and Arumugam Rajesh2
(1)
Department of Radiology, Harvard Medical School Massachusetts General Hospital, Boston, Massachusetts, USA
(2)
Department of Radiology, University Hospitals of Leicester NHS Tr Leicester General Hospital, Leicester, UK
Tumor
Case 5.1
Brief Case Summary:
64 year old female with abdominal pain
Imaging Findings
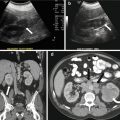
Axial image from a contrast enhanced CT scan of the abdomen and pelvis demonstrates the presence of a heterogeneous, soft tissue mass expanding the inferior venae cava (IVC) (arrow, Fig. 5.1a). The cephalocaudal extent of the lesion is better demonstrated on the coronal reformatted image (Fig. 5.1b).


Fig. 5.1
(a) Axial image from a contrast enhanced CT scan of the abdomen and pelvis demonstrates the presence of a heterogeneous, soft tissue mass expanding the inferior venae cava (IVC) (arrow). (b) Cephalocaudal extent of the lesion is better demonstrated on the coronal reformatted image
Axial images from a three phase (non-contrast, arterial and portal venous) CT scan in another patient demonstrate the presence of an enhancing soft tissue mass expanding the inferior vena cava (Fig. 5.2a–c). The mass contains a punctate calcification, best visualized on the non-contrast image (arrow, Fig. 5.2a). Coronal reformatted image from the same patient demonstrates the cephalocaudal extension of the lesion, with involvement of both the left renal vein (arrow, Fig. 5.2d) and the suprahepatic IVC (double arrow, Fig. 5.2d).
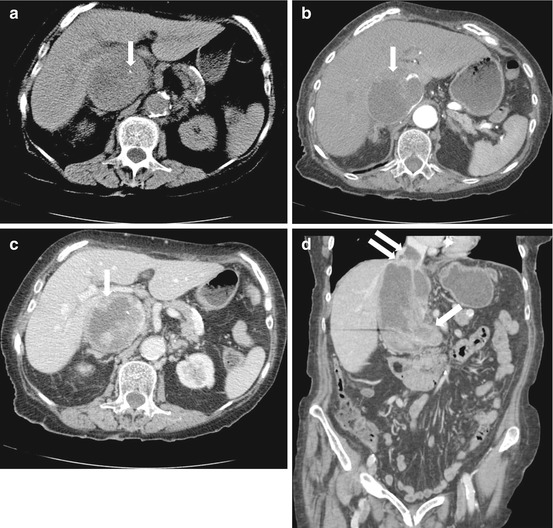
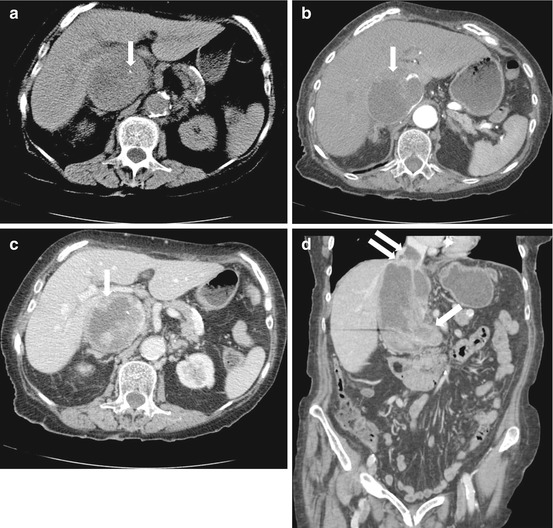
Fig. 5.2
Axial images from a three phase (non-contrast, arterial and portal venous) CT scan in another patient demonstrate the presence of an enhancing soft tissue mass expanding the inferior vena cava (a–c). The mass contains a punctate calcification, best visualized on the non-contrast image (arrow, a). Coronal reformatted image from the same patient demonstrates the cephalocaudal extension of the lesion, with involvement of both the left renal vein (arrow, d) and the suprahepatic IVC (double arrow, d)
Differential Diagnosis
Bland thrombus involving the IVC, Primary leiomyosarcoma of the IVC, Primary retroperitoneal sarcoma extending into the IVC, Exophytic mass arising from an adjacent organ (adrenal glands, kidney).
Diagnosis and Discussion:
Primary leiomyosarcoma of the IVC.
Primary leiomyosarcoma of the IVC is a rare, slow growing neoplasm that arises from the smooth muscle layer of the tunica media. Clinical symptoms may relate to the specific segment of involved IVC where infra-renal IVC involvement may present with sign of venous obstruction, while tumor at or above the level of the renal veins may give rise to renal failure or Budd Chiari syndrome. The imaging appearance is non-specific, manifesting as a heterogeneous mass expanding the IVC with variable area of soft tissue enhancement and necrosis. Calcifications within the lesion are rare.
The tumor may be confined to the IVC lumen or may extend extrinsically to involve adjacent structures. Metastases to the liver, lung, lymph nodes, skeleton and brain usually occur late in the disease process. Aggressive surgical resection is the mainstay of therapy with no established consensus on the role for adjuvant/neoadjuvent therapy. Tumors confined to the level of hepatic veins are least amenable to surgical therapy.
Pitfalls
Benign mimickers of IVC filling defects include bland thrombus and flow related phenomenon. Contiguous extension of a primary retroperitoneal leiomyosarcoma into the IVC may be difficult to distinguish from a primary IVC neoplasm. A heterogeneous mass in the IVC may also result from tumor extension from renal cell carcinoma, hepatocellular carcinoma and adrenocortical carcinoma.
Teaching Points
1.
Unlike bland thrombus, IVC tumor thrombus/neoplasm expand the lumen and show variable degrees of enhancement and necrosis.
2.
Differentiation of a primary IVC leiomyosarcoma from contiguous involvement of the IVC from a retroperitoneal soft tissue mass is challenging. Complete effacement of the IVC at the point of maximal contact with the neoplasm may be suggestive of a primary IVC neoplasm.
3.
Overall prognosis is poor with aggressive surgical resection being the mainstay of treatment. Tumors confined above the level of hepatic veins are least amenable to surgical therapy.
Case 5.2
Brief Case Summary:
76 year old male with abdominal pain.
Imaging Findings
CT scan of the abdomen and pelvis with intravenous and oral contrast demonstrates the presence of a large, complex, predominantly fat containing right sided retroperitoneal mass displacing both the right kidney and loops of bowel anteromedially (Fig. 5.3, arrow). Several septations are noted within the lesion and there are focal areas of higher attenuation (Fig. 5.3, curved arrow).
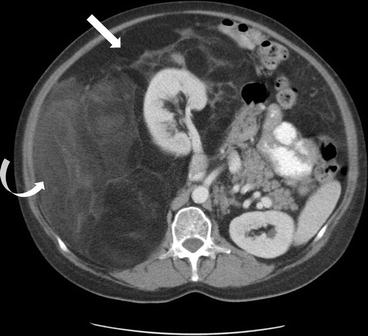
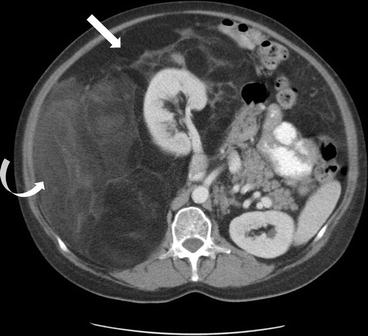
Fig. 5.3
CT scan of the abdomen and pelvis with intravenous and oral contrast demonstrates the presence of a large, complex, predominantly fat containing right sided retroperitoneal mass displacing both the right kidney and loops of bowel anteromedially (arrow). Several septations are noted within the lesion and there are focal areas of higher attenuation (curved arrow)
Differential Diagnosis
Primary retroperitoneal Liposarcoma, Lipoma, Lipoblastoma, Exophytic renal angiomyolipoma (AML), extraadrenal myelolipoma, Hibernoma, Teratoma
Diagnosis and Discussion:
Primary retroperitoneal Liposarcoma, well–differentiated.
Primary retroperitoneal liposarcoma is a rare neoplasm, but constitutes the most common malignant retroperitoneal soft tissue tumor in adults. The neoplasm is most often discovered during the fifth to seventh decades of life, either presenting incidentally, or related to mass effect on adjacent structures. The different histological subtypes have been grouped into three categories. Group 1 includes atypical lipomatous tumor (ALT), well differentiated and dedifferentiated liposarcomas, group 2 is composed of myxoid and round cell subtypes while group 3 consists of pleomorphic liposarcoma. Despite the variable aggressiveness of these subtypes, tumor recurrence is common.
Well differentiated and ALT subtype liposarcomas are the least aggressive neoplasms and do no metastasize. Both are indistinguishable by imaging and typically present as predominantly fat attenuation masses, with variable degrees of septal thickening and nodular soft tissue masses <1 cm. Dedifferentiation within these neoplasm may occur over time, manifesting by new and enlarging areas of focal soft tissue nodules >1 cm in size. Cystic components are rare, and calcifications within the lesion are a poor prognostic factor, usually suggesting the presence of dedifferentiation. Metastases from dedifferentiated liposarcoma may occur in the liver, lung and rarely, the peritoneum.
Myxoid and round cell subtypes are thought to be a continuum of the same histological entity and most often occur within the extremities. Imaging findings are somewhat distinct from group 1 and 2 lesions, manifesting as enhancing multilobulated low attenuation masses with a paucity of intralesional fat. Pleomorphic liposarcoma is an aggressive neoplasm which manifest as heterogeneous soft tissue masses, often with internal hemorrhage and necrosis, with lacy, linear or amorphous foci of fat.
Treatment involves wide surgical excision, with or without adjacent or neoadjuvent chemotherapy dependent on the size and histology of the neoplasm.
Pitfalls
1.
Lipoma and well differentiated liposarcoma may be indistinguishable. However, primary retroperitoneal lipomas are exceedingly rare, and a fat containing primary retroperitoneal lesion should be assumed to be a well-liposarcoma as evaluated as such.
2.
Lipoblastoma is a fat containing mass found in infants and young children
3.
Large exophytic AML or myelolipoma may potentially mimic a liposarcoma, though careful evaluation usually reveals the origin from the kidney and adrenal gland respectively. Extraadrenal myelolipoma most often occurs in the presacral space.
4.
Hibernomas are uncommon lesions composed of brown fat. They rarely occur in the retroperitoneum and demonstrate higher levels of FDG 18 fluorodeoxyglucose uptake on Positron emission tomography (PET) scans.
5.
Retroperitoneal teratomas typically occur in a younger patient demographic, and demonstrate the presence of distinct calcifications (toothlike, well defined) and a fat-fluid level (due to sebum).
Teaching Point
1.
Three groups of liposarcoma have been established. Group 1 is the most common, least aggressive, and is predominantly fat containing. Increase in size of the soft tissue component and the absence of calcifications suggests dedifferentiation with potential risk for metastatic disease.
2.
Group 2 liposarcoma are multilobulated and may appear cystic, however enhancement will be demonstrated after administration of intravenous contrast.
3.
Group 3 lesions are the most aggressive and appear as heterogenous soft tissue masses with a paucity of fat.
Case 5.3
Brief Case Summary:
53 year old male with abdominal pain.
Imaging Findings
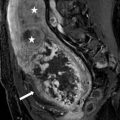
Coronal T1 precontrast (Fig. 5.4) and coronal T1 postcontrast (Fig. 5.5), coronal T2 (Fig. 5.6) and axial T2 (Fig. 5.7) weighted images of the abdomen and pelvis demonstrate the presence of a well-circumscribed multicystic right sided retroperitoneal mass with thickened septations and enhancing soft tissue, displacing the right kidney anteriorly.

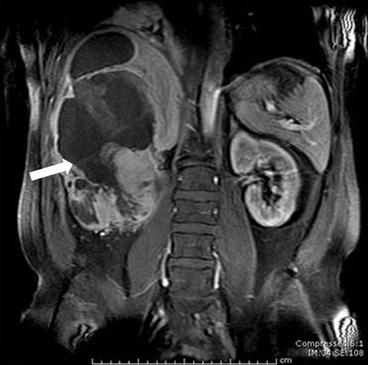

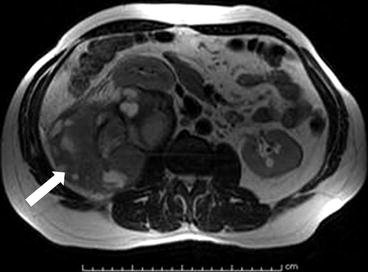

Fig. 5.4
Coronal T1 precontrast weighted image of the abdomen and pelvis demonstrating the presence of a well-circumscribed multicystic right sided retroperitoneal mass (arrow) with thickened septations and soft tissue, displacing the right kidney anteriorly
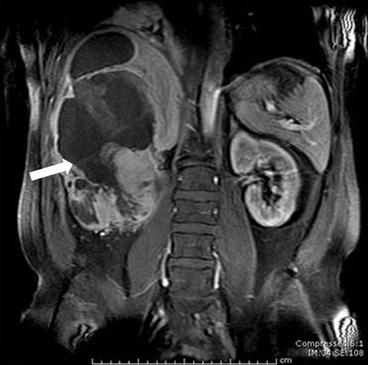
Fig. 5.5
Coronal T1 postcontrast weighted image of the abdomen and pelvis demonstrating the presence of a well-circumscribed multicystic right sided retroperitoneal mass (arrow) with thickened septations and enhancing soft tissue, displacing the right kidney anteriorly

Fig. 5.6
Coronal T2 weighted image of the abdomen and pelvis demonstrating the presence of a well-circumscribed multicystic right sided retroperitoneal mass (arrow) with thickened septations and soft tissue, displacing the right kidney anteriorly
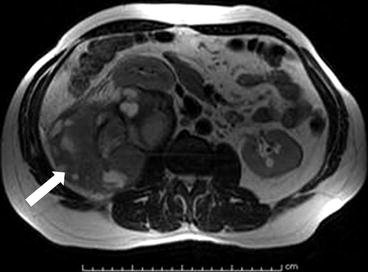
Fig. 5.7
Axial T2 weighted image of the abdomen and pelvis demonstrating the presence of a well-circumscribed multicystic right sided retroperitoneal mass (arrow) with thickened septations and soft tissue, displacing the right kidney anteriorly
Differential Diagnosis
Malignant fibrous histiocytoma, leiomyosarcoma, liposarcoma, malignant peripheral nerve sheath tumor
Diagnosis /Discussion:
Malignant fibrous histiocytoma
Malignant fibrous histiocytoma (MFH) is the third most common primary retroperitoneal sarcoma following liposarcoma and leiomyosarcoma. Patients with retroperitoneal MFH often manifest late with tumors growing greater than 10 cm in diameter on presentation. Imaging finding are non-specific with MFH typically demonstrating heterogeneous soft tissue enhancement with variable area of necrosis, hemorrhage and calcification. Surgical excision is the mainstay of therapy, with limited role of chemotherapy and radiation.
Pitfalls
There are no specific features that allow confident differentiation of MFG from other primary retroperitoneal sarcomas. Leiomyosarcomas calcify less often than MFH and have a tendacy to invade vasculaure, while liposarcomas often contain fat.
Teaching Points
1.
MFH is the third most common retroperitoneal sarcoma, often growing greater than 10 cm on presentation.
2.
It is difficult to differentiate MFH from other primary retroperitoneal sarcomas.
3.
Surgical excision is the mainstay of therapy.
Case 5.4
Brief Case Summary:
27 year old male with abdominal pain after doing situps.
Imaging Findings
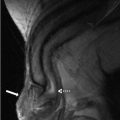
Axial image from a CT scan of the abdomen and pelvis after the administration of intravenous and oral contrast demonstrates the presence of a low attenuating, partially septated midline retroperitoneal mass. The IVC is flattened and compressed posteriorly by the mass (arrow, Fig. 5.8).
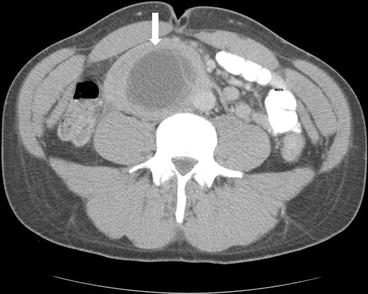
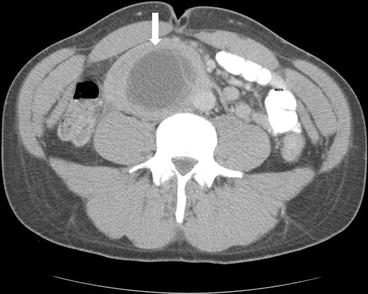
Fig. 5.8
Axial image from a CT scan of the abdomen and pelvis after the administration of intravenous and oral contrast demonstrates the presence of a low attenuating, partially septated midline retroperitoneal mass. The IVC is flattened and compressed posteriorly by the mass (arrow)
Plain radiograph in another patient done for abdominal pain demonstrates the presence of a mass overlying the expected region of the right kidney (Fig. 5.9a). Coronal noncontrast (Fig. 5.9b) and axial contrast enhanced (Fig. 5.9c) images from a CT scan of the abdomen and pelvis performed re demonstrates the lesion and localizes it to the right perinephric space. Left para-aortic lymphadenopathy is also noted (double arrow, Fig. 5.9c).
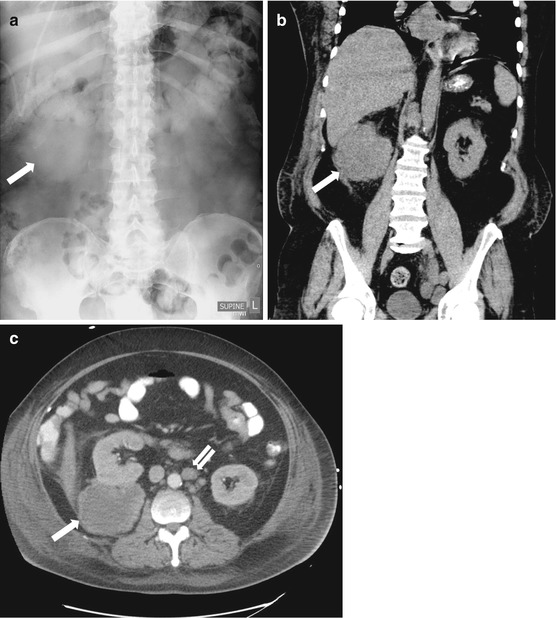
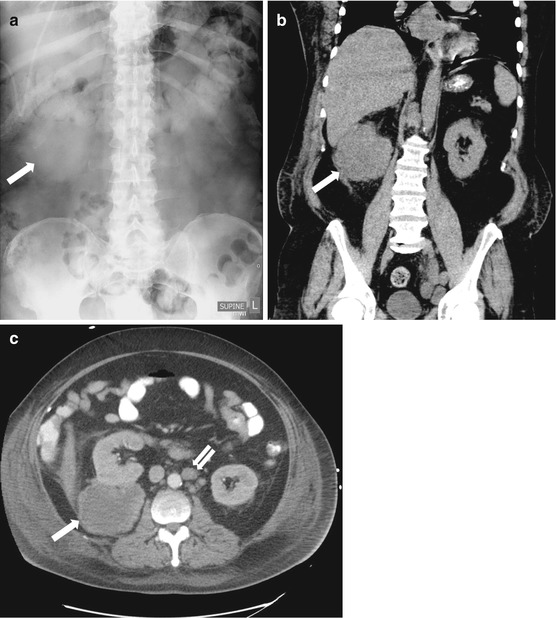
Fig. 5.9
Plain radiograph in another patient done for abdominal pain demonstrates the presence of a mass overlying the expected region of the right kidney (a). Coronal noncontrast (b) and axial contrast enhanced (c) images from a CT scan of the abdomen and pelvis performed re demonstrates the lesion and localizes it to the right perinephric space. Left para-aortic lymphadenopathy is also noted (double arrow, c)
Axial and coronal image from a CT scan of the abdomen and pelvis after the administration of intravenous and oral contrast in another patient demonstrates the presence of confluent retroperitoneal lymphadenopathy with a homogenous soft tissue attenuation (Fig. 5.10a, b). Notice the anterior elevation of the aorta off the upper lumbar spine (arrow, Fig. 5.10a).
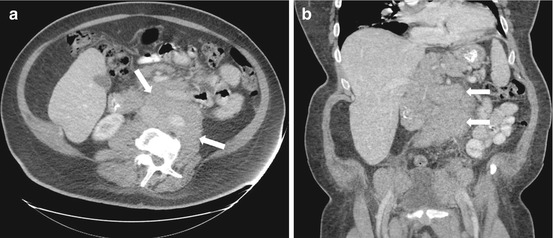
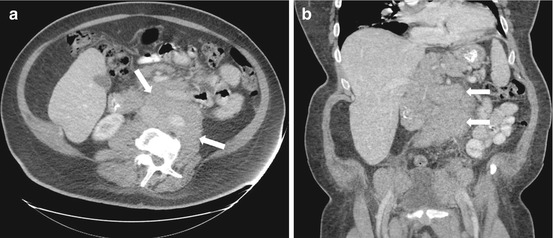
Fig. 5.10
Axial and coronal image from a CT scan of the abdomen and pelvis after the administration of intravenous and oral contrast in another patient demonstrates the presence of confluent retroperitoneal lymphadenopathy with a homogenous soft tissue attenuation (a, b). Notice the anterior elevation of the aorta off the upper lumbar spine (arrows, a)
Differential Diagnosis
Metastatic disease, primary retroperitoneal sarcoma, lymphoma, lymphadenopathy due to infection
Diagnosis and Discussion:
Metastatic disease (germ cell tumor in Fig. 5.8, melanoma in Fig. 5.9, non–Hodgkin lymphoma in Fig. 5.10).
Retroperitoneal lymph nodes are a common pathway for regional spread of intratesticular neoplasms. Metastatic nodes are typically larger than 10 mm in short axis dimension and may manifest as homogenous or heterogeneous density, particularly with nonseminomatous primary testicular neoplasms. Other notable neoplasms to give rise to retroperitoneal metastatic disease include ovarian, prostate, and colorectal cancer, as well as lung and breast. Metastases to the perirenal space are uncommon, but have been described for melanoma, lung, breast and prostate cancer.
Lymphoma represents the most common malignant retroperitoneal tumor. The two broad categories are Hodgkin and non-Hodgkin lymphoma. The latter typically presents at an advanced age with extranodal disease involving the liver, spleen and bowel, and often has mesenteric and retroperitoneal lymphadenopathy at presentation. Hodgkin lymphoma has a bimodal age of distribution of disease and typically presents with isolated disease, often involving the mediastinum. On imaging, retroperitoneal lymphadenopathy related to lymphoma is mildly enhancing, confluent and homogenous, typically insinuating between normal viscera and vessels without compression or obstruction. The aorta may be lifted off the spine resulting in the “floating aorta” sign.
Chemotherapy and radiation are the cornerstones of treatment, and patient are typically followed using positron emission tomography (PET) imaging with viable tumors demonstrating 18 fluorodeoxyglucose (FDG) uptake. Focal areas of calcification and necrosis may be seen after therapy.
Pitfalls
Retroperitoneal soft tissue masses may potentially mimic primary retroperitoneal sarcomas, however the multiplicity, proximity to vessels and the often homogenous attenuation of the lesions typically favors lymphadenopathy
Teaching Point
1.
Retroperitoneal lymphadenopathy in an otherwise healthy young male adult should warrant a search for an underlying testicular neoplasm (ultrasound).
2.
Lymphoma is the most common malignant retroperitoneal tumor. Distinction from primary retroperitoneal sarcoma is critical as the former is treated medically and the latter is treated with surgery.
3.




Confluent, mildly enhancing lymphadenopathy, insinuating between viscera and vessels without compression or obstruction is characteristic of lymphoma. Heterogeneity with calcifications and necrosis may be seen post chemotherapy and radiation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree