Preoperative breast imaging evaluation can contribute useful clinical information to the management of the patient with known breast cancer. Breast magnetic resonance imaging (MRI) has been used as part of this imaging evaluation, and the ability of breast MRI to detect otherwise occult multifocal and multicentric disease has been demonstrated in multiple studies. The use of MRI for breast cancer staging remains under debate, however. This article reviews some of the current discussion regarding the use of breast MRI in this patient population. It is important to note that this discussion occurs in an evolving context of surgical and breast conservation therapies.
The main goal of preoperative breast imaging evaluation in the patient with known cancer is to assess accurately the extent of disease. This information then can be used to guide surgical treatment planning. In cases where the disease appears localized, breast-conserving surgery likely will be successful. In contrast, when the disease appears to be multifocal or multicentric, mastectomy likely will be required. In addition, imaging evaluation of the contralateral breast can result in the detection of clinically unsuspected synchronous cancer, which also may affect surgical management.
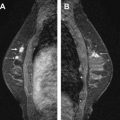
Beyond mammography and breast ultrasound, breast magnetic resonance imaging (MRI) has emerged as a tool that can be applied toward the preoperative imaging evaluation of patients with known cancer. The ability of breast MRI to depict the extent of cancer has been well-documented in the literature. MRI has been reported to detect multifocal disease in the ipsilateral breast in 10% to 44% of cases. The utility of breast MRI in the detection of multicentric disease also has been widely reported, with additional cancer detected in 11% to 54% of cases. In addition, many of these cases were MRI-demonstrated but mammographically and clinically occult ( Figs. 1 and 2 ). Given the potential of MRI to detect unsuspected multifocal or multicentric cancer, it has been suggested that the addition of MRI to the preoperative imaging work-up of patients with newly diagnosed breast cancer can aid in surgical and definitive treatment. This implies that breast MRI has the theoretical potential to reduce the number of surgical procedures to obtain negative margins of resection or to convert patients from planned breast-conservation therapy (BCT) to mastectomy when multifocal or multicentric cancer is found. It also has been postulated that the detection of additional areas of cancer in the ipsilateral breast on MRI may result in a lower rate of in-breast recurrence following BCT.


In addition to evaluating the extent of disease in the ipsilateral breast, it also has been demonstrated that MRI can be used to evaluate the contralateral breast. Historically, the reported incidence of synchronous bilateral breast cancer detected on physical examination or mammography is 3% to 6%. With the application of breast MRI, there are now multiple single-institution and multicenter trial reports indicating the ability of MRI to detect synchronous cancers in the contralateral breast that were otherwise mammographically and clinically occult. Rates of approximately 3% to 19% of patients examined have been reported. The study by Lehman and colleagues had the largest number of patients (969), and the rate of contralateral disease detected by MRI was 3.1%. Approximately half of the lesions detected on MRI have been invasive cancers, and the other half have been ductal carcinoma in situ (DCIS). Breast MRI can detect synchronous cancers in the contralateral breast, information that can help to optimize clinical therapy for the patient.
Pitfalls of MRI staging of breast cancer
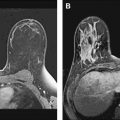
One of the major limitations of MRI of the breast is false-positive enhancement of benign lesions, including fibroadenomas, fat necrosis, fibrocystic changes, and presumably normal breast tissue. False-positive enhancement is one main pitfall in the application of MRI for breast cancer staging ( Fig. 3 ). False-positive rates in the setting of breast cancer staging have varied among studies, with an average rate of approximately 20%. In a study of 70 women with percutaneously diagnosed breast cancer who were being considered for BCT, MRI detected additional sites of cancer in the ipsilateral breast in 27% of patients. Biopsy was recommended for MRI-detected additional lesions in the ipsilateral breast in 51% of women. The positive predictive value (PPV) was 52%, with an overall rate of 24% of women with MRI-recommended biopsies for findings that ultimately were found to be benign. The PPV was higher for lesions in the same quadrant as the index lesion as compared with lesions in different quadrants (64% vs 31%). A similar finding was reported by Bedrosian and colleagues, where a higher percentage of enhancing lesions in the same quadrant as the index cancer were malignant compared with findings in a different quadrant.

Despite the relatively high PPV for breast MRI that is higher than the reported PPV for mammographically detected suspicious lesions, these reports that demonstrate the performance of breast MRI also indicate that many of these recommended biopsies for MRI-detected suspicious lesions will yield benign results. Thus, there is still potential theoretical delay in definitive surgical therapy for these patients with additional enhancing findings detected on preoperative breast MRI, especially if the findings are found to be benign. False-positive MRI findings in the setting of breast cancer staging may result in high cost, increased patient anxiety, additional surgical procedures that may compromise the cosmetic results for those patients who do undergo BCT, and potentially an increase in the mastectomy rate. The range of these costs and the quantifiable potential impact on patient management remain to be determined definitively.
Impact of preoperative breast MRI on clinical management
Multiple studies demonstrate that the addition of MRI will result in a change in therapeutic approach, with reported rates of change ranging from 4% to 43%, with most of these rates at about 20%. The findings on MRI were reported as true positive in 4% to 32% of cases, and false positive in a lower percentage. In cases where the enhancement proved to be benign, this resulted in unnecessary additional surgery, or delay in definitive surgery because of the need for percutaneous biopsy.
Given that there are false positives in breast MRI, a caveat to keep in mind is that before any final surgical treatment decision, tissue diagnosis should be obtained of suspicious findings if the results will affect clinical recommendations relating to BCT versus mastectomy. Balancing the known pitfalls of breast MRI and its false positives with the clinical goal of accurate assessment of extent of disease is also an evolving process, and an area of continued investigation.
Impact of preoperative breast MRI on clinical management
Multiple studies demonstrate that the addition of MRI will result in a change in therapeutic approach, with reported rates of change ranging from 4% to 43%, with most of these rates at about 20%. The findings on MRI were reported as true positive in 4% to 32% of cases, and false positive in a lower percentage. In cases where the enhancement proved to be benign, this resulted in unnecessary additional surgery, or delay in definitive surgery because of the need for percutaneous biopsy.
Given that there are false positives in breast MRI, a caveat to keep in mind is that before any final surgical treatment decision, tissue diagnosis should be obtained of suspicious findings if the results will affect clinical recommendations relating to BCT versus mastectomy. Balancing the known pitfalls of breast MRI and its false positives with the clinical goal of accurate assessment of extent of disease is also an evolving process, and an area of continued investigation.
Preoperative staging with breast MRI—current controversies
The data are clear that MRI permits detection of mammographically, sonographically, and clinically occult multifocal cancer in selected patients with presumed unifocal disease. There is an ongoing debate, however, over the use of MRI for preoperative cancer staging. Much of the controversy appears to center around the clinical impact of the additional sites of disease that are detected only on MRI. In terms of short-term benefit, will the addition of MRI result in improved surgical planning, ultimately resulting in a decrease in number of surgical procedures to obtain negative margins? In terms of long-term benefit, will the addition of MRI result in reduced recurrence rates and improved overall survival?
Investigation into the use of MRI for preoperative breast cancer staging has demonstrated both negative and positive results. In one study that compared patients who underwent surgery with and without a routine preoperative MRI, MRI use was reported to not be associated with improved margin status, but instead was reported to be associated with a treatment delay and an increased mastectomy rate. In addition, a recent meta-analysis of breast MRI accuracy and impact on surgical management reported an 11.3% conversion rate from wide local excision to more extensive surgery. This analysis also alluded to the false positives that MRI finds, and concludes that additional studies need to be done.
Recently, a multicenter, randomized controlled trial was reported from the United Kingdom. The comparative effectiveness of MRI in breast cancer (COMICE) trial included approximately 1623 women with a breast cancer diagnosis, with 816 patients receiving a preoperative breast MRI, and 807 not receiving one. The group without preoperative MRI underwent conventional breast imaging with mammography and ultrasound. Reoperation rate within 6 months was reported as 19% in the MRI group, and 19% in the group without a preoperative MRI. The conclusions included that no significant benefit in terms of reduction in reoperation rate was achieved with use of preoperative breast MRI.
As counterpoint, however, a report of preoperative MRI associated with more completely excised invasive cancer also has been published. In addition, preoperative MRI again has been reported to be useful in the surgical management of patients eligible for different management choices. Furthermore, a prospective single-institution study also was reported recently by Siegmann and colleagues that assessed that location’s experience with the impact of preoperative bilateral breast MRI on the clinical management of patients. They reported that the findings of preoperative breast MRI examinations changed the clinical management in 48 of the 119 study patients (approximately 40%). In 36 of these women, additional sites of malignancy were demonstrated that clarified the surgical management (17 with conversion to mastectomy). In 12 patients, the MRI-detected lesions ultimately were found to be benign. In comparison to the 30.3% of patients where breast MRI clarified the extent of the malignancy by detecting additional sites of malignancy, the false positives in 10.1% of patients was deemed relatively acceptable.
Also important to remember is that the increased use of breast MRI may not be the only factor influencing changes in surgical management and the reports of increased mastectomy rate. In another recently published analysis, the year of surgery and a preoperative breast MRI were reported as independent significant predictors of the type of surgery a breast cancer patient received. Although patients with an MRI were reported to be more likely to undergo mastectomy than those without (54% vs 36%, P <.0001), the year of surgery (2004 to 2006) at this institution also was associated with an increased mastectomy rate (29% in 2003 to 41% in 2006, P <.0001). In this latter group, the rate of mastectomy increased in patients without MRI . Factors such as increased awareness and information about genetic status and family history have been discussed as possible influences on this trend, with potential choices for mastectomy being made even for early stage breast cancer, and even without a breast MRI. Furthermore, increased knowledge about and development of breast reconstruction options also may factor into any trend in increased mastectomy rates. A recent report suggests that women are much more likely to choose mastectomy when informed with breast reconstruction options. Thus, there also may be other variables and influences on the recently reported increase in mastectomy rate for breast cancer patients beyond breast MRI.
There are many potential explanations for these conflicting reports on the impact of preoperative MRI on surgical management. One explanation may be differences in patient populations in each study. It is possible that the selective application of breast MRI in certain populations will help optimize the use of this tool in the preoperative breast imaging evaluation of the patient with known cancer. It is also important to note that no imaging test is universally 100% sensitive and 100% specific. Given the variable histology of breast cancer, individual patient variability, and variation in current clinical application, there is much to influence the false-positive rate of any breast imaging study, including breast MRI. Further investigation needs to be done in the application of breast MRI in patients with known breast cancer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree