RETROPHARYNGEAL AND PREVERTEBRAL SPACE MASSES
KEY POINTS
- Magnetic resonance imaging and computed tomography provide critical and usually definitive data needed in the diagnosis and management of retropharyngeal and prevertebral space masses.
- Prompt and accurate imaging can help to avoid potentially severe neurologic compromise in pathology of the prevertebral space.
- Myelography should be done reluctantly and with the greatest care, if necessary, when there is disease compromising the spinal canal.
- Computed tomography–guided tissue sampling may be useful in the management of these masses.
INTRODUCTION
The retropharyngeal space (RS) and prevertebral space are discussed in this chapter as the sites of origin for mass lesions of the head and neck. The RS is a common secondarily involved site in common inflammatory conditions, such as suppurative retropharyngeal adenitis and the very uncommon true retropharyngeal abscess, and mucosal-origin neoplastic conditions, such as nasopharyngeal squamous cell carcinoma; these are discussed in other chapters. The spectrum of disease seen in the RS but not necessarily originating there is outlined in Table 147.1. The prevertebral space, including both its musculoskeletal and neural elements, is mainly involved by inflammatory and neoplastic pathology of the spine.1
Clinical Presentation
Deep space masses of the suprahyoid neck are often discovered as incidental findings on computed tomography (CT) and magnetic resonance (MR) studies done for other purposes. However, smaller masses in the RS are rarely found this way since the incidence of retropharyngeal masses is much lower than those of the parapharyngeal and masticator spaces. Some larger lesions are discovered because the patient or a health care provider notices a submucosal bulge along the posterior pharyngeal wall at the level of the oropharynx.
Most RS masses are discovered because of symptoms related to the mass with cancers causing pain either due to local effects or skull base invasion. Dysphagia or odynophagia is a common presenting complaint in adults; in infants, swallowing problems may manifest simply as “feeding difficulties.” Otalgia is possible. RS masses may also present as Horner syndrome or neuropathy of cranial nerves IX through XII if the retrostyloid parapharyngeal space (RSPS) is secondarily involved, usually by a malignancy or chordoma.
A prevertebral space–origin mass may present with neck pain that might be mechanical and occipital headache as well as radiculopathy and even myelopathy.
APPLIED ANATOMY
In the suprahyoid neck, the spaces adjacent to the visceral compartment are more numerous and structurally somewhat more complex than they are in the infrahyoid neck. In addition to the RS and prevertebral space, these spaces include the parapharyngeal space (pre- and retrostyloid divisions), prevertebral space, masticator space, parotid gland within its capsule, and submandibular space (Figs. 142.3–142.7, 147.1, and 147.2). The parotid and submandibular glands are discussed in Chapter 175.
The primary skills necessary to interpret CT and MR studies of the deep spaces of the face and supra- and infrahyoid neck are common to these areas and include the following:
- Thorough knowledge of the anatomy.
- Realization that the differential diagnosis:
- Is primarily anatomically driven and largely based on analysis of the point of origin and displacement of normal anatomic structures.
- Requires a rudimentary knowledge of developmental disorders.
- Must take into account that disease may spread transcompartmentally because the process is aggressive and/or extends along existing anatomic structures (e.g., nerve, vessel, muscle bundles, and lymphatics).
- Is primarily anatomically driven and largely based on analysis of the point of origin and displacement of normal anatomic structures.
Spatial Boundaries
The RS is separated from the prevertebral space by the musculofascial sheath associated with the prevertebral muscles at the level the longus colli and longus capitis (Fig. 142.3A, 147.1, and 147.2). The spaces come into contact directly with the posterior skull base at the craniocervical junction. The prevertebral fascia is a strong interface between the two. Both are continuous across the suprahyoid and infrahyoid neck; however, for these two spaces, this separation is still useful because retropharyngeal nodal pathology is relatively common, and those nodes are essentially structures of the suprahyoid neck within the RS.
Structures of Interest
The analysis of a mass of the retropharyngeal and prevertebral spaces depends on a thorough understanding of their relationship to the following structures:
 Superiorly: Posterior skull base in the area of the clivus
Superiorly: Posterior skull base in the area of the clivus
 Inferiorly: Hyoid bone
Inferiorly: Hyoid bone
 Anteriorly: Posterior pharyngeal wall
Anteriorly: Posterior pharyngeal wall
 Posteriorly: Upper cervical spine and pre- and paravertebral muscles and fascia, anterior longitudinal ligament, cervical vertebral bodies and discs, and more superiorly the lower clivus
Posteriorly: Upper cervical spine and pre- and paravertebral muscles and fascia, anterior longitudinal ligament, cervical vertebral bodies and discs, and more superiorly the lower clivus
 Medially: Not applicable
Medially: Not applicable
 Laterally: RSPS, prestyloid parapharyngeal space, and lateral retropharyngeal lymph nodes
Laterally: RSPS, prestyloid parapharyngeal space, and lateral retropharyngeal lymph nodes
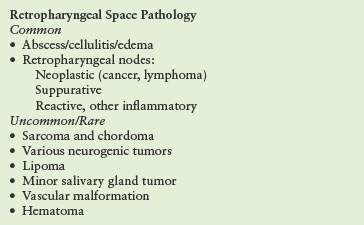
TABLE 147.1 RETROPHARYNGEAL SPACE PATHOLOGY BY FREQUENCY OF OCCURRENCE
IMAGING APPROACH
Computed Tomography and Magnetic Resonance Imaging
The spaces of the suprahyoid neck are studied in essentially the same manner as the nasopharynx is evaluated with magnetic resonance imaging (MRI) and CT. The specifics and relative value of using these studies in this anatomic region are reviewed in Chapter 184. Problem-driven protocols for CT and MRI are presented in Appendixes A and B. In general, MRI is more definitive than CT in the evaluation of deep space masses in the suprahyoid neck, and the images are usually of excellent quality especially above the hard palate. Investigation of inflammatory pathology is usually initiated with contrast-enhanced CT.
Other
Ultrasound has no significant role in the evaluation of pathology in these spaces.
The approach with radionuclide studies depends on the specific aim of the examination. Most current usage is limited to known or suspected cancer evaluation with fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) and bone/gallium scans for inflammatory pathology such as discitis; both are discussed in other chapters. The use of FDG-PET should be extremely limited in retropharyngeal and prevertebral space masses since they will almost always be biopsied for a definitive diagnosis and such imaging will not contribute materially to medical decision making.
Catheter angiography is used rarely occasionally to confirm the diagnosis of a paraganglioma and as a prelude to usually adjunctive endovascular treatment for hypervascular masses.
PATHOPHYSIOLOGY AND PATTERNS OF DISEASE AND DIFFERENTIAL DIAGNOSIS AS SEEN ON MAGNETIC RESONANCE IMAGING AND COMPUTED TOMOGRAPHY
The initial evaluation of a mass involving the retropharyngeal and prevertebral spaces must determine whether they might be only secondarily involved due to a mucosal disease or due to a transspatial process arising deep to the mucosa in the spaces of the suprahyoid neck, cervical spine, or skull base. Transspatial disease may begin in the RS.
Transspatial processes are, regardless of space of origin, masses that arise primarily in the deep spaces of the suprahyoid neck; some of these are listed in Table 143.1. The mechanisms and potential routes of transspatial spread are summarized in Table 143.1. For aggressive pathologies such as cancers or discitis and vertebral osteomyelitis, transspatial spread is a simple morphologic spread pattern to understand. However, the prevertebral fascia is a very tough boundary and is highly restrictive to transspatial spread of any disease, typically confining the disease to the prevertebral and paravertebral space (of origin) and compressing the other surrounding spaces and compartment (Fig. 147.3). It is also is a fairly intuitive pattern to understand in developmental abnormalities that affect the RS. For instance, since venolymphatic malformations grow due to disordered vascular budding, they simply follow vessels as those vessels would normally traverse various compartments or spaces of the suprahyoid neck (Fig. 147.4). In the case of the retropharyngeal and prevertebral spaces, such developmental knowledge helps to predict how notochord remnants relate to those spaces as a source of chordoma (Fig. 147.5).
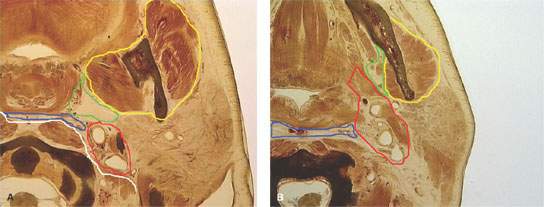
FIGURE 147.1. Anatomic diagrams of the relationships of the deep spaces of the suprahyoid neck and important related anatomic structures. A, B: The retropharyngeal space is outlined in blue and the prevertebral space in white. The white line approximate the attachments of the prevertebral fascia. The retrostyloid parapharyngeal space is outlined in red, the prestyloid parapharyngeal space in green, and the masticator space in yellow for reference.
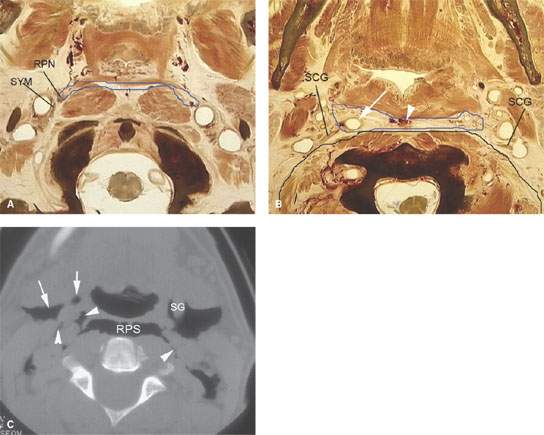
FIGURE 147.2. Anatomic diagrams and a computed tomography (CT) image showing the relationship between the retropharyngeal space (RS) and important adjacent anatomic structures. A: Anatomic diagram showing the RS outlined in blue. The retropharyngeal lymph node (RPN) is within the space. Note that both the lymph node and the sympathetic ganglion and plexus (SYM) relate to the lateral extremity of the RS; this anatomy explains the origin of both nodal and neurogenic processes that might extend into the RS. B: An anatomic section more inferior than that seen in (A). The RS is outlined in blue and the prevertebral and paravertebral spaces in black. The black line shows the approximate position of the prevertebral fascia. Note the relationship of the superior cervical ganglion to the lateral extremity of the RS. Also note that the carotid artery can easily wander into the RS (arrow) and that there is normally a vascular plexus within the RS at this level of the neck. Note the relationship of the superior cervical ganglion to these two spaces and compartments of the neck (SCG). C: CT section of a patient with air spreading within the suprahyoid neck. The RS (RPS) is clearly demarcated as in the prior anatomic diagrams from the prevertebral musculature. Note how the gas collections respect the attachments of the prevertebral fascia spreading within the RS (arrowheads) and parapharyngeal spaces (arrows) but not deep to the prevertebral fascia. (SG, styloglossus muscle.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








