears “white” will generally either be bone (calcium) density or blood in the absence of a metallic foreign body (Table 25-2).
On an unenhanced CT scan of the brain, anything that appears “white” will generally either be bone (calcium) density or blood in the absence of a metallic foreign body (Table 25-2).
 Metallic densities in the head can cause artifacts on CT scans. Dental fillings, aneurysm clips, and bullets can all cause streak artifacts.
Metallic densities in the head can cause artifacts on CT scans. Dental fillings, aneurysm clips, and bullets can all cause streak artifacts.| Hypodense (Dark) (AKA Hypointense) | Isodense | Hyperdense (Bright) (AKA Hyperintense) |
|---|---|---|
| Fat (not usually present in the head) Air (e.g., sinuses) Water (e.g., CSF) | Normal brain Some forms of protein (e.g., subacute subdural hematomas) | Metal (e.g., aneurysm clips or bullets) Iodine (after contrast administration) Calcium Hemorrhage (high protein) |
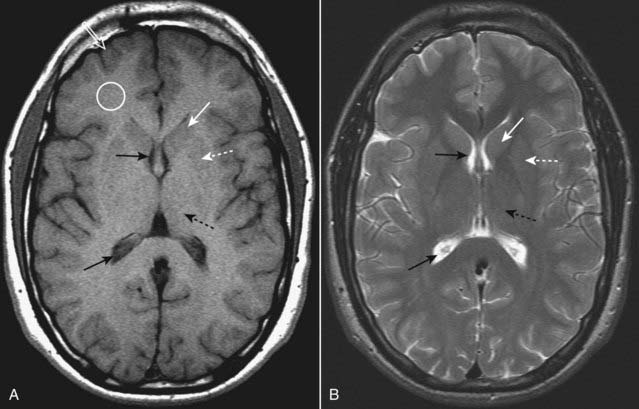
Mri and the Brain
 MRI is more difficult to interpret because the same structure or abnormality will appear differently depending on the pulse sequence, the scan parameters, and the fact that MRI is more variable in its depiction of differences which occur over the time course of some abnormalities (e.g., hemorrhage) than is CT.
MRI is more difficult to interpret because the same structure or abnormality will appear differently depending on the pulse sequence, the scan parameters, and the fact that MRI is more variable in its depiction of differences which occur over the time course of some abnormalities (e.g., hemorrhage) than is CT. Initial evaluation of an MRI of the brain might start with the T1-weighted sagittal view of the brain. On this view the brain looks more like the anatomic specimens or diagrams you are accustomed to looking at (Fig. 25-3). We are fortunate that many structures in the brain are paired, so don’t forget to compare one side to the other on axial scans of the brain (Fig. 25-4).
Initial evaluation of an MRI of the brain might start with the T1-weighted sagittal view of the brain. On this view the brain looks more like the anatomic specimens or diagrams you are accustomed to looking at (Fig. 25-3). We are fortunate that many structures in the brain are paired, so don’t forget to compare one side to the other on axial scans of the brain (Fig. 25-4).Head Trauma
 Traumatic brain injuries extract a huge cost to the patient and society, not only as a result of the acute injury but also for the long-term disability they produce. In the United States, motor vehicle accidents account for nearly half of traumatic brain injuries.
Traumatic brain injuries extract a huge cost to the patient and society, not only as a result of the acute injury but also for the long-term disability they produce. In the United States, motor vehicle accidents account for nearly half of traumatic brain injuries. Unenhanced CT is the study of choice in acute head trauma. The primary goal in obtaining the scan is to determine if there is a life-threatening, but treatable, lesion.
Unenhanced CT is the study of choice in acute head trauma. The primary goal in obtaining the scan is to determine if there is a life-threatening, but treatable, lesion. To determine if there is mass effect, look for a displacement or compression of key structures from their normal positions by analyzing the location and appearance of the ventricles, basal cisterns and the sulci.
To determine if there is mass effect, look for a displacement or compression of key structures from their normal positions by analyzing the location and appearance of the ventricles, basal cisterns and the sulci. Blood will usually be hyperintense (bright) and might collect in the basal cisterns, sylvian and interhemispheric fissures, ventricles, the subdural or epidural spaces, or in the brain parenchyma (intracerebral).
Blood will usually be hyperintense (bright) and might collect in the basal cisterns, sylvian and interhemispheric fissures, ventricles, the subdural or epidural spaces, or in the brain parenchyma (intracerebral).Skull Fractures
 Skull fractures are usually produced by direct impact to the skull and they most often occur at the point of impact. They are important primarily because their presence implies a force substantial enough to cause intracranial injury.
Skull fractures are usually produced by direct impact to the skull and they most often occur at the point of impact. They are important primarily because their presence implies a force substantial enough to cause intracranial injury. In order to visualize skull fractures, you must view the CT scan using the “bone window” settings that optimize visualization of the osseous structures (Fig. 25-5).
In order to visualize skull fractures, you must view the CT scan using the “bone window” settings that optimize visualization of the osseous structures (Fig. 25-5). Skull fractures can be described as linear, depressed, or basilar.
Skull fractures can be described as linear, depressed, or basilar.• Linear skull fractures are the most common and have little importance other than for the intracranial abnormalities that may have occurred at the time of the fracture, such as an epidural hematoma. Fractures of the cranial vault are most likely to occur in the temporal and parietal bones (see Fig. 25-5B).
• Depressed skull fractures are more likely to be associated with underlying brain injury. They result from a high-energy blow to a small area of the skull (e.g., from a baseball bat), most often in the frontoparietal region and are usually comminuted. They may require surgical elevation of the depressed fragment when the fragment lies deeper than the inner table adjacent to the fracture (Fig. 25-6A).
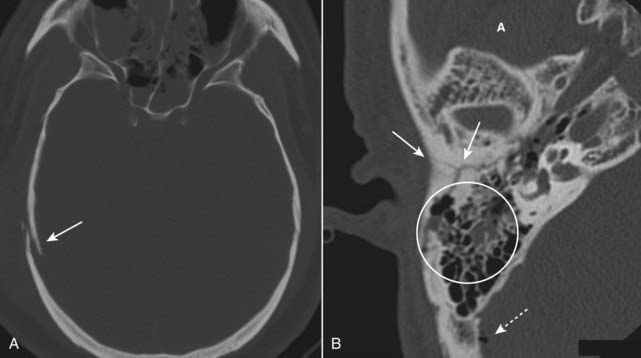
![]() Basilar skull fractures are the most serious and consist of a linear fracture at the base of the skull. They can be associated with tears in the dura mater with subsequent CSF leak, which can lead to CSF rhinorrhea and otorrhea. They can be suspected if there is air seen in the brain (traumatic pneumocephalus), fluid in the mastoid air cells, or an air-fluid level in the sphenoid sinus (Fig. 25-6B).
Basilar skull fractures are the most serious and consist of a linear fracture at the base of the skull. They can be associated with tears in the dura mater with subsequent CSF leak, which can lead to CSF rhinorrhea and otorrhea. They can be suspected if there is air seen in the brain (traumatic pneumocephalus), fluid in the mastoid air cells, or an air-fluid level in the sphenoid sinus (Fig. 25-6B).
Facial Fractures
 CT is the imaging study of choice for evaluating facial fractures. Multislice scanners allow for reconstruction in the coronal plane so the patient does not have to be repositioned in the scanner.
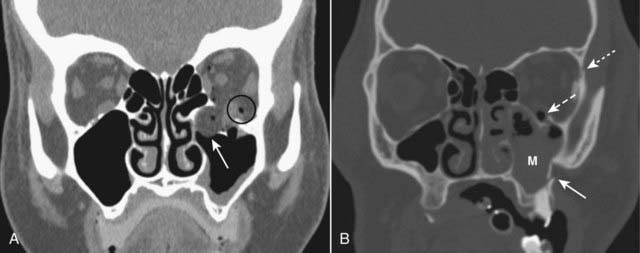
CT is the imaging study of choice for evaluating facial fractures. Multislice scanners allow for reconstruction in the coronal plane so the patient does not have to be repositioned in the scanner. The most common orbital fracture is the blow-out fracture, which is produced by a direct impact on the orbit (e.g., a baseball strikes the eye) that causes a sudden increase in intraorbital pressure leading to a fracture of the inferior orbital floor (into the maxillary sinus) or the medial wall of the orbit (into the ethmoid sinus). Sometimes, the inferior rectus muscle can be trapped in the fracture leading to restriction of upward gaze and diplopia.
The most common orbital fracture is the blow-out fracture, which is produced by a direct impact on the orbit (e.g., a baseball strikes the eye) that causes a sudden increase in intraorbital pressure leading to a fracture of the inferior orbital floor (into the maxillary sinus) or the medial wall of the orbit (into the ethmoid sinus). Sometimes, the inferior rectus muscle can be trapped in the fracture leading to restriction of upward gaze and diplopia. Recognizing a blow-out fracture of the orbit (Fig. 25-7A).
Recognizing a blow-out fracture of the orbit (Fig. 25-7A).• Orbital emphysema. Air in the orbit from communication with one of the adjacent air-containing sinuses, either the ethmoid or maxillary sinus.
• Entrapment of fat and/or extraocular muscle, which projects downward as a soft tissue mass into the top of the maxillary sinus.
 A tripod fracture, usually a result of blunt force to the cheek, is another relatively common facial fracture. This fracture involves separation of the zygoma from the remainder of the face by separation of the frontozygomatic suture, fracture of the floor of the orbit, and fracture of the lateral wall of the ipsilateral maxillary sinus (Fig. 25-7B).
A tripod fracture, usually a result of blunt force to the cheek, is another relatively common facial fracture. This fracture involves separation of the zygoma from the remainder of the face by separation of the frontozygomatic suture, fracture of the floor of the orbit, and fracture of the lateral wall of the ipsilateral maxillary sinus (Fig. 25-7B).Intracranial Hemorrhage
Epidural Hematoma (Extradural Hematoma)
 Epidural hematomas represent hemorrhage into the potential space between the dura mater and the inner table of the skull (Table 25-4).
Epidural hematomas represent hemorrhage into the potential space between the dura mater and the inner table of the skull (Table 25-4). Most cases are due to injury to the middle meningeal artery or vein from blunt head trauma, typically from a motor vehicle accident.
Most cases are due to injury to the middle meningeal artery or vein from blunt head trauma, typically from a motor vehicle accident.| Layer | Comments |
|---|---|
| Dura mater | Composed of two layers, an outer periosteal layer which cannot be separated from the skull and an inner meningeal layer; the inner meningeal layer enfolds to form the tentorium and falx. |
| Arachnoid | The avascular middle layer, it is separated from the dura by a potential space known as the subdural space. |
| Pia mater | Closely applied to the brain and spinal cord, the pia mater carries blood vessels that supply both; separating the arachnoid from the pia is the subarachnoid space; together the pia and arachnoid are called the leptomeninges. |
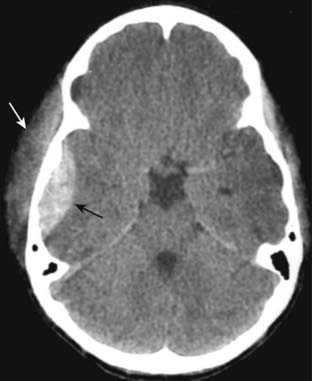
 Recognizing an epidural hematoma
Recognizing an epidural hematoma• They appear as a high density, extraaxial, biconvex lens-shaped mass most often found in the temporoparietal region of the brain (Fig. 25-8).
• Since the dura is normally fused to the calvarium at the margins of the sutures, it is impossible for an epidural hematoma to cross suture lines (subdural hematomas can cross sutures).
Subdural Hematoma (SDH)
 Subdural hematomas are more common than epidural hematomas and are usually not associated with a skull fracture. They are most commonly a result of deceleration injuries in motor vehicle or motorcycle accidents (younger patients) or secondary to falls (older patients).
Subdural hematomas are more common than epidural hematomas and are usually not associated with a skull fracture. They are most commonly a result of deceleration injuries in motor vehicle or motorcycle accidents (younger patients) or secondary to falls (older patients). Subdural hematomas are usually produced by damage to the bridging veins that cross from the cerebral cortex to the venous sinuses of the brain. They represent hemorrhage into the potential space between the dura mater and the arachnoid.
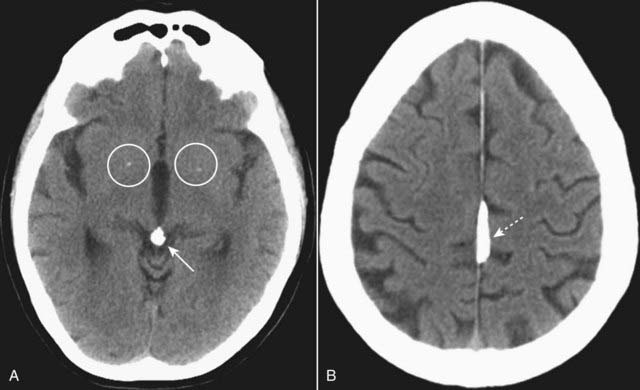
Subdural hematomas are usually produced by damage to the bridging veins that cross from the cerebral cortex to the venous sinuses of the brain. They represent hemorrhage into the potential space between the dura mater and the arachnoid. Recognizing an acute subdural hematoma
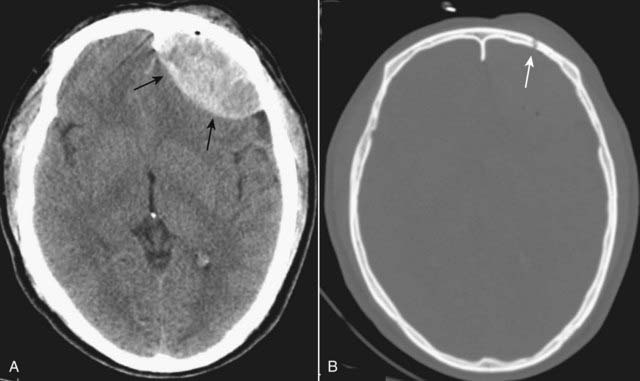
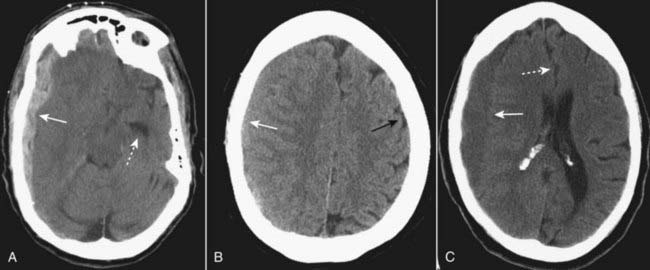
Recognizing an acute subdural hematoma• On CT, acute subdural hematomas are crescent-shaped, extracerebral bands of high attenuation that may cross suture lines and enter the interhemispheric fissure. They do not cross the midline.
• Typically, a SDH is concave inward towards the brain (epidural hematomas are convex inward) (Fig. 25-9A).
• As time passes and they become subacute, or if the subdural blood is mixed with lower attenuating CSF, they may appear isointense (isodense) to the remainder of brain, in which case you should look for compressed or absent sulci or sulci displaced away from the inner table as signs of SDH (Fig. 25-9B).
Intracerebral Hematoma (Intracerebral Hemorrhage)
 Trauma is only one of the mechanisms that can lead to intracerebral hemorrhage. Intracerebral hematomas can also occur from ruptures of aneurysms, atheromatous disease in small vessels, or vasculitis.
Trauma is only one of the mechanisms that can lead to intracerebral hemorrhage. Intracerebral hematomas can also occur from ruptures of aneurysms, atheromatous disease in small vessels, or vasculitis. Injuries occurring at the point of impact (called coup injuries) and injuries occurring opposite the point of impact (called contrecoup injuries) are most common following trauma. Coup injuries are most often due to shearing of small intracerebral vessels. Contrecoup injuries are acceleration/deceleration injuries that occur when the brain is propelled in the opposite direction and strikes the inner surface of the skull.
Injuries occurring at the point of impact (called coup injuries) and injuries occurring opposite the point of impact (called contrecoup injuries) are most common following trauma. Coup injuries are most often due to shearing of small intracerebral vessels. Contrecoup injuries are acceleration/deceleration injuries that occur when the brain is propelled in the opposite direction and strikes the inner surface of the skull.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree