and Michael K. Brooks2
(1)
Department of Radiology, Winthrop-University Hospital, Mineola, NY, USA
(2)
Section of Musculoskeletal Radiology, Department of Radiology, Winthrop-University Hospital, Mineola, NY, USA
Keywords
Biopsy: image-guidedPercutaneousIndicationsRib: anatomyRib core biopsyRib lesionsTechnique: approachesCoaxialLearning Objectives
- 1.
To review the radiologic anatomy that is pertinent toward the safe performance of a rib biopsy
- 2.
To review the indications and contraindications for performing a rib biopsy
- 3.
To learn image-guided percutaneous rib biopsy approaches and techniques
8.1 Introduction
Rib biopsies are performed to identify the etiology of a rib lesion so as to determine if a lesion is malignant or benign. Metastatic disease involves the ribs in approximately 16% of patients with metastatic cancer (De Maesenner et al. 2004). The likelihood that even a solitary rib lesion is a metastasis is high; if the patient does not have a preexisting neoplasm, one series showed an incidence of metastatic foci in 28% of patients, and if the patient has a preexisting extra-skeletal malignancy, another series showed an incidence of metastatic foci in 41% (Baxter et al. 1995; De Maeseneer et al. 2004). The benign spectrum of rib lesions includes healing rib fractures and benign neoplasms such as fibrous dysplasia or hemangioma.
Image-guided percutaneous rib biopsies are infrequently performed procedures. This contributes to the challenging nature of this procedure. The procedure is made more difficult due to patient factors such as inconsistent breathing and the technical challenges related to imaging a curvilinear structure that moves in and out of the imaging plane. Furthermore, the rib is a small structure, in terms of diameter, with a small surface area and with a slick, mobile, hard cortical surface. The rib appears even more diminutive in contrast to its neighboring lung field. Image-guided percutaneous rib biopsies are performed by different radiology subspecialists; hence, an infrequently performed procedure is further diluted among these groups of operators. This creates a relative barrier to developing a consistent approach and technique for addressing this procedure when requested and when clinically indicated. Despite these challenges, given a sound appreciation of these anatomic and technical constraints, a rib biopsy can be performed, safely and efficiently, with a high diagnostic yield.
The curved orientation of the ribs and their proximity to the lungs makes the rib a challenging structure to biopsy.
8.2 Anatomic Considerations
With a few exceptions, 12 ribs are present on each side of the thoracic cage. A minority of individuals will have either 11 or 13 ribs, and when this occurs, care should be taken in analyzing for the presence of transitional vertebrae. The ribs form a rib cage that surrounds the thoracic cavity, including the lungs and pleural cavity. Adjoining ribs are connected by intercostal muscles and fascia. The first seven ribs are directly connected via the costal cartilages with the sternum and are referred to as true ribs (Clemente 1997). The first and second ribs are the most curved, with the second rib being longer than the first. The 8–12th ribs are indirectly connected to the sternum. Ribs number 8, 9, and 10 are continuous with costal cartilages and are referred to as false ribs. Ribs 11 and 12 terminate in the lateral soft tissues of the trunk and are referred to as floating ribs. The ribs are curvilinear tubular structures that have a downward angulation from posterior, near the spine, to anterior. Thus, on conventional axial CT images, the ribs are viewed segmentally and sequentially; the anterior portions of ribs are seen lower down on more caudal images. To study them on an axial data set requires significant scrolling through the images. An alternative technique that can be used to try to visualize a rib in its entirety is to reformat the ribs with obliquely angled images (Figs. 8.1, 8.2, and 8.3). A sagittal or coronal cross section of a rib will show that the rib consists of a semiround cortical surface which surrounds a narrow marrow containing cavity (Fig. 8.4).





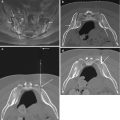
Fig. 8.1
Anatomy of a true rib. Axial CT image reconstructed in the oblique axial plane at the T4 level shows the anatomic parts of a single (fourth) rib. The rib head (h) articulates with the vertebral body at the costovertebral joint (arrow) and the rib tubercle (r) articulates with the vertebral transverse process at the costotransverse joint (curved arrow). The neck of the rib (nk) is located between the head of the rib and the tubercle. The shaft (s) or body is the longest part of the rib. The posterior curve of the rib is referred to as the costal angle (ca). Note that at the level of the upper thoracic spine, the scapula may limit access to the lateral rib from a posterior approach

Fig. 8.2
Anatomy of a false rib. Axial CT image reconstructed in the oblique axial plane at the T8 level shows the anatomic parts of the eighth rib. These are identical to those of the true rib, but there is no direct articulation with the sternum. The shaft(s) is well seen

Fig. 8.3
Anatomy of a floating rib. Axial CT image reconstructed in the oblique axial plane at the T12 level shows segmental visualization of the 12th rib (arrows)

Fig. 8.4
CT cross-sectional appearance of the rib shaft. Reformatted sagittal CT image (a) shows sagittal cross sections of the ribs (arrows). The margin of the rib is comprised of an oval-shaped thick cortical layer of bone that surrounds a small marrow cavity (curved arrow). Coronal reformatted CT image (b) shows the small cross-sectional area (arrow) of each rib and the costal groove (curved arrow) of the rib
A typical rib consists of a rib head, neck, tubercle, and body or shaft (Figs. 8.1, 8.2, and 8.3). The 10–12th ribs possess only a single articular facet on the rib head as compared to the remaining ribs which have two articular facets on the rib head. The rib head articulates with the vertebral body at the costovertebral junction or joint. The rib tubercle, which also has an articular facet, articulates with the vertebral transverse process at the costotransverse junction or joint. The neck or crest of the rib is located between the head of the rib and the tubercle. The shaft or body of the rib commences at the tubercle just beyond the neck and curves around the lateral margin of the thoracic cavity to terminate in the sternal extremity. The initial angle of curvature of the rib is called the costal angle. The undersurface of the rib contains the costal groove. The intercostal vein, artery, and nerve are found underneath the costal groove.
The critical structures that must be considered when performing a rib biopsy are the lungs and the intercostal arteries and veins (Fig. 8.5). The lungs are mostly surrounded by the intercostal muscles. A needle that deflects off of the rounded surface of the rib could readily pass through the very short distance between the muscle and the pleural surface of the lung. Lytic rib lesions can also expose the lung to potential injury during a biopsy procedure. Care must also be exercised when advancing a needle near the inferior or costal groove of the rib as the intercostal neurovascular structures are found in this location. When deciding upon the feasibility of an image-guided percutaneous rib biopsy procedure, the operator must always factor these critical structures into their approach.


Fig. 8.5
Critical structures to consider when performing a rib biopsy. Sagittal reformation in soft tissue algorithm from a contrast-enhanced chest CT study shows the paired intercostal artery and vein (curved arrows) traveling underneath each respective rib. The ribs only protect a small area of lung (arrows)
Critical Structures: Rib Biopsy
Lung
Intercostal vessels
8.3 Indications
Image-guided percutaneous rib biopsy is indicated for the evaluation of pathologic lesions that are located within one or more ribs (Table 8.1) (Edelstein et al. 1985; Faro et al. 1993). The most common indication for performing a rib biopsy is the evaluation of a suspected neoplastic process (Guttentag and Salwen 1999; De Maeseneer et al. 2004). Neoplastic processes within the ribs are usually secondary lesions associated with metastatic disease (Jakanani and Saifuddin 2013; Cronin et al. 2009). Direct extension from a pulmonary malignancy is another possible etiology for a rib lesion. Primary tumors within a rib, though extremely rare, may also require a biopsy procedure (Kim et al. 2008). It is very important to review all of the patient’s imaging studies prior to performing a rib biopsy. The remainder of the body should be studied in order to assess for the presence of other lesions which can be more safely sampled. Since the majority of patients with metastatic disease often have lesions located elsewhere within their bodies, it is more likely than not that these other sites are in better locations for sampling. This accounts for the relatively low frequency of rib biopsy procedures. Rib biopsy procedures are performed when one or more rib lesions are detected on radiologic imaging studies in a patient with either one or more known primary tumors or with no prior history of cancer. The patient’s prior imaging studies (chest radiograph, chest CT, or skeletal scintigraphy) may show only rib lesions, hence the impetus to perform a biopsy procedure in order to determine subsequent patient management, especially in patients with preexisting cancer.
Table 8.1
Indications for image-guided percutaneous rib biopsy
Neoplasm |
1. Solitary rib lesion |
Metastatic disease |
Adult: Lung, breast, thyroid, kidney, prostate, liver Child: Ewing’s sarcoma, neuroblastoma |
Contiguous spread of lung or pleural-based tumor |
Primary osseous neoplasm |
Adult: Chondrosarcoma, myeloma, giant cell tumor Child: Ewing’s sarcoma, osteosarcoma |
Primary benign tumor |
Fibrous dysplasia, hemangioma, Langerhans cell histiocytosis, osteoid osteoma, osteoblastoma, osteochondroma, enchondroma, chondromyxoid fibroma, aneurysmal bone cyst |
2. Multiple rib lesions |
Metastatic disease |
Multiple myeloma |
3. Other |
Pathologic rib fracture vs. benign rib fracture |
Infection: tuberculosis, actinomycosis, bacterial infection |
8.3.1 Contraindications
The major contraindication to performing a rib biopsy is uncorrected coagulopathy (Table 8.2). Because of the challenging nature of rib biopsy procedures, they should not be performed on uncooperative or unstable patients. For lesions that show a benign radiographic appearance, then it might be reasonable to delay if not avoid the rib biopsy procedure. A nondiagnostic biopsy result may be observed when performing biopsies on benign lesions (Omura et al. 2011). In this situation, the patient’s prior radiologic studies should be reviewed to determine if the lesion has always been within the rib and if it is stable in appearance. Alternatively, the rib lesion can be followed at predetermined intervals with imaging surveillance.
Table 8.2
Contraindications to image-guided percutaneous rib biopsy
Absolute |
Uncorrected coagulopathy |
Relative |
Patient factors |
Combative or uncooperative patient |
Clinically unstable patient |
Factors related to the lesion in question |
Probable benign lesion |
Very small lesions (<5 mm in diameter) |
Lesion in other location that is safer to biopsy |
8.4 Risks and Complications Associated with Rib Biopsy and How to Minimize Them
The risks and complications that are associated with image-guided percutaneous rib biopsy are related to potential injury to nearby critical structures (Table 8.3). The proximity of the rib to the lung puts the latter organ at risk for pneumothorax during the biopsy procedure. Fortunately, the occurrence of this complication is rare, and the likelihood of pneumothorax is further decreased by using CT-guidance and tangential coaxial biopsy techniques. The other complication that may occur is vascular injury, particularly to the intercostal vessels. This can result in hemorrhage with hematoma formation.
Table 8.3
Percutaneous rib biopsy – potential risks and complications
Tissue injury |
Pneumothorax |
Vascular injury |
Hemorrhage |
Infection |
Inappropriate needle placement |
Wrong level |
Inadequate tissue sampling |
Technical failure – biopsy system failure, lost specimen |
Radiation exposure |
Anesthesia complications |
Aspiration, airway compromise, respiratory depression |
The risks of image-guided percutaneous rib biopsy can be decreased by using CT-guidance and coaxial biopsy techniques which utilize tangential approaches.
8.5 Imaging Guidance
CT is the most common modality that is used to perform image-guided percutaneous rib biopsy (Jelinek et al. 2002; Hwang et al. 2011). The addition of CT fluoroscopy further improves the efficiency of the rib biopsy procedure. The ability of CT to delineate osseous structures such as the rib makes CT an ideal modality for this procedure. CT provides optimal contrast resolution and is able to readily define the lung fields and intercostal soft tissues. The use of thin section acquisition techniques with immediate reconstruction also contributes to the usefulness of this modality for the purposes of performing a rib biopsy.
Large rib lesions with extraosseous soft tissue components have also been biopsied using ultrasound guidance, in a minority of cases (Jakanani and Saifuddin 2013). The probability of a neoplastic rib lesion increases when there is cortical destruction associated with an extraosseous soft tissue mass though infection may also account for these imaging findings (Lee et al. 1993). Additionally, the diagnostic yield of the biopsy procedure increases when there is an extraosseous soft tissue component and decreases with the presence of only an intramedullary rib lesion (Jakanani and Saifuddin 2013). Lesion access and tissue sampling can be challenging in the latter clinical scenario and are not feasible with ultrasound guidance.
8.6 Approaches
Biopsy approaches to the rib are determined by the lesion location and size. It is, therefore, imperative for the operator to review all pertinent pre-procedure imaging examinations in order to plan the most optimal approach to a rib lesion. The two principle trajectories for rib access are tangential, along the long axis of the rib, and perpendicular (to the rib outer surface – so called short axis) (Table 8.4). The tangential trajectory attempts to obtain a sample without compromising the lung or the vascular pedicle of the rib. This trajectory enables a longer throw of the biopsy needle through the marrow space of the rib. The perpendicular trajectory is direct and has the theoretical potential to puncture the lung or injure the intercostal vessels. This perpendicular trajectory is best reserved for bulky rib lesions or for directly infiltrating lesions from the adjacent pleura or lung (Fig. 8.6). In both of these clinical scenarios, the diameter of the lesion should be large enough to safely accommodate a biopsy needle without injuring the lungs or intercostal vessels.
Table 8.4




Approaches for rib biopsy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree