Presentation and Presenting Images
( ▶ Fig. 18.1, ▶ Fig. 18.2, ▶ Fig. 18.3, ▶ Fig. 18.4, ▶ Fig. 18.5, ▶ Fig. 18.6, ▶ Fig. 18.7, ▶ Fig. 18.8)
A 40-year-old female with a history of a palpable right retroareolar mass 2 weeks ago that has since resolved. The referring physician’s assessment mentions no palpable abnormalities in either breast. She presents for baseline screening mammography and she requests tomosynthesis.
18.2 Key Images
18.2.1 Breast Tissue Density
There are scattered areas of fibroglandular density.
18.2.2 Imaging Findings
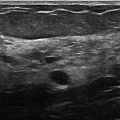
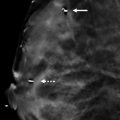
Imaging reveals bilateral retropectoral saline implants ( ▶ Fig. 18.9 and ▶ Fig. 18.10). Saline implants are relatively radiolucent compared to silicone implants. The implants are behind the pectoralis muscle (arrow). The radiopaque smaller circle in the center of the implants represent the valve for implant filling during surgical placement. There are no suspicious masses, architectural distortions, or calcifications in either breast.
18.3 BI-RADS Classification and Action
Category 2: Benign
18.4 Differential Diagnosis
Retropectoral saline implant and normal mammogram: The implant is located posterior to, or behind, the pectoralis muscle. Saline implants are easily penetrated by the X-ray beam. There are no mammographic findings seen that correlate to the resolved clinical issue.
Retropectoral silicone implant: The implant is located posterior to, or behind, the pectoralis muscle. Silicone is dense and not easily penetrated by the X-ray beam. This implant is not dense enough to be silicone.
Prepectoral saline implant: Prepectoral implants are positioned in front of the pectoralis muscle. The implant, in this example, is behind the pectoralis muscle, or retropectoral.
18.5 Essential Facts
Tomosynthesis images may be acquired in every conventional mammographic orientation, that is, craniocaudal (CC), mediolateral oblique (MLO), mediolateral (ML), and lateromedial (LM). Tomosynthesis can also perform spot-compression and implant-displaced views, but not magnification views.
Implants positioned behind the pectoralis muscle have a lower prevalence of capsular contraction than prepectoral implants. It is easier to perform mammograms with retropectoral implants.
In order to limit radiation exposure in patients with breast implants, we acquire tomosynthesis images only in the implant-displaced views.
Although this patient informed the referring physician and technologist that the palpable finding had resolved and the referring physician’s assessment revealed no palpable abnormalities in either breast, the final report reflected the history, physical examination findings, and the imaging findings that no suspicious right retroareolar findings were seen.
18.5.1 Management and Digital Breast Tomosynthesis Principles
Tomosynthesis may be safely performed in patients with saline and silicone implants without significant concern for implant rupture. The exact incidence of implant ruptures is unknown. The risk of rupture is directly associated with the age of the implant and inversely related to the thickness of the implant’s elastomer shell.
The amount of breast compression with tomosynthesis is less than the compression with conventional digital mammography. This is important, as discomfort and pain associated with compression for conventional digital mammography is a concern of patients and prevents some patients from remaining compliant with annual mammography. Breast compression may be of even greater concern for patients with implants, who should be assured that tomosynthesis may be safely performed in patients with breast implants.
18.6 Further Reading
[1] Juanpere S, Perez E, Huc O, Motos N, Pont J, Pedraza S. Imaging of breast implants-a pictorial review. Insights Imaging. 2011; 2(6): 653‐670 PubMed
[2] Saunders RSJr, Samei E, Lo JY, Baker JA. Can compression be reduced for breast tomosynthesis? Monte carlo study on mass and microcalcification conspicuity in tomosynthesis. Radiology. 2009; 251(3): 673‐682 PubMed
[3] Yang N, Muradali D. The augmented breast: a pictorial review of the abnormal and unusual. AJR Am J Roentgenol. 2011; 196(4): W451-W460PubMed

Fig. 18.1 Right craniocaudal (RCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree