Clinical Presentation
The patient is a 49-year-old woman who presented with intermittent low back pain, right more than left, with radiation to the lateral hips but no radiation below the knee. This started without precipitating event as best as she is able to recall. It has gotten worse over the past 10 months. She describes intermittent dull discomfort that can sometimes be burning. The severity fluctuates from mild to quite severe. Prolonged standing, walking, and transitional movements make her symptoms worse. She has tried several over-the-counter and narcotic medications without benefit. She denies any paresthesias, weakness, or radicular features. She denies any bowel or bladder dysfunction and no saddle anesthesia. No recent fevers or infection. She has had a 40-pound weight gain since her pain complaints started.
Imaging Presentation
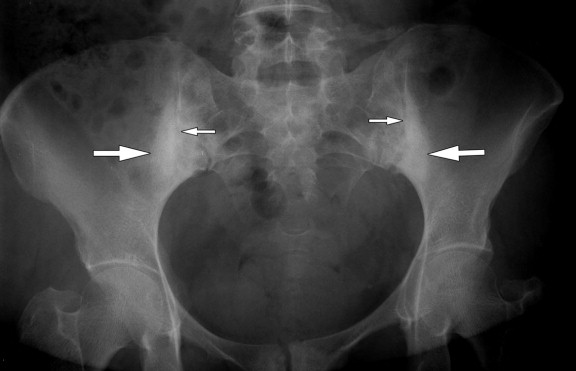
Frontal radiograph of the pelvis reveals sclerosis about both sacroiliac joints. There are also small irregularities along the margin of both sacroiliac joints consistent with erosions ( Fig. 63-1 ) .
Imaging Presentation
Frontal radiograph of the pelvis reveals sclerosis about both sacroiliac joints. There are also small irregularities along the margin of both sacroiliac joints consistent with erosions ( Fig. 63-1 ) .

Discussion
The sacroiliac joint (SIJ) is the largest joint in the axial skeleton. The inferior two thirds of the SIJ are lined by articular cartilage and the upper third is a syndesmosis. The lower portion is often called a diarthrodial joint , however, only a portion of the SIJ has a true synovial-lined joint capsule. The majority of the lower SIJ is like a symphysis, lined with hyaline cartilage and held together by fibrous tissues. The cartilage is thinner on the iliac side of the joint, which is why degenerative change is seen much earlier on the iliac side of the joint. Only the inferior few centimeters is a true chondral joint from front to back. The sacrum and ilium are held together in the syndesmotic portion by the interosseous ligament. The entire joint is also supported by strong anterior and posterior sacroiliac ligaments and the sacrospinous and sacrotuberous ligaments. The SIJ ligamentous structure is more extensive dorsally because a posterior capsule is either absent or rudimentary. The main function of the SIJ ligamentous structure is to limit motion in all directions. This ligamentous structure is weaker in women to allow mobility for birthing. Several muscles, including the gluteus maximus, piriformis, and biceps femoris muscles, help stabilize the SIJ and are connected to SIJ ligaments. The innervation of the SIJ is often debated. Most agree that the lateral branches of the L4-S3 dorsal rami supply innervation to the posterior joint; however, some believe L3 and S4 also give posterior joint supply. Multiple studies debate anterior innervation ranging from L2-S2, L4-S2, and L5-S2, and some who believe there is no innervation anteriorly.
Pain related to the SIJ is not uncommon. Studies based solely on physical examination, fluoroscopically guided SIJ injections of local anesthetics in joints that were abnormal on post-arthrography computed tomography (CT) and with concordant pain during joint distension, and unilateral SIJ blocks using International Spine Intervention Society guidelines place the prevalence of SIJ dysfunction from 15% to 30% of patients presenting with chronic low back pain.
Studies have shown that examination the patient history and physical are unable to consistently identify patients with SIJ pain. SIJ pain crosses over with many other causes of low back pain. The most common pain pattern for SIJ dysfunction is radiation into the buttocks (94%), lower lumbar region (72%), lower extremity (50%), pain radiating below the knee (28%), groin (14%), foot pain (12%), upper lumbar region (6%), and abdomen (2%). The most common finding in SIJ dysfunction is unilateral pain below the level of L5. “Risk factors associated with SIJ pain include leg length discrepancy, gait abnormalities, prolonged vigorous exercise, scoliosis, spinal fusion to the sacrum, and pregnancy because of increased weight gain, exaggerated lordosis, hormonal ligamentous laxity, and trauma from birth.”
Osteoarthritis is one of the most common disorders to affect the SIJ. Osteoarthritis is usually seen in patients older than 40 years of age. The main findings of osteoarthritis of the SIJ are joint space narrowing, subchondral sclerosis, and anterior osteophytes. When the osteophytes get larger, they can fuse anteriorly. Osteoarthritis is distinguished from the inflammatory arthritides in that intra-articular ankylosis is not a feature of osteoarthritis. Gas can be seen in the SIJ space in osteoarthritis.
The SIJ is often involved with the HLA-B27 inflammatory arthritides, most commonly ankylosing spondylitis (AS). The sacroiliitis related to AS is usually bilateral and symmetric. Patients with inflammatory bowel disease and approximately 5% to 15% of patients with Crohn’s disease and ulcerative colitis can develop a sacroiliitis indistinguishable from AS. Interestingly, 50% of patients with Crohn’s disease and ulcerative colitis carry the HLA-B27 antigen. Sacroiliitis is also seen in patients with psoriatic arthritis and Reiter’s syndrome, but is distinguished from AS by being bilateral and asymmetric. Sacroiliitis is unusual with rheumatoid arthritis. People with Behçet’s syndrome, relapsing polychondritis, and systemic lupus erythematosus can also demonstrate sacroiliitis. Infection can cause a septic arthritis that is usually unilateral.
Imaging Features
The imaging findings of sacroiliitis are erosions along the joint margin. The erosions are identified earlier on the iliac side of the joint because the cartilage is thinner on the iliac side. The joint can have a fuzzy appearance on plain radiographs (see Fig. 63-1 ). There may be pseudo joint space widening due to the erosions. In the late stages, ankylosis of the joint can be seen. Plain radiographs are widely used and most cost-effective in the screening for sacroiliac joint disease. However, there are significant interobserver and intraobserver variations in interpretation. In one study, 20% of radiographs incorrectly underdiagnosed sacroiliitis when compared with computed tomography (CT) results. Plain radiographs also have very poor sensitivity in the early stages of sacroiliitis, which is why, in the past, there was between a 2- to 7-year lag between the diagnosis and presentation. SIJ radiographs are used to categorize sacroiliitis into five grades: grade 0 (normal), grade 1 (suspicious, unclear), grade 2 (small erosions, hypersclerosis), grade 3 (definite erosions, pseudodilitation of the joint space), and grade 4 (ankylosis).
Nuclear medicine bone scan has been used in the past in the diagnosis of SIJ inflammatory disease; however, it has been shown to be too nonspecific of an examination and has many factors that can influence the imaging interpretation. “For example, hopping on one leg before an examination will increase the uptake of the radionuclide .”
CT is more sensitive and specific in evaluating the early erosions and sclerosis seen with sacroiliitis ( Fig. 63-2 ) . However, two disadvantages of CT are the radiation dose and the inability to detect changes of synovitis and marrow edema that can be detected with magnetic resonance imaging (MRI). Both CT and MRI can demonstrate the anterior osteophytes commonly associated with SIJ osteoarthritis.











