Given the incidence of small renal masses, from benign cysts to malignancy, most radiologists encounter these lesions multiple times during their career. Radiologists have an opportunity to provide critical data that will further refine the understanding of the impact of these masses on patient outcomes. This article summarizes and describes recent updates and understanding of the critical observations and descriptors of renal masses. The templates and glossary of terms presented in this review article facilitate the radiology reporting of such data elements, giving radiologists the opportunity to improve diagnostic accuracy and influence management of small renal masses.
Key points
- •
Incidental renal masses are frequently encountered by radiologists and their management is usually guided by imaging features.
- •
Reporting of renal masses is improved by the use of structured templates with specific terminology and management guidelines.
- •
The Society of Abdominal Radiology’s Disease Focused Panel on Renal Cell Carcinoma (DFPRCC) published the results of a survey of academic radiologists and urologists to determine the most desired contents of a structured radiology report describing a renal mass.
- •
A proposed update to the widely used Bosniak classification system aims to improve its specificity through changes, such as providing clearer definitions of descriptors and incorporating MR imaging findings.
- •
We present sample templates for reporting of renal masses with a glossary of terms by building on templates created by the DFPRCC and incorporating the 2019 Bosniak classification update.
Introduction
Radiologists have increasingly adopted structured radiology report templates and constrained vocabularies for describing imaging findings. There are many arguments in favor of moving in this direction, including a decrease in error rate, improved quality, comprehensiveness, adherence to guidelines, consistency, and revenue capture. The body of literature demonstrating a preference for structured radiology reports by referring providers and radiologists is growing. , , , Structured report templates using common data elements facilitate cross-institution collaborations and the creation of radiology registries to support translational and clinical research. , Such registries could also be used to establish national quality benchmarks and to drive the creation and adoption of artificial intelligence algorithms.
Generally, constrained vocabularies are modality-specific and intended to reduce variability of terminology in reports, improve communication between radiologists and recipients of radiology report data, and create a framework for improving understanding of the diseases imaged. Many constrained vocabularies and scoring systems have been cataloged and developed through the American College of Radiology Reporting and Data Systems initiative. , Although no specific vocabulary has been developed for renal masses, the Bosniak system, created more than 30 years ago, with a suggested update in 2019, is commonly used for cystic renal mass classification. , The advent of minimally invasive techniques for management of solid renal masses, such as partial nephrectomy, has driven the surgical literature to devise scoring rubrics for surgical risk stratification. Finally, because of the frequency of detection of renal masses, algorithms for management have been developed.
This article summarizes and describes recent updates and understanding of the critical observations and descriptors of renal masses. A series of template modules are included and a glossary of terms. This article reviews the consensus work out of the Society of Abdominal Radiology Disease Focused Panel on Renal Cell Carcinoma (DFPRCC) ( https://www.abdominalradiology.org/page/DFPRCC ).
Epidemiology of renal masses
More than 330,000 new cases of kidney cancer are diagnosed a year, making it the 13th most common cancer worldwide. The incidence of renal cell carcinoma (RCC) has been increasing steadily since the 1970s. Although changes in lifestyle and exposure to risk factors have been implicated in the increased incidence of RCC, the rise in use of diagnostic imaging is also a factor in detection. Most renal masses are benign cysts, with the prevalence of cysts also increasing with age. In fact, renal cysts are identified in 20% to 45% of a general imaging population, suggesting they may be in the realm of a normal finding. , , However, of those incidental renal lesions, a proportion are RCCs and patient prognosis seems to improve if the renal mass was detected incidentally. , This apparent improvement in outcome may be the consequence of early treatment or increased detection of benign neoplasms or indolent cancers. Because of the role imaging plays in the detection of these masses and the associated epidemiologic impact, it behooves the radiology community to leverage the knowledge and understanding of the features that differentiate malignant and benign renal masses, to mitigate risks associated with potential overtreatment if the disease is overdiagnosed.
Increasing precision in the description of renal masses
Addressing Stakeholder Concerns
Through the leadership and initiative of the DFPRCC, the knowledge and understanding of the features that radiologists should be describing when characterizing newly discovered renal masses is improving. This improvement is manifest through the radiology report that is generated when a radiologist encounters the incidental renal mass. In 2019, the DFPRCC published the results of their survey of radiologists and urologists from nine tertiary care academic institutions that was designed to determine the most desired contents of a structured report of a computed tomography (CT) or MR imaging performed to evaluate a renal mass.
Davenport and colleagues determined that consensus was reached if 70% of respondents agreed that a particular reporting element was essential or preferred. This threshold was chosen because of the range of opinions and local practice patterns that were elicited in the survey. Features that met this 70% threshold included whether a mass is cystic or solid, including a Bosniak classification of cystic masses with the features used to assign said classification; mass size in comparison with prior imaging, with a desire for mass size to be in the impression if it is a mass that will require surveillance or intervention, such as solid, Bosniak IIF, Bosniak III, and Bosniak IV masses; the presence of fat or enhancement and how much of the mass enhances, whether or not there is necrosis in a solid mass; the features of the margin, whether circumscribed or infiltrative; and finally radiologic staging for solid masses and Bosniak IV cystic masses. Additionally, there were several specific features that assist in surgical planning for patients who might benefit from a nephron-sparing therapy that met the 70% threshold for consensus. These include the axial location of the mass, capsular location of the mass, distance of the mass to the sinus fat, and distance of the mass to the collecting system.
Not surprisingly, there were some differences in opinion between urologists and radiologists as to essential features. The urologists were more likely to want enhancement on CT to be reported quantitatively (eg, Hounsfield units of the precontrast and postcontrast and/or calculated difference) rather than qualitatively (eg, enhancement, no enhancement). Other than a recommendation of the best type and interval of follow-up imaging, most urologists did not want management recommendations included in the report.
Updating the Bosniak Classification
Given the importance of the Bosniak classification in the description of cystic renal masses and known inconsistencies in the application of the original features to classification, another recent development is a proposed update of the Bosniak classification of cystic renal masses. The Bosniak classification is widely used in clinical practice to stratify the risk of malignancy in cystic renal masses based on imaging features on contrast-enhanced CT and to guide management. The Bosniak classification, version 2019, proposes several updates to the original classification system to improve specificity and reduce the number of benign masses that undergo unnecessary treatment. The updated version accomplishes this by providing specific definitions for previously vague imaging features, incorporating MR imaging findings into the classification, expanding the number of masses that can be included in the classification, and increasing the proportion of masses that can be assigned to lower Bosniak classes. In addition, specific management language is included, also with the goals of increasing consistency.
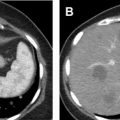
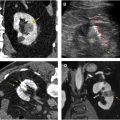
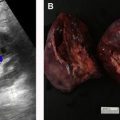
In the updated Bosniak classification, a cystic mass is defined as a mass of which less than 25% is composed of enhancing tissue. A summary of the Bosniak classes follows. The imaging features that differentiate classes are illustrated in Fig. 1 .

Bosniak I
Bosniak I cysts are simple cysts without septa, solid component, or calcification. A Bosniak I cyst must be well-defined with a smooth, thin wall that may enhance. A “thin” wall is defined as being less than or equal to 2 mm.
The updated version defines enhancement as either clearly visible enhancement or nonvisible enhancement based on established quantitative criteria, which includes increase of 20 HU or more on contrast-enhanced CT when compared with noncontrast study or an increase in signal intensity of 15% or more on contrast-enhanced MR imaging compared with noncontrast MR imaging.
Bosniak I cysts are benign cysts and do not require further work-up or follow-up. When encountered these can be described as “Bosniak I: benign simple cyst requiring no follow-up.”
Bosniak II
Bosniak II category includes
- 1.
“Minimally complicated” cysts, which may have few thin and smooth septa with or without any type of calcification. “Few” septa are defined as between one and three, and “thin” is defined as less than or equal to 2 mm.
- 2.
“Benign hyperattenuating” cysts that are homogeneous and 70 HU or greater on noncontrast CT, or 20 HU or greater and do not enhance on renal mass protocol CT.
The updated Bosniak classification, version 2019, also includes in the Bosniak II category those renal masses that are incompletely characterized but have a high likelihood of being benign fluid-filled lesions. These include homogeneous masses that are
- 1.
Between −9 and 20 HU on noncontrast CT
- 2.
Between 21 and 30 HU on portal venous phase CT
- 3.
Hypoattenuating masses on CT that are too small to characterize
- 4.
Markedly T2 hyperintense masses with signal intensity that is similar to cerebrospinal fluid on noncontrast T2-weighted MR imaging
- 5.
Markedly T1 hyperintense masses, which are defined as approximately 2.5 times renal parenchymal signal intensity, on noncontrast T1-weighted MR imaging
Bosniak II masses are also considered benign with a less than 1% chance of malignancy and do not require further follow-up. Those that are confirmed to be cysts can be reported as “benign Bosniak II renal cyst requiring no follow-up,” whereas those that are low-attenuating but too small to characterize can be reported as “likely benign Bosniak II renal mass requiring no follow-up.”
Bosniak IIF
Bosniak IIF class includes well-defined cystic masses with more than a few septa. The septa and wall may be thin, or they may be smooth with minimal thickening. The updated Bosniak classification defines “more than a few septa” as greater than four, “thin” as less than or equal to 2 mm, and “minimal thickening” as 3 mm or less. The walls or septa of a Bosniak IIF mass must enhance.
Bosniak IIF also includes cystic masses that are heterogeneously hyperintense on fat-saturated T1-weighted MR imaging without contrast and do not meet the criteria for Bosniak III or IV category. Because this finding is a presentation of papillary RCC, it has been added to Bosniak IIF class in the updated version.
Heterogeneous masses detected on CT that do not enhance are incompletely characterized and are further evaluated with contrast-enhanced MR imaging. If the mass is truly cystic on MR imaging, the Bosniak class may be determined based on its MR imaging features.
Bosniak IIF masses are considered indeterminate and undergo surveillance. The phrase that is recommended by Silverman and colleagues to use in the report is, “Bosniak IIF cystic renal mass. Most Bosniak IIF masses are benign. When malignant, nearly all are indolent. Generally, Bosniak IIF masses are followed by imaging at 6 months and 12 months, then annually for a total of 5 years to assess for morphologic change.”
Bosniak III
Bosniak III class includes cystic masses with thick and irregular enhancing wall or septa. The definition of “thick” is greater than 4 mm. “Irregular” is defined as a focal or diffuse convex protrusion measuring 3 mm or less with obtuse margins with the wall or septa. Bosniak III masses have 50% likelihood of malignancy and are treated. The phrase that is recommended by Silverman and colleagues to use in the report is, “Bosniak III cystic renal mass. Bosniak III masses have an intermediate probability of being malignant. If not already obtained, consider urology consultation.”
Bosniak IV
Bosniak IV category includes cystic masses with enhancing nodules. A “nodule” is defined as a focal or diffuse convex protrusion of any size that has acute margins with the wall or septa, or a convex protrusion that is 4 mm or greater and has obtuse margins with the wall or septa. These masses have 90% likelihood of malignancy and are also treated. The phrase that is recommended by the Silverman and colleagues to use in the report is, “Bosniak IV cystic renal mass. Most Bosniak IV masses are malignant. If not already obtained, consider urology consultation.”
Nephrometry Scoring Systems
According to the American Urologic Association and European Association of Urology guidelines, nephron sparing surgery (NSS), or partial nephrectomy, should be prioritized in the treatment of clinical T1a lesions when technically feasible. , NSS has equivalent oncologic outcomes when compared with radical nephrectomy in localized small tumors, and robust evidence suggests higher overall survival rates, which may be attributable to favorable functional renal outcome.
Tumor size, location, and anatomic factors have decisive influence on the technical feasibility of NSS. Thus, various systems have proposed standard metrics to assess the tumor complexity and predict risk of complications after partial nephrectomy. These systems have been referred to as nephrometry scoring systems. For instance, the R.E.N.A.L. (radius, exophytic/endophytic, nearness to collecting system/sinus, anterior/posterior, and location relative to polar lines) and the Preoperative Aspects and Dimensions Used for an Anatomic (PADUA) classification systems use similar semiquantitative anatomic factors and methodologies. In contrast, centrality index (C-index) and mathematical tumor contact surface area use the geometric relationship between the tumor and kidney. Despite demonstration of external validation and association with perioperative outcomes, the roles of each of these surgical planning scoring systems are still being studied, and clinical adoption is variable. ,
Percutaneous thermal ablation should be considered as an alternate organ-sparing treatment of clinical T1s renal tumors less than 3 cm. Studies have shown that the surgical scoring systems, including R.E.N.A.L. and PADUA, may not have the same predictive efficacy when applied to patients undergoing ablation. This limitation is in part because the percutaneous access approach and ablation technique invoke different periprocedural risks than a surgical approach. For example, a surgeon, whether using open or laparoscopic techniques, is able to physically move adjacent organs, such as bowel or liver, that may be near the tumor, whereas the percutaneous approach relies on hydrodissection to mitigate risk related to adjacency. Thus, interventional radiologists have also advocated for the use of scoring systems to stratify complexity of percutaneous ablation of renal tumors, but with appropriate modifications, including the proximity of the tumor to surrounding anatomic structures.
Management Algorithms
Using the imaging criteria described previously, the incidentally detected renal masses are sorted into several categories for consideration of additional imaging. , , As defined by the American College of Radiology Incidental Findings committee, for the purpose of further imaging after incidental detection on CT, the approach to subsequent imaging depends on whether the mass was initially detected on a contrast-enhanced or nonenhanced CT study, the size of the mass, the attenuation pattern, and absolute attenuation values. If the mass cannot be confidently characterized using subjective criteria on the initial examination, it should be classified as indeterminate.
The management recommendations include no further work-up, MR imaging without and with contrast, or CT without and with contrast either within 6 to 12 months or as soon as can be scheduled. Once the lesion is characterized, the cystic lesions fall into management recommendations based on the updated Bosniak criteria manuscript, and the solid renal masses are managed based on size categories of less than 1.0 cm, 1.0 to 4.0 cm, and greater than or equal to 4.0 cm. , , The sample phrases to include in the summary of any report describing a cystic renal lesion are discussed previously in the summary of the new Bosniak classification recommendations.
Sample Structured Templates
To facilitate the incorporation of the essential features into radiology reporting workflow, including the new Bosniak classification features, we used a sample template rubric ( Box 1 ) to create a series of modules for cystic and solid renal mass reporting ( Boxes 2–4 ) and a management recommendation module ( Box 5 ). A glossary of terms is also included ( Table 1 ). These templates build on those created by the DFPRCC and incorporate the 2019 Bosniak classification update. By building these reports out using Common Data Elements (CDEs) ( https://radelement.org/ ) that encapsulate specific definitions for the terms in the reports, it is possible to have a more streamlined appearing report. Essentially, each pick list presented in the templates is a CDE. Then, the set of CDEs that make up the descriptive module is the rich content that enables the data mining that advances knowledge and understanding about the natural history and risk of these masses, captured when the constrained choices are used for reporting.