Fig. 23.1
“Sloppy lateral” position for insertion of bilateral paravertebral nerve block catheters
Step-by-Step Technique
The appropriate thoracic level is identified using landmarks and marked. The ultrasound probe is placed in a transverse orientation over the midline of the back at the designated dermatomal level and the spinous process identified by the characteristic hyperechoic inverted V shape with an acoustic shadow beneath. The probe is moved lateral and rotated to a slightly oblique orientation (lateral probe edge slightly caudal) until the tip of the TP is seen in the same view as the parietal pleura (Fig. 23.2). The internal intercostal membrane (IICM), the membranous extension of the internal intercostals muscle, is identified as a hyperechoic structure connecting the edge of the internal intercostal muscles to the lower edge of the TP (Fig. 23.3).

Fig. 23.2
Lateral and slightly oblique orientation of probe for paravertebral blocks
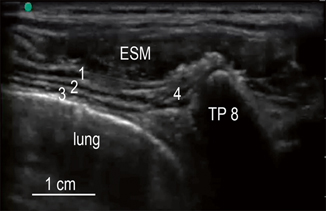
Fig. 23.3
Ultrasound anatomy of paravertebral nerve block: 1 external intercostal muscle; 2 internal intercostal muscle; 3 innermost intercostal muscle; 4 internal intercostal membrane (IICM). ESM erector spinae muscle, TP8 8th transverse process
An echogenic needle is introduced, bevel up and in-plane, at the lateral edge of the probe and advanced from lateral to medial until the needle tip is through the IICM in the space between the parietal pleura and the acoustic shadow of the overlying TP (Fig. 23.4). Correct position within the PVB space is confirmed by real-time ultrasound visualization of anterior displacement of the pleura with an injection of a few milliliter of saline solution (Fig. 23.5). Once the paravertebral space is identified, and after a negative aspiration for blood and CSF, local anesthetic is injected.

Fig. 23.4
Lateral to medial needle orientation for paravertebral block
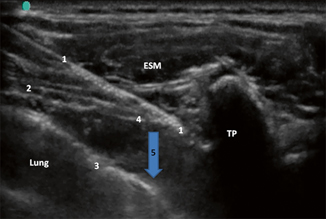
Fig. 23.5
Needle position in paravertebral space: 1 Tuohy needle; 2 intercostal muscles; 3 parietal pleura; 4 internal intercostal membrane; 5 downward displacement of parietal pleura. TP transverse process, ESM erector spinae muscle
Medication
Complications
Pneumothorax, pleural puncture, vascular puncture, tenderness at injection site, unilateral or bilateral Horner syndrome, hypotension, and spinal anesthesia.
Scientific Literature in Children
Boretsky et al. found that a lateral in-plane technique is the most reliable technique for continuous needle visualization in a series of infants and children as young as 6 months of age and as small as 6 kg [7].
Important Points
If the rib is seen, the probe is slid cephalad a few millimeter until the pleura and TP are visualized with no overshadowing rib. The superior costotransverse ligament should not be visible on the ultrasound image, since it spans between the TP and the rib. If the tip of the needle is placed below the IICM (the lateral continuation of the superior costotransverse ligament) and an anterior movement of the pleura is visualized during injection of local anesthetic the block can technically be considered correctly performed.
TAP Blocks
Introduction
The TAP blocks are increasingly being used to provide analgesia after pediatric surgeries involving the abdominal wall [21]. TAP blocks reduce opioids consumption, improve pain scores compared with traditional pain strategies, and are alternatives to neuroaxial analgesia [22].These blocks require injection of local anesthetic between the internal oblique and transversus abdominis muscles. Evidence suggests that midaxillary and subcostal injections result in a predominantly anterior spread of local anesthetic and the sensory blockade produced is relatively patchy [23]. Therefore, TAP blocks should be performed as posterior as possible [24].
Anatomy
The innervation of the abdominal wall is from the anterior divisions of the T6-L1. The nerves run between the internal oblique and transversus abdominis muscle into the transversus abdominis plane. The points of entry of the anterior branches into the TAP and the distance that these nerves travel in this plane are variable [23]. The nerves have a perforator branch that innervates the anterolateral portion of the abdominal wall. A posterior injection may block T6-L1 nerves in close proximity to one another before they bifurcate. This is clinically significant because the blocks should be performed as posterior as possible to include these nerves, improve the spread of local anesthetic, cover several dermatomes, and improve the block success.
Indication
Using the classic midaxillary procedure, these blocks work well for procedures below the T10 dermatome (urology and gynecologic procedures, varicocelectomy, hydrocelectomy, ureteral reimplantation). Lateral, posterior, or quadratus lumborum TAP block techniques are recommended for surgeries at the T10 dermatome (colectomy, colostomy, ileostomy creation and take down, inguinal hernia repair, laparoscopic procedures such as appendectomy). More studies should be done to assess whether these blocks can cover as high as the T8 dermatome. Alternative techniques are recommended for upper abdominal surgeries such as cholecystectomies, Nissen fundoplications, and G tube placements (subcostal TAP).
Ultrasound Techniques
In-plane.
Ultrasound Probe
High-frequency linear probes (15/13−6 MHz), 5 cm footprint. A small footprint (2.5 cm) is recommended for patients less than 20−30 kg.
Patient Position
Supine.
Step-by-Step Technique
Place the probe in a transverse plane with the medial end of probe over the umbilicus and obtain an image of the rectus abdominis muscle. Slide the probe laterally across the abdominal wall with the goal to have the probe in the anterior axillary line, between the costal margin and iliac crest, until three muscle layers are present (Fig. 23.6). The most superficial one is the external oblique followed by the internal oblique and the transversus abdominis muscle. Continue to move the probe laterally until the transversus abdominis muscle terminates on the screen (Fig. 23.7). The site of injection is between the internal oblique and transversus abdominis muscles, close to the termination of transversus abdominis muscle. The needle is advanced from anterior to posterior direction through adipose tissue, external, and internal oblique muscles (Fig. 23.8). Correct needle position within the TAP is confirmed by real-time ultrasound visualization of saline hydrodissecting the plane between the two muscle layers (Fig. 23.9). Once proper needle location is confirmed local anesthetic is injected.

Fig. 23.6
Ultrasound probe position for transversus abdominis plane block
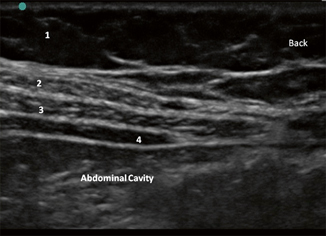
Fig. 23.7
Ultrasound anatomy of transversus abdominis plane block: 1 adipose tissue; 2 external oblique muscle; 3 internal oblique muscle; 4 transversus abdominis muscle

Fig. 23.8
Medial to lateral needle orientation for transverses abdominis and quadratus lumborum plane blocks
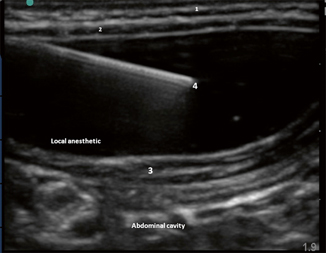
Fig. 23.9
Local anesthetic hydrodissecting transversus abdominis plane in a neonate: 1 external oblique muscle; 2 internal oblique muscle; 3 transversus abdominis muscle; 4 needle
Alternate Techniques
To obtain analgesia above the umbilicus, a subcostal TAP block is necessary. The probe should be placed parallel to the costal margin and move medially just inferior to the costal margin (Fig. 23.10). Transversus abdominis muscle can be seen extending behind the rectus abdominis muscle (Fig. 23.11). The needle should be inserted in a medial to lateral direction beneath the costal margin (Fig. 23.12) and the medication should be seen hydrodissecting the plane above the transversus abdominis muscle.

Fig. 23.10
Ultrasound probe position for subcostal transversus abdominis plane block
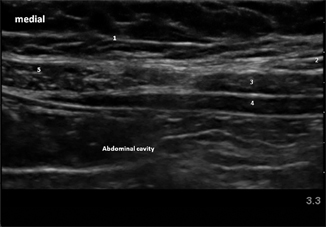
Fig. 23.11
Ultrasound anatomy of subcostal transversus abdominis plane blocks: 1 adipose tissue; 2 external oblique muscle; 3 internal oblique muscle; 4 transversus abdominis muscle; 5 rectus muscle
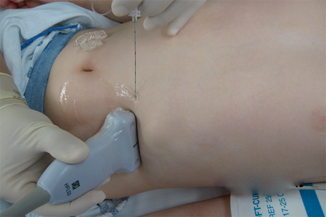
Fig. 23.12
Medial to lateral needle orientation for subcostal transversus abdominis plane block
In order to reach as many dermatomes as possible, a quadratus lumborum block can be performed. A lateral position with the operative side up (Fig. 23.13) or “sloppy lateral (positioned supine with the body rotated towards the opposite side to have access to the patient’s back at the block site) (Fig. 23.1). The probe should be placed between the costal margin and iliac crest and moved as posterior as possible until quadratus lumborum muscle is identified (Fig. 23.14). The needle is inserted in a medial to lateral direction beneath the anterior border of quadratus lumborum muscle (Fig. 23.15). This block may be very challenging because the muscle is not always easy to identify and is difficult to keep the needle in the correct tissue plane as the body curves laterally.

Fig. 23.13
Patient position for posterior and quadratus lumborum transversus abdominis plane block
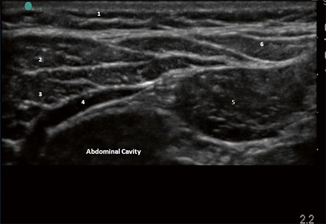
Fig. 23.14
Ultrasound anatomy of quadratus lumborum block: 1 adipose tissue; 2 external oblique muscle; 3 internal oblique muscle; 4 transversus abdominis muscle; 5 quadratus lumborum muscle; 6 latissimus dorsi muscle
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree