Renal Cell Carcinoma
Todd M. Blodgett, MD
Alex Ryan, MD
Hesham Amr, MD
Key Facts
Terminology
Renal cell carcinoma (RCC), clear cell carcinoma, hypernephroma, renal cancer
Imaging Findings
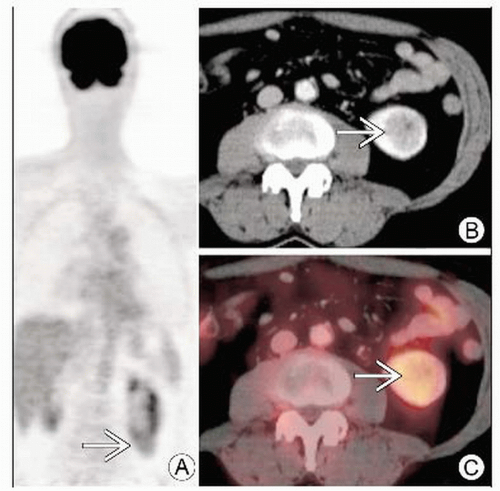
Iso- or hypermetabolic renal mass ± lymphadenopathy, metastases on FDG PET
Presents most commonly as incidental solid tumor on imaging
Enhancing solitary mass on CT highly suspicious for RCC
Hypervascular mass with enhancement (HU increase by > 20) compared to noncontrast
Enhancement often heterogeneous, particularly larger lesions
FDG PET and RCC
FDG uptake by RCC, metastases variable
Sensitivity 60%, specificity ˜ 100% for evaluating primary RCC
80-100% specific for bony metastases
Top Differential Diagnoses
Angiomyolipoma (AML)
Renal Oncocytoma
Hemorrhagic Renal Cyst
Transitional Cell Carcinoma (TCC)
Rare Parenchymal TCC (Indistinguishable from RCC)
Lymphoma
Renal Infection or Abscess
Metastatic Disease
Diagnostic Checklist
FDG PET for staging, evaluation of bony metastases
RCC has variable uptake on FDG PET
TERMINOLOGY
Abbreviations and Synonyms
Renal cell carcinoma (RCC), clear cell carcinoma, hypernephroma, renal cancer
Definitions
Carcinoma of renal tubular epithelium
IMAGING FINDINGS
General Features
Best diagnostic clue
Iso- or hypermetabolic renal mass ± lymphadenopathy, metastases on FDG PET
Presents most commonly as incidental solid tumor on imaging
Enhancing solitary mass on CT highly suspicious for RCC
Necrosis, hemorrhage, septae more likely in large masses
Location
Usually renal cortex
Often exophytic
Rarely bilateral (2%) or multicentric (more common in von Hippel-Lindau)
Size: Variable depending on time of diagnosis
Morphology
10% calcified, often irregular
2-5% cystic
Imaging Recommendations
Best imaging tool
Combination of CT, ultrasound
CECT often shows enhancing lesion; hyperdense benign cysts will not enhance
US indicated in patients with nonenhancing hyperdense renal lesions to differentiate cyst from mass
If contraindication to contrast, MR superior to CT
FDG PET and PET/CT not currently covered by Medicare, but may be helpful for staging and restaging
Protocol advice
For CT: Noncontrast and CECT, thin sections (2.5-5.0 mm), during both corticomedullary and nephrographic phases
For PET CT: If only single phase obtained, use later nephrographic phase of contrast enhancement
Corticomedullary phase (25-70 seconds post-injection)
Better visualization of renal vessels; evaluate for renal vein/IVC thrombosis or tumor extension
Limited detection of small renal lesions
Centrally located tumors commonly mistaken for normal hypoattenuating medulla
Nephrographic phase (80-180 seconds post-injection)
Best imaging of renal medulla masses
CT Findings
NECT
Solid-tissue-density mass, which distorts normal kidney contour and typically is in the 30-50 HU range
Can be hyperdense, isodense, or hypodense to surrounding normal kidney
Heterogeneous mass (hemorrhage and necrosis); high (acute hemorrhage) or low attenuation (chronic)
± Calcifications (10% of cases); amorphous internal (most common), curvilinear (peripheral or central), dense or diffuse calcification
High density rim may separate mass from adjacent renal tissue (pseudocapsule)
Rarely contains small areas of fat (-50 to -150 HU)
Combination of fat and calcification suggests RCC, not renal angiomyolipoma
Cystic RCC
Uni- or multilocular cystic mass with a thick calcification of septa or tumor capsule
Septa may enhance on CECT
CECT
Hypervascular mass with enhancement (HU increase by > 20) compared to noncontrast
Enhancement often heterogeneous, particularly larger lesions
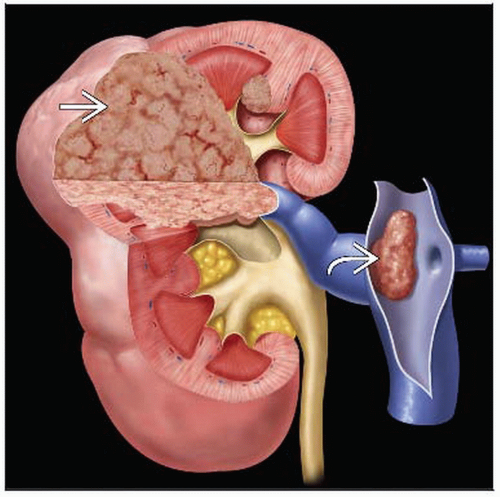
Tumor extension or thrombus in renal vein (23%), inferior vena cava (7%)
Local extension common
Nodal spread typically to para-aortic or aortocaval lymph nodes
Most common metastatic locations include lung, liver, bone, adrenal, and opposite kidney
Usually solid, and decreased attenuation suggestive of necrosis often present
Sometimes presents as predominantly cystic mass with thick septa and wall nodularity
Nephrographic phase is most sensitive for tumor detection, especially for masses smaller than 3 cm
Corticomedullary phase required for tumor extension into renal veins
Evaluation for hypervascular metastases
Helical CT improves diagnosis and eliminates respiratory misregistration
Nuclear Medicine Findings
FDG PET and PET/CT for RCC
Iso- or hypermetabolic renal mass ± lymphadenopathy, metastases
FDG uptake by primary RCC and metastases is somewhat variable; therefore, PET and PET/CT are more helpful when positive
Negative study may represent either a non-FDG-avid RCC or truly negative disease
Sensitivity 60%, specificity ˜ 100% for evaluating primary RCC
Excretory FDG in collecting system can mask small RCCs adjacent to collecting system
80-100% specific for bony metastases
DIFFERENTIAL DIAGNOSIS
Angiomyolipoma (AML)
Fat attenuation (-30 to -150 HU) fairly specific for this neoplasm
Low FDG uptake
Reliably distinguished from malignancy by CT characteristics
Renal Oncocytoma
Central scar on CT/MR and spoke-wheel pattern of vessels on angiograms suggest oncocytoma; not entirely specific
Cannot confidently differentiate from RCC by PET
Hemorrhagic Renal Cyst
> Water attenuation on CT (˜ 30-70 HU)
Should not enhance when comparing noncontrast and CE series
Transitional Cell Carcinoma (TCC)
Renal pelvis filling defect, narrowing
Urothelial thickening or involvement
Rare parenchymal TCC indistinguishable from RCC
Lymphoma
Typically more diffusely infiltrative than discrete mass
Renal Infection or Abscess
Focal nephritis can appear mass-like
Short term follow-up helpful
Clinical history and urine analysis often helpful
Metastatic Disease
History essential
Common primary cancers include lung, breast, colon, melanoma, pancreatic
Typically only hypervascular metastases mistaken for RCC
PATHOLOGY
General Features
General path comments
Staging
Stage I: Solid mass ≤ 7 cm, confined to kidney
Stage II: > 7 cm but still organ confined; spread to perinephric fat
Stage III: Invasion of renal vein or vena cava, involvement of ipsilateral adrenal gland &/or perinephric fat, or spread to one local lymph node
Stage IV: Invasion of adjacent organs, more than one local node, or distant metastases
Genetics: Associated with von Hippel-Lindau syndrome (autosomal dominant)
Etiology
Arise from tubular epithelium
Bilateral lesions associated with von Hippel-Lindau syndrome, tuberous sclerosis, chronic dialysis
Other risk factors: Smoking, chemical exposure (diethylstilbestrol and fluoroacetamide)
Epidemiology
Approximately 2% of adult malignancies (30,000/year in USA)
Undiagnosed small RCCs found at autopsy even more frequently
Gross Pathologic & Surgical Features
Solid to cystic components with necrosis, hemorrhage, and rarely fat
Microscopic Features
70% clear cell, 13% papillary, 7% granular, 10% other
CLINICAL ISSUES
Presentation
Most common signs/symptoms
Usually a combination of hematuria (50%), flank pain (40%), &/or flank mass (35%)
Nearly half of RCCs discovered incidentally
Other signs/symptoms
Fever, nausea, weight loss
Rarely, humoral factors such as erythropoietin, renin, parathyroid hormone, or prolactin may cause symptoms
Demographics
Age: Generally 50-70 years, with wide distribution
Gender: M > F, 2:1
Natural History & Prognosis