Salivary Glands
The major salivary glands include the parotid, submandibular, and sublingual glands. The parotid gland is artificially divided into deep and superficial lobes by the facial nerve. The main duct of the parotid gland is Stensen duct, which runs anteriorly to pierce the buccinator muscle and open into the vestibule opposite the second maxillary molar. The main duct of the submandibular gland is Wharton duct, which opens at the top of a small papilla in the sublingual space.
With inflammation and infection, a salivary gland will be enlarged and, on CT, demonstrate increased attenuation. Eighty percent of salivary glands stones occur in Wharton duct ( Fig. 2.90 ) with only 15% in Stenson duct ( Fig. 2.91 ). The majority of salivary gland stones are radiopaque. Sialolithiasis (salivary stones) presents clinically with pain and swelling and, when untreated, can lead to infection of the involved gland. Sjögren syndrome is a chronic systemic autoimmune disease, with bilateral enlargement of the parotids due to multiple cystic and solid lesions, occasionally associated with calcifications. Five percent of patients with HIV develop benign lymphoepithelial lesions, specifically multiple cystic and solid masses within and enlarging the parotid glands. This is often accompanied by tonsillar hyperplasia and benign, reactive cervical adenopathy.

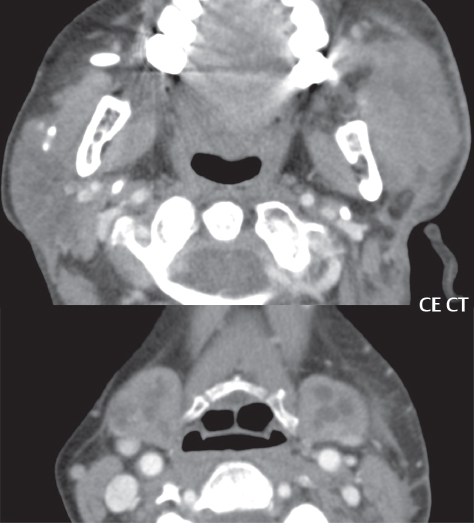
A ranula is a mucous retention cyst (mucocele) of the sublingual gland, which occurs due to rupture of the salivary gland duct (usually caused by trauma). A “simple” ranula is most common, and is confined to the sublingual space ( Fig. 2.92 ). These may be difficult to differentiate from epidermoid cysts, which are common in this location, but fat- containing dermoid cysts are easily distinguished. A “diving” or “plunging” ranula forms following rupture of a simple ranula and presents in the submandibular space, often with a residual tail in the sublingual space.
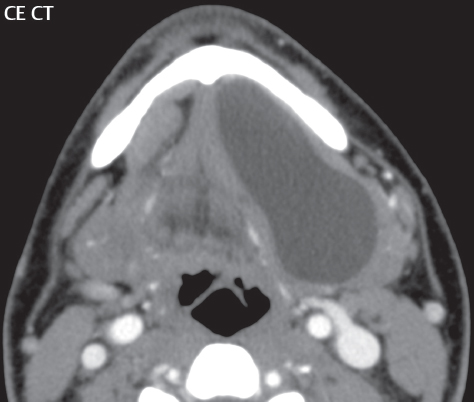
A good general rule is that the smaller the salivary gland, the greater the likelihood of malignancy, when a mass is detected. A benign mixed tumor (pleomorphic adenoma) is the most common salivary gland tumor. The majority occur in the parotid gland, with most in the superficial lobe. On imaging they are solitary, ovoid, and well-demarcated ( Fig. 2.93 ).

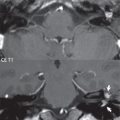
On CT, these will be higher in attenuation than the adjacent parotid tissue. On MR, the most common appearance is a lesion with low signal intensity on T1, intermediate to high signal intensity on T2, with moderate contrast enhancement. Warthin tumors are the second most common type of benign parotid lesions. These lesions arise from intraparotid lymph nodes and are isolated to the parotid gland as other salivary glands do not contain lymph nodes ( Fig. 2.94 ). A classic presentation is that of a well-marginated, heterogeneous, parotid tail mass (although these can be located anywhere within the parotid, or adjacent to the parotid). Overall, they appear more complex than benign mixed tumors. Multiple lesions, unilateral or bilateral, occur in 20% to 30% of cases. Two malignant salivary gland tumors are of note, although much less common than benign tumors, mucoepidermoid and adenoid cystic carcinomas ( Fig. 2.95 ).


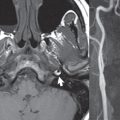
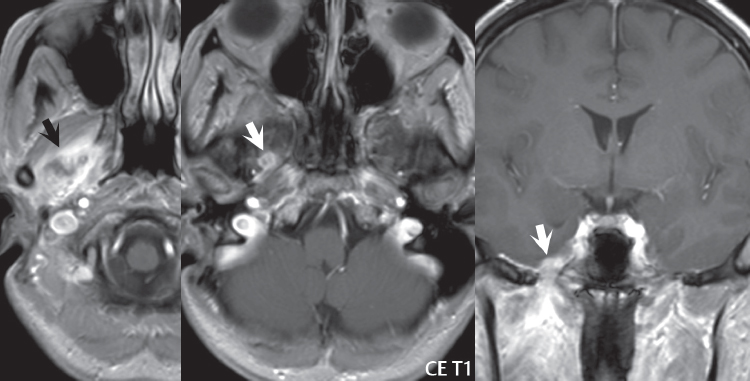
Perineural spread is particularly common with adenoid cystic carcinoma ( Fig. 2.96 ). Although lesion heterogeneity and ill-defined lesion margins favor more aggressive lesions in the salivary glands, low-grade malignant salivary gland tumors may have an imaging appearance indistinguishable from benign masses, being well-circumscribed, homogeneous, and enhancing. Metastases to intraparotid lymph nodes may occur as they represent first order drainage from malignancies of the face, auricle, and scalp.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree