Chapter 3
Safety of MRI and CT
Ersan Altun and Richard C. Semelka
The University of North Carolina at Chapel Hill, Department of Radiology, Chapel Hill, NC, USA
In recent years, diagnostic imaging safety has garnered considerable interest in medical literature because of concerns of health risks attributable to imaging investigation. Perhaps the greatest concern is the likelihood of cancer development, secondary to the use of increasing numbers and exposures of medical radiation, especially resulting from the increasing use of multislice CT scanners. Additional health concerns are the toxicity of iodine-based contrast agents (IBCAs) that are used in CT, and gadolinium-based contrast agents (GBCAs) that are used in MRI. The discovery in 2006, after 16 years of clinical use, of the association of the development of nephrogenic systemic fibrosis (NSF) in patients with renal impairment following the administration of GBCAs, stimulated unprecedented alarm in the imaging sphere among physicians and patients. This was especially vexing, as for many years GBCAS were considered the safe alternative to IBCAs.
Perhaps all of these concerns are sobering reminders that nothing is 100% safe, and we have to be constantly vigilant on the subject of patient safety. In this chapter we discuss many of these issues.
Toxicity of contrast agents
Iodine based contrast agents
IBCAs, which are the primary agents used in CT examinations, are the most commonly used contrast agents in routine daily practice. The risks of adverse reactions, contrast induced nephropathy (CIN), and possible drug interactions, have garnered attention, and may be especially important because of the large number of studies performed. Prevention or minimization of these complications is important.
Allergy-like acute adverse reactions
Allergy-like acute adverse reactions typically manifest themselves shortly after the administration of an IBCA, with signs ranging from urticaria to an anaphylactoid process characterized by life threatening bronchospasm, laryngeal edema, and hypotension (1, 2). The majority of adverse side effects are mild to moderate, non-life-threatening events, occurring in about 30% of studies, and require only observation, reassurance, and support. Virtually all life-threatening reactions occur immediately, or within the first 20 min, after IBCA administration (3, 4). Histories of allergies and previous reactions have served as predictors for the possible development of adverse reactions. Although a history of multiple severe allergies does increase the risk of a reaction following contrast agent injection, only a small percent of patients with severe adverse reactions to IBCAs have a strong history of allergies, and only a small percentage of patients with allergies will develop reactions to IBCA (1). Most reactions in these patients are also minor. A history of asthma is also considered to be a good predictor of increased risk of reactions to IBCAs (1–4). Fortunately, asthmatics are generally familiar with the use of β-agonist inhalers and usually have one with them. Nevertheless, such inhalers should be available where contrast media (CM) are administered (2). Patients who have experienced an allergy-like adverse event after IBCA injection are unlikely to experience a similar or more severe reaction if an IBAC is injected again (1). In fact, although a prior reaction remains the best predictor of a future adverse event, the likelihood of a recurrent reaction is in the range of 8–25%. If the previous reaction was caused by a true allergy, the risk would approach 100% (1, 2). Therefore, if the patient has had a prior reaction to an IBCA, it is not necessary to avoid any further contrast agent injection in most cases, unless the reaction has been a major one. The use of a different IBCA is a reasonable approach, although it is often impossible to define either the specifics of a prior reaction or the specific contrast agent used. The use of non-ionic low osmolality contrast agents has been shown to reduce the risk of acute adverse reactions and CIN (5, 6). The use of a pre-treatment regimen, including administration of corticosteroids with or without antihistamines or other medications, has been shown to be safe and effective in preventing minor adverse events (7, 8). Prospective studies of pre-treatment have involved too few patient numbers, considering the rarity of life-threatening occurences, to determine whether pre-treatment with steroids prevents life-threatening reactions (7, 9). There is evidence from a large prospective registry, however, that they do not (1). If pre-treatment is to be used, its use should begin about 12 h before contrast agent injection, to prevent minor adverse events (7), as shorter pretreatment regimen may not be effective. It is crucial that a trained health care worker be ready and able to treat an on-going life threatening reaction (3, 4).
Contrast induced nephropathy (CIN)
CIN is defined as iatrogenic renal function impairment following exposure to CM, and the vast majority of cases have been related to IBCA use. Theoretically they also may occur with high dose GBCAs (10–12), but in the current era of NSF-concern, effectively no high dose GBCA studies are performed any more. CIN occurs much more commonly following the administration of IBCAs compared to GBCAs, but this likely reflects a dose-related phenomenon rather than intrinsic safety of the agent per se (13–15). CIN resulting from exposure to IBCAs is the third most common cause of acute renal failure in hospitalized patients, after impaired renal perfusion and the use of other nephrotoxic drugs (10–13, 16).
The diagnosis of CIN includes three components: (i) an acute deterioration of renal function, (ii) a temporal relationship with the parenteral administration of CM, and (iii) the exclusion of alternative etiologic reasons which may result in the acute deterioration of renal function (10–12). The acute deterioration of renal function is described as a relative increase of 25% or more, or an absolute increase of 0.5 mg/dl or more from baseline in serum creatinine value (10–12). The acute deterioration of renal function in CIN develops within the first 24 h in 80% of patients, and may persist to 48–72 h in 20% of patients (10). Recently, caution has been suggested in the interpretation of an elevation of serum creatinine value, as fluctuations may occur in the normal state of the patient independent of CM use (17).
The pathophysiology of CIN remains uncertain (18, 19). The proposed mechanisms include toxic injury to renal tubules, ischemic injury, or decreased renal medullary perfusion (18, 19). It has also been reported that osmolality and viscosity of iodinated CM is also responsible in the pathophysiology, with higher viscosity having a greater likelihood of causing this condition (20). As the glomerular filtration rate (GFR) decreases, the risk of CIN increases; and the risk particularly increases when the GFR is below 60 ml/min/1.73 m2 (10).
The incidence of CIN varies according to the type of IBCA used. Earlier literature emphasized a risk stratification based on IBCA osmolarity, with higher risk in high-osmolar compared to low- or iso-osmolar agents (13). The incidence of CIN is two times higher with the use of high-osmolality IBCA (HOCM) compared to that of low-osmolality IBCA (LOCM) (13). HOCM has been largely replaced with LOCM because of their higher nephrotoxicity, lesser patient tolerance, and higher risk of adverse reactions (13).
The incidence of CIN following the intra-arterial or intravenous use of LOCM has been reported to vary between 0.6 – 2.3% in patients with normal renal function (10). In patients with decreased renal function, the incidence of CIN following the intra-arterial and intravenous use of LOCM has been reported to vary from 3% to 50% and 1% to 21%, respectively (13, 21). The intra-arterial administration of LOCM has been reported to have a two times higher incidence of CIN compared to intravenous administration (10), which may in part reflect that administration rates and volumes are not as tightly controlled, and may be much higher than with intravenous administration.
The incidence of CIN following the use of iso-osmolality CM (IOCM) and LOCM is similar in patients with normal renal function (13, 21). Although the incidence of CIN with IOCM has been reported to be lower in patients with decreased renal function compared to LOCM in a few studies, other studies have shown the opposite effect, apparently influenced in part by the sponsor of the study. There is no definite evidence that IOCM are safer in patients with decreased renal function compared to LOCM (21, 22).
CIN is by definition an acute event, but the critical aspect of this condition is the long-term consequences and residual renal impairment. Few studies have been conducted to evaluate the long term outcome of CIN. Residual renal impairment may be seen in 30% of patients with CIN (16). CIN that requires dialysis may be observed in 3% of patients who have underlying renal impairment (16). Hospital mortality rate has been reported to be between 7 and 34% for in-patients secondary to CIN alone, 15% for patients with underlying renal impairment alone, and 36% for patients who require dialysis secondary to CIN (16, 23). One-year mortality rate has been reported to be 38% for patients with renal impairment, and 45% for patients with renal impairment requiring dialysis (16). These numbers are comparable to the mortality rates of NSF.
The much lower incidence of CIN following exposure to GBCAs reflects primarily that in the doses that GBCAs are administered, these agents are less nephrotoxic than IBCAs at the dosages they are administered, which may be 10–20 times the volume of contrast compared to MRI (13–15).
Gadolinium-based contrast agents (GBCAs)
Toxicity can generally be categorized as acute, subacute, and chronic, where the time of occurrence of the complication determines this categorization. Acute toxicity generally occurs within 48 h (often within minutes) and these are generally manifest clinically as acute adverse events that are classified as mild, moderate, and severe. Subacute toxicity generally occurs from 1 week to several months. NSF is the major subacute toxicity. It is not known whether there is substantial chronic toxicity of GBCAs, and this may relate to bone deposition, and perhaps other organs like the liver.
Acute toxicity
The acute adverse reactions seen following GBCAs are allergy-like (urticaria), or unpleasant sensation-related, such as nausea, vomiting, headache, and altered taste sensation. Nausea, which is quite common with needle sticks in general, and vomiting, have served as a great source of concern with various GBCAs, and perhaps most of this is driven by sales individuals from the various manufacturers of these agents. Nausea and head-aches are also often referred to as side-effects and not adverse events, and these are relatively common. True acute adverse events are uncommon, and are usually mild to moderate in severity. Severe reactions, anaphylactoid types, are extremely rare (0.01–0.001%), which is a factor of 10 more safe than IBCAs (4). An increased frequency in adverse reactions has been observed in patients with a history of reactions to either GBCAs or IBCAs, and also a modest increased chance of adverse reactions is observed in patients with a history of allergies, as described with IBCAs. In patients with a history of previous GBCA reaction, a different MR contrast agent should be used, and 12–24 h of premedication with corticosteroids and antihistamines should be considered (4). This would be most prudent in patients with a prior moderate to severe reaction, because second reactions to GBCAs tend to be more severe than the first (4). Severe reactions should be treated very carefully and require the assistance of a resuscitation team.
GBCAs are generally considered to have no nephrotoxicity at approved dosages for MR imaging (4).
Subacute toxicity
Nephrogenic systemic fibrosis (NSF)
NSF is a systemic disease characterized by widespread tissue fibrosis (24–27). To date, it has been exclusively seen in patients with renal impairment (24–27). The progressive fibrosis results from the deposition of collagen in tissues, and initially and predominantly affects the skin (24–27). Systemic involvement, including the muscles and internal organs such as heart, lungs, and esophagus, generally follows after skin involvement (24–28). The incidence of NSF varies according to the type of GBCA administered (29). The incidence of NSF has been reported to be 2–7% in patients with renal impairment following the use of Omniscan, which has been the agent most often reported to be associated with the development of NSF (28, 30).
Diminished renal function and GBCAs are the two crucial factors necessary for the development of NSF (31, 32). Because NSF does not develop in all patients who have diminished renal function and prior GBCA exposure, it has been considered that additional cofactors might be involved in the pathophysiology (27), although most experts down-play the role of co-factors.
NSF is seen in patients with acute or chronic kidney disease (renal insufficiency), in whom the GFR is less than 30 ml/min/1.73 m2 (29, 33). Additionally, NSF is also seen in patients with acute renal insufficiency of any severity (29, 33). More correctly though, the expression “of any severity” reflects that the actual dysfunction of kidneys in the acute setting is difficult to impossible to ascertain as it may be a rapidly changing/evolving process, hence acute renal sufficiency may represent ‘extreme’ renal failure, despite what lab values may suggest. Patients with GFR above 60 ml/min/1.73 m2 have not been reported to develop NSF (29, 33). More than 95% of NSF patients have stage 4 and 5 chronic kidney disease, with the great majority of these having stage 5 chronic renal disease and/or on renal dialysis (Table 3.1) (27, 33).
Table 3.1 Stages of chronic kidney disease.
| Stage | Description | GFR, ml/min/1.73 m2 |
| 1 | Slight kidney damage with normal or increased filtration | More than 90 |
| 2 | Mild decrease in kidney function | 60–89 |
| 3 | Moderate decrease in kidney function | 30–59 |
| 4 | Severe decrease in kidney function | 15–29 |
| 5 | Kidney failure requiring dialysis or transplantation | Less than 15 |
Diminished renal function has the effect of decreasing renal excretion of gadolinium, which results in an increased half-life in the body (30, 34). The level of renal dysfunction is correlated with the risk of developing NSF, and the severity of NSF; that is, the worse the renal function, the higher the risk and severity of NSF (29, 33, 36).
Extreme caution is also recommended in pregnancy and in children < 1 year of age. Because GBCAs can cross the placenta, enter fetal circulation, and stay in the amniotic fluid for a long time in pregnant patients, the half-life of gadolinium is longer in pregnant patients and in embryos or fetuses (29, 35). The half-life of gadolinium is likely longer in children under age of 1 as well due to their immature renal function (29).
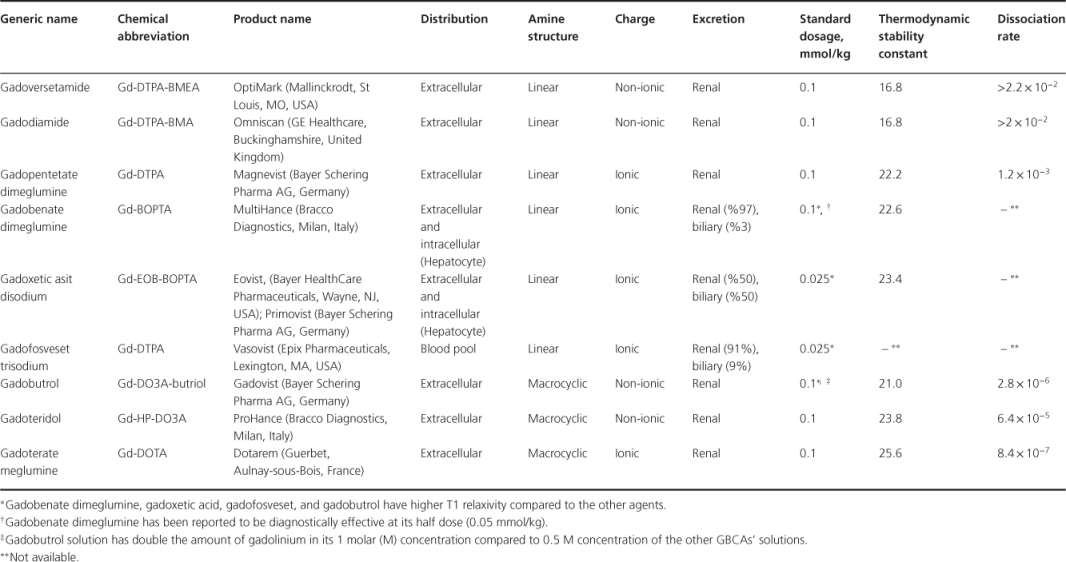
The dissociation of gadolinium ions from gadolinium-chelate complexes varies for different types of GBCAs and can be defined by the thermodynamic stability constant and dissociation constant (38). Thermodynamic stability constant determines the concentration at which gadolinium ions will dissociate from gadolinium-chelate complexes (38). The rate of this dissociation reaction is dependent on the dissociation constant. Taken together, these two constants define the affinity of ligands for gadolinium ions at the physiological pH (38). Each GBCA has a different thermodynamic stability constant and dissociation rate (Table 3.2) (38). Because the specific type of GBCAs with lower thermodynamic stability and higher dissociation constants are more commonly associated with the development of NSF, the dissociation of gadolinium ion from gadolinium-chelate complexes has been considered the trigger
Table 3.2 Categorization of GBCAs according to the distribution in the body, chemical structure, elimination pathway, thermodynamic stability, and dissociation rate