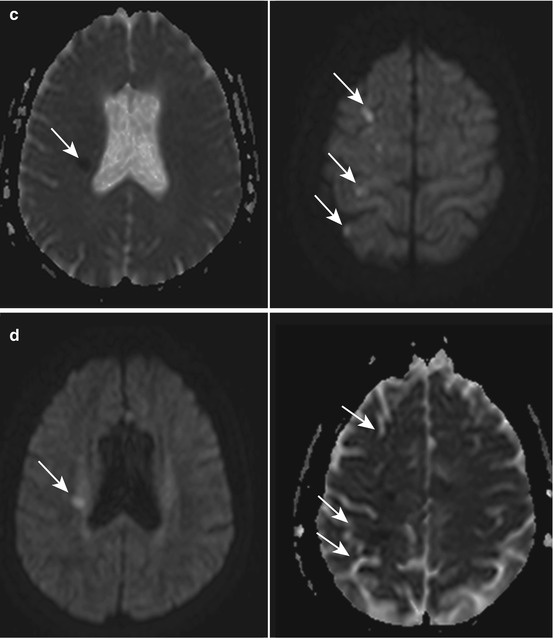
Fig. 1
Watershed ischemia post-balloon remodeling of right MCA aneurysm. (a) Pre- and post-angiograms using remodeling technique. MRI study post-embolization of right MCA aneurysm using remodeling technique. (b) FLAIR; (b) DWI; (c) ADC; (d) Maps show area of deep (left) and superficial (right) MCA watershed ischemia – white arrows show infarction
Additional adjuvant uses of microballoons include
1.
Rescue treatment of prolapsed coils
2.
Treating local thrombus formation
3.
Concomitant angioplasty
4.
Managing intra-procedural ruptures, whether at the time of microcatheter/coil placement or during intubation
Balloon Configuration
Prior to incorporating microballoons within the repertoire of endovascular techniques, one must have an understanding of the basic subtypes of microballoons and their advantages and disadvantages.
Until recently, balloons had two basic geometric shapes (with some minor variation in size to extend the range of aneurysms that can be managed):
Sausage configuration.
Most widely utilized balloon: sausage configuration, oblong shaped.
One such balloon of this type is the HyperGlide™, ev3 (Covidien).
3–6 mm diameter size and lengths from 10–30 mm.
Most commonly used: the 4 × 10–15 mm length.
Rugby or football configuration (when unconstrained).
Typically more compliant than sausage configuration
One example: HyperForm™, eV3 (Covidien, Plymouth, MN, USA)
Available in two sizes: 4 × 7 mm and 7 × 7 mm
Hyperglide-Type Balloon
Typically less compliant, which tends to determine its use for selective catheterization of branches arising at or within the proximal sac, in order to protect.
Generally more predictable during placement and sequential inflation.
During inflation, usually just prior to vessel occlusion, this balloon type has a tendency to move forward. With practice this can be anticipated for and compensated for by a small pull of the balloon just prior to vessel occlusion.
The converse is equally true: the balloon tends to jockey proximally upon deflation.
For the most part, this motion is manageable and of little impact upon the subjacent microcatheter.
Can be extreme in some patients.
Extra care needs to be taken particularly with very small aneurysms where this movement can potentially propel the microcatheter through the aneurysm sac.
Microballoon Preparation (Fig. 2)
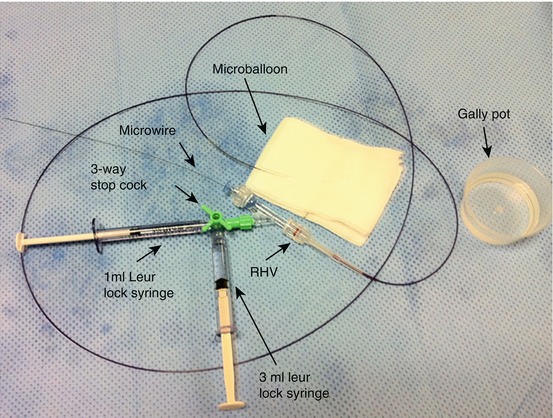
Fig. 2
Pictorial representation of microballoon configuration
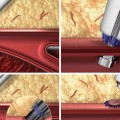
Preparation of the microballoon is of utmost importance, with avoidance of introducing microbubbles within the system a prerequisite.
Preparation is best undertaken within a designated area.
Using a separate trolley makes for a natural “zone” to work within and by virtue creates “safe zone” to avoid contamination of the contrast-saline mixture.
There are several key stages:
Stage 1
Contrast-Saline Mixture
A small gally pot is used to make the desired mixture by first placing 20 ml of saline, followed by 20 ml of 300 omnipaque contrast.
The gally pot could be labeled for additional safety.
The importance of identifying the correct contrast-saline mixture cannot be overemphasized, to avoid inflating a balloon with clear saline and the inherent risk of overinflation and vessel rupture.
Using neat contrast makes deflation of the balloon protracted, potentially necessitating microwire withdrawal to achieve deflation of the balloon.
May potentially contaminate the microballoon with blood, making subsequent inflation difficult, reduce visibility, and make subsequent deflation impossible, even once the microwire has been completely withdrawn.
Stage 2
Preparing the Microballoon
A 1 ml Luer-Lok syringe is filled with the contrast-saline mixture and attached to a 3-way stopcock, which in turn is attached to a RHV (rotating hemostatic value), without introducing any bubbles. This then is attached to the microballoon, which is subsequently flushed. This ensures the microballoon “system” is flushed with the desired contrast-saline mixture and free of microbubbles.
A 3 ml Luer-Lok syringe is attached, again flushed with the contrast-saline mixture, to the vacant hub of the 3-way tap.