Fig. 5.1
Posteroanterior (PA) chest x-ray showed straightening of the left cardiac border with double contour sign (arrows) indicating left atrial enlargement as well as prominent pulmonary venous blood flow

Fig. 5.2
Lateral chest x-ray showed obliteration of retrosternal space (arrows) consistent with right ventricular enlargement
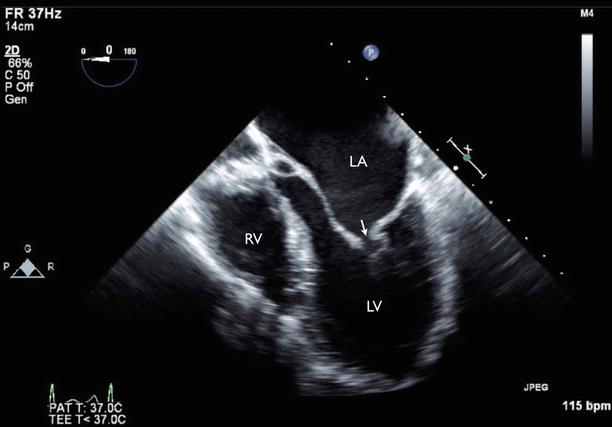
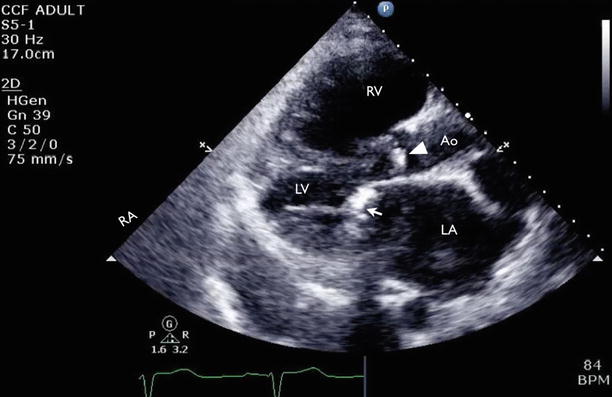
Fig. 5.3
Transesophageal echocardiography (TEE) showed thickened mitral valve with restricted opening (arrow). LA left atrium, LV left ventricle, RV right ventricle
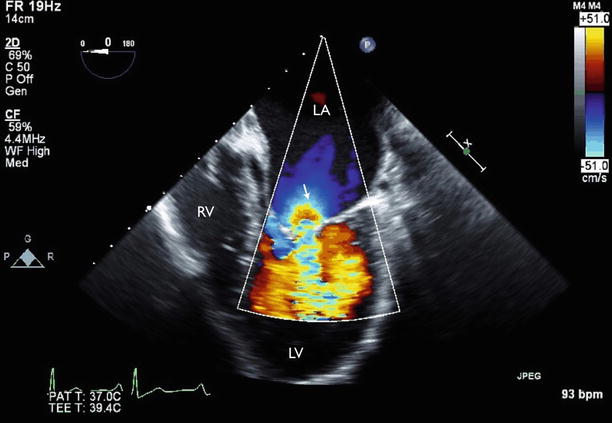
Fig. 5.4
Color flow imaging showed diastolic flow acceleration across the mitral valve during diastole (arrow)
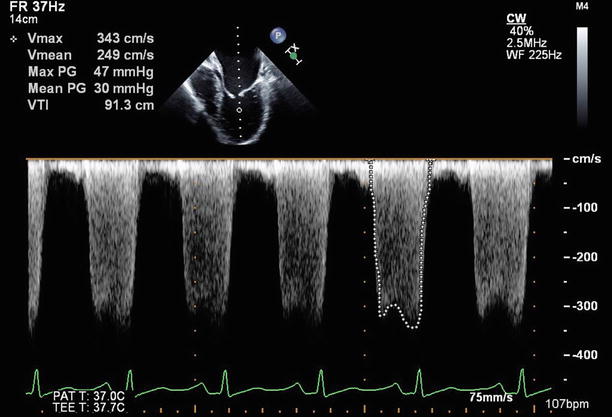
Fig. 5.5
Transmitral gradient across MV showed mean gradient of 30 mmHg, consistent with severe mitral stenosis
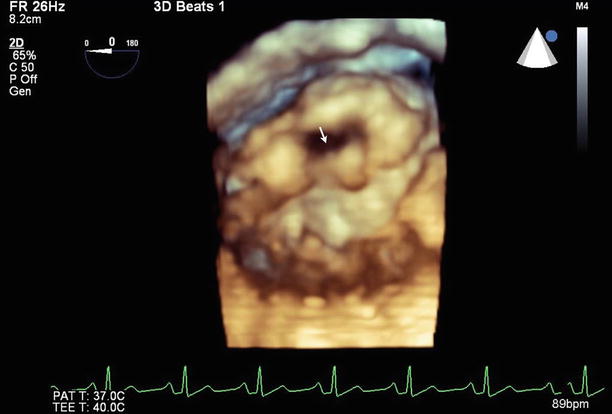
Fig. 5.6
Three-dimensional imaging of the ventricular side of the mitral valve showed limited opening of the valve (arrow)
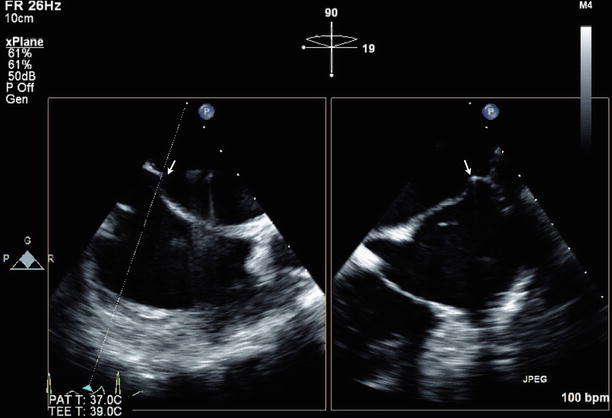
Fig. 5.7
X-plane imaging showing orthogonal imaging of the interatrial septum at the puncture site at the time of the percutaneous balloon mitral commissurotomy (PBMC) (arrows)
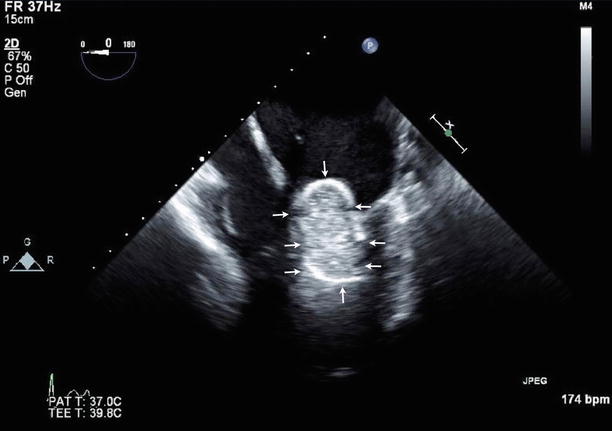
Fig. 5.8
The Inoue balloon (arrows) inflated at the mitral valve
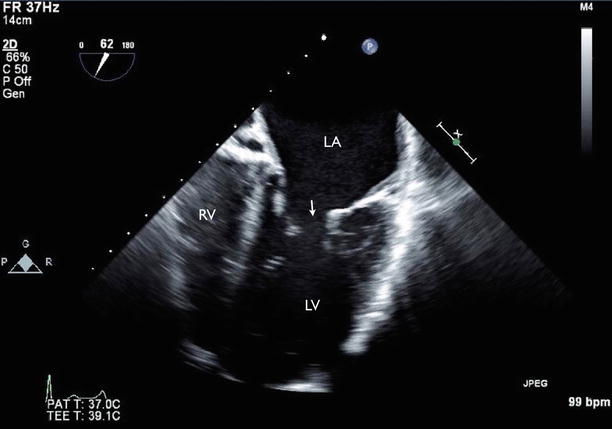
Fig. 5.9
Post PBMC. Improved mitral valve opening (arrow)
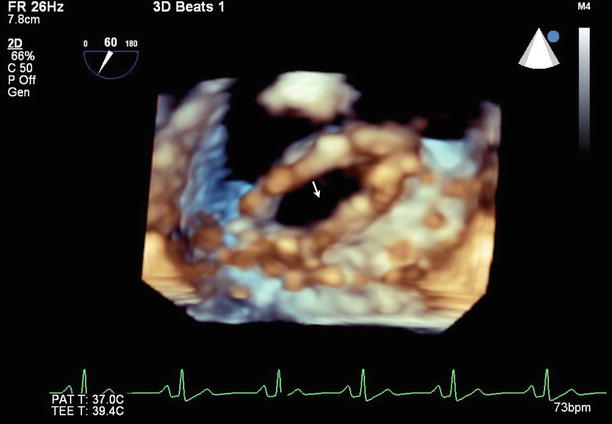
Fig. 5.10
Post PBMC. Mitral valve area (arrow) is increased
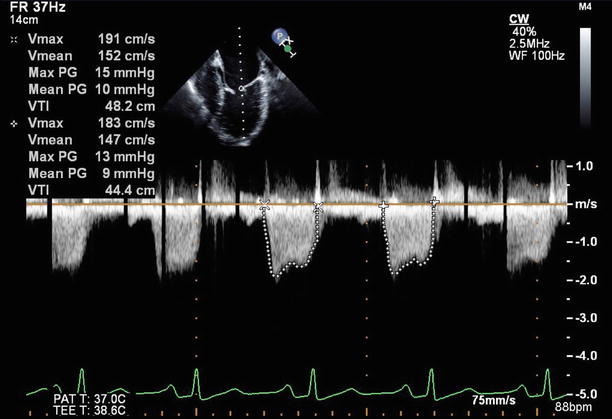
Fig. 5.11
Post PBMC. Decreased transmitral pressure gradient
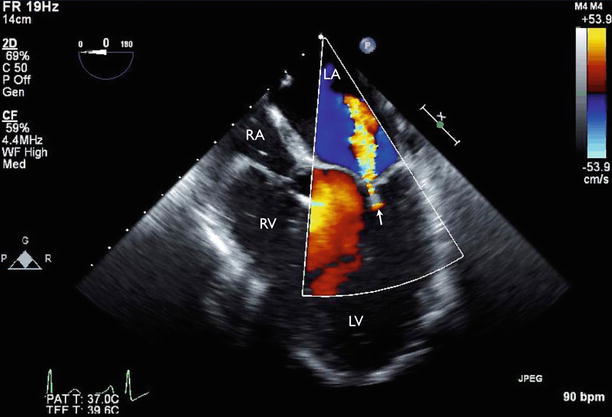
Fig. 5.12
Post PBMC. Mild mitral regurgitation (arrow). RA right atrium
Video 5.1 Transesophageal echocardiography (TEE) showed thickened mitral valve with restricted opening (AVI 2662 kb)
Video 5.2 Color flow imaging showed diastolic flow acceleration across the mitral valve during diastole (AVI 2135 kb)
Video 5.3 Three-dimensional imaging of the ventricular side of the mitral valve showed limited opening of the valve (AVI 2636 kb)
Video 5.4 X-plane imaging showing orthogonal imaging of the interatrial septum at the puncture site at the time of the percutaneous balloon mitral commissurotomy (PBMC) (AVI 2450 kb)
Video 5.5 The Inoue balloon inflated at the mitral valve (AVI 2191 kb)
Video 5.6 Post PBMC. Improved mitral valve opening (AVI 2952 kb)
Video 5.7 Post PBMC. Mitral valve area is increased (AVI 3022 kb)
Video 5.8 Post PBMC. Mild mitral regurgitation (AVI 1995 kb)
5.1.1 Learning Points
Rheumatic mitral stenosis is a slowly progressive disease with a prolonged latent phase between the initial rheumatic illness and the development of valve stenosis. Currently, adequate assessment of mitral stenosis and associated lesions can be obtained in nearly all patients by transthoracic echocardiography (TTE), occasionally supplemented by transesophageal echocardiography (TEE). Several randomized controlled trials have established the safety and efficacy of percutaneous balloon mitral commissurotomy (PBMC), compared with surgical closed or open commissurotomy. The technique is generally performed by advancing one or more balloon catheters across the mitral valve and inflating them, thereby splitting the commissures. For the percutaneous approach to have an optimal outcome, it is essential that the valve morphology be predictive of success, generally being mobile, relatively thin, and free of calcium. This morphology is usually assessed by the Wilkins score, although other risk scores have also shown utility. Clinical factors such as age, NYHA class, and the presence or absence of atrial fibrillation are also predictive of outcome [1].
5.2 Case 2. Severe Rheumatic Mitral stenosis with Severe Pulmonary Hypertension and Severe Secondary Tricuspid Regurgitation
A 66-year-old woman presented with severe rheumatic mitral stenosis and moderate mitral regurgitation with severe pulmonary hypertension and severe secondary tricuspid regurgitation. She reports dyspnea, peripheral edema, and palpitations, which have been worsening over the past 6 months. She presents to her primary care physician with right-sided weakness and an expressive dysphasia and is found to be in atrial fibrillation. She underwent successful mitral valve replacement with tricuspid valve replacement and left atrial appendage ligation (Figs. 5.13, 5.14, 5.15, 5.16, 5.17, 5.18, 5.19, 5.20, 5.21, 5.22, 5.23, and 5.24).