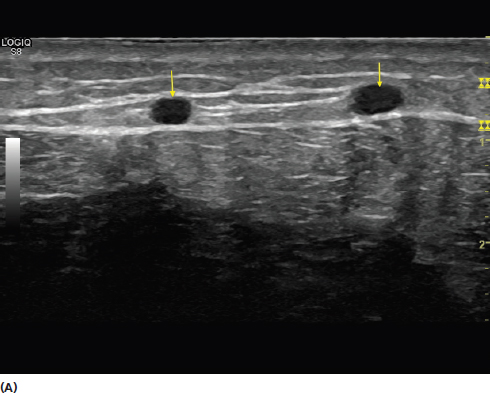
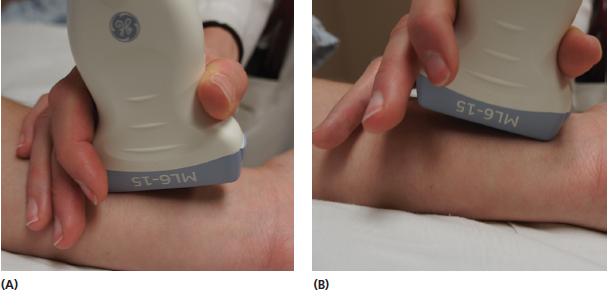
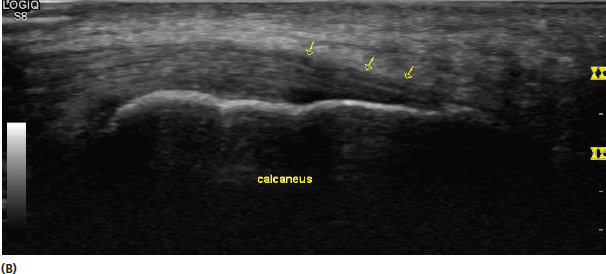
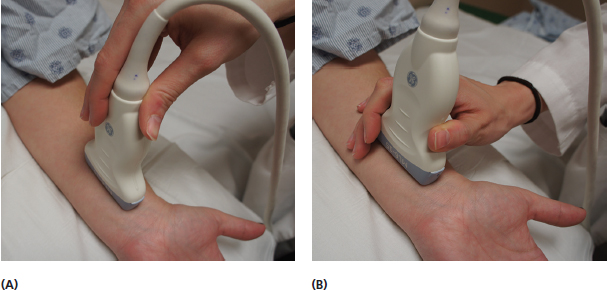
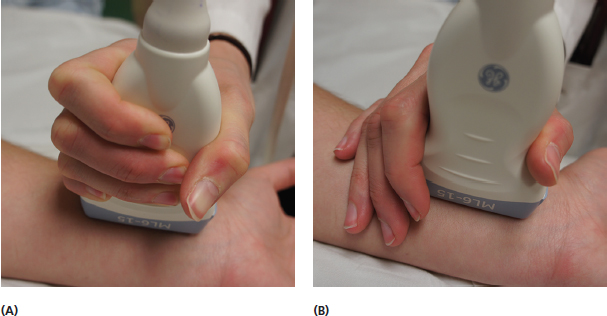
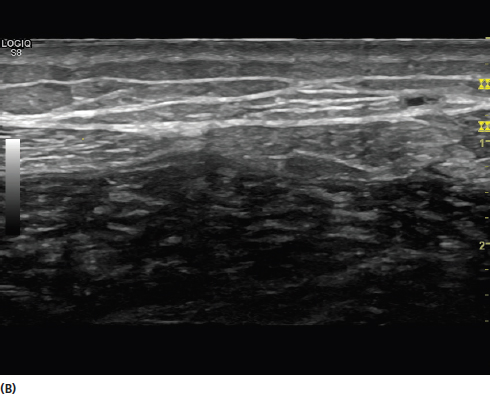
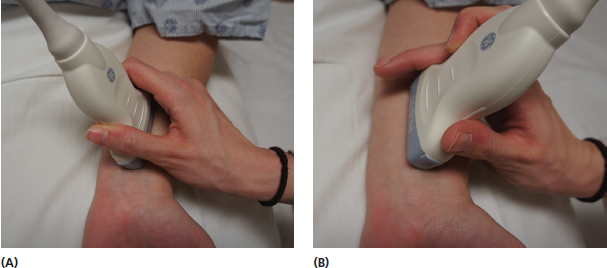
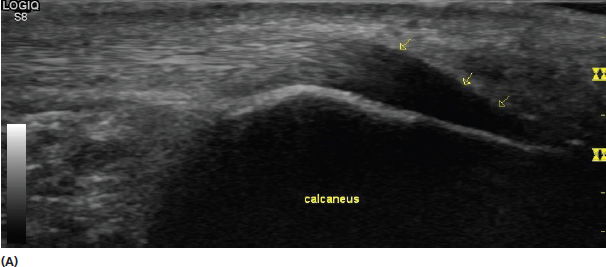
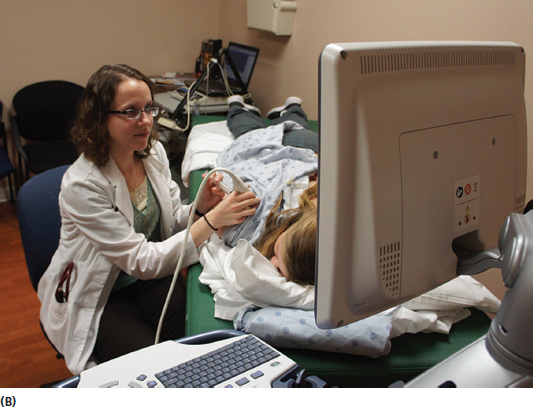
Development of proper positioning and scanning early on in training is paramount to success later on. The goal should be to have an arrangement in which both the patient and examiner are comfortable to make image acquisition easily and efficiently. Proper mechanics will help prevent fatigue, strain, and overuse injuries common to ultrasonographers. Attention should be given to the manner in which the transducer is held and moved. Both the patient and examiner should be placed in proper position in relation to the screen and controls. Successful scanning requires an effective grip on the transducer. Novice scanners tend to hold the transducer inappropriately and with a grip that is too tight. The transducer should be held at the base to facilitate control (Figure 5.1). The grip should be firm without squeezing the transducer. In the same fashion as it is difficult to write well while gripping a pen too tightly, it is difficult to scan easily with good control while doing this with the transducer (Figure 5.2). It is also helpful to maintain contact with the patient while scanning to maintain stability and prevent the transducer from moving or rotating out of the image desired. Contacting the patient with the small and ring fingers and ulnar aspect of the hand while gripping the transducer with the thumb, index, and long fingers provides stability and optimizes scanning control. The examiner should also resist the urge to apply excessive pressure with the transducer as this can deform the image (Figure 5.3). FIGURE 5.1 Pictures demonstrating the incorrect (A) and correct (B) methods of holding the transducer for optimal stability and control. In (A), the examiner is holding the transducer too far from the base and does not have contact with the patient. In the appropriate hand position in (B), the examiner has a comfortable grip of the transducer at its base with the thumb, index, and long fingers while maintaining good contact with the patient with the small and ring fingers and ulnar portion of the hand. FIGURE 5.2 Pictures demonstrating excessive (A) and appropriate (B) grip when holding the transducer. In (A), the examiner is grasping the transducer with excessive grip resulting in more difficulty performing smooth transducer movements during the examination. Appropriate grip is shown in (B). This grip allows smooth and easy transducer movements with good balance and also does not create undue strain during the examination. FIGURE 5.3 Sonograms demonstrating an example of the effect of increasing transducer pressure on the image. The image in (A) is performed with relatively minimal transducer pressure. Note the appearance of the veins (yellow arrows). In (B), the transducer pressure is increased. Note in that image, the transducer pressure has caused the veins to collapse and are no longer evident. In addition, the subcutaneous tissue at the top of the image is thinner than the image in (A). The examiner should always be vigilant about excessive pressure with the transducer, which can affect the appearance. Plenty of conduction gel should be used for good contact and a clear image (Figure 3.20). Scanning is often performed with sweeping motions to visualize the area intended. In many circumstances, scanning more rapidly helps to distinguish different types of tissue and can improve conspicuity relative to the image created when scanning very slowly. Using back and forth scanning often will facilitate appreciation of different types of echotexture such as fascicular pattern of nerves compared to the fibrillar pattern of tendons. The examiner should be comfortable using techniques to minimize anisotropic artifact. This includes changing the direction of the transducer beam to a more orthogonal (perpendicular) orientation of the tissue of interest when the angle of incidence is too small. Changing the direction of the beam by altering the angle without moving the base is called toggling the transducer (Figure 5.4). A heel-to-toe maneuver is used to improve the conspicuity of a curved structure in long axis (Figure 5.5). It is particularly effective in the circumstance of tendons in long axis that have a portion curved out of perpendicular orientation to the transducer (Figure 5.6). FIGURE 5.4 Pictures demonstrating toggling of the transducer to change the angle of incidence of the sound waves on the tissue. Note that the position angle of the transducer is changed from (A) to (B). This maneuver is used to reduce anisotropic artifact. The angle is changed without moving the base to a different position. Simultaneously moving the base while toggling should generally be avoided to prevent a confusing change of too many components of the image. FIGURE 5.5 Pictures demonstrating the heel-to-toe rocking of the transducer to change the angle of incidence of the sound waves on the tissue. Note that the position of the transducer is changed from (A) to (B). This maneuver is used to reduce anisotropic artifact of tissue in long axis. With heel-to-toe rocking, the angle is changed without sliding the base to a different position. FIGURE 5.6 Sonograms demonstrating the effect of the heel-to-toe rocking maneuver on the appearance of the long-axis view of the Achilles tendon insertion at the calcaneus (yellow arrows). In (A), the incident sound waves have an increased angle of incidence with respect to the curved portion of the Achilles insertion. Note that the fibers appear hypoechoic (dark) in this location. In (B), the heel-to-toe rocking changes the beam to a more perpendicular orientation in relation to that area, reducing the hypoechoic anisotropic artifact. This maneuver helps distinguish this anisotropic artifact from pathologic change in the tendon fibers, which would persist in hypoechoic appearance despite the orientation change. Attention to body position for both the examiner and the patient can improve the efficiency of the evaluation and minimize undue strain. The patient should be placed in a position that provides easy access with the transducer and allows comfortable arm position. Having to reach excessively can lead to fatigue and overuse syndromes (Figure 5.7). The patient should be generally placed between the examiner and the screen allowing visualization of both. This is important for both diagnostic evaluations as well as therapeutic injections (Figure 5.8). The machine should also be close enough to allow easy access to the controls without excessive moving. Attention to these details can make the scanning experience much easier for both the examiner and patient. FIGURE 5.7 Pictures demonstrating poor (A) and good (B) positioning for performing an ultrasound evaluation. In the poor positioning (A), the examiner has to reach for the patient as well as the machine. This creates an inefficient examination with undue muscle strain and fatigue. The area being examined is not in line with the screen. In (B), note how both the patient and examiner are in comfortable positions. The examiner does not have to overextend to perform the scanning or reach the controls. The patient is relatively between the examiner and screen allowing the examiner to attend to both areas simultaneously. The patient is also able to see the screen during the examination, which can facilitate live demonstration and explanation of the findings. FIGURE 5.8 Pictures demonstrating poor (A) and good (B) positioning for performing an ultrasound-guided injection. In the poor positioning (A), the patient is in a position that is out of line with the screen. This results in the need to look away from the patient to see the screen and also difficult positioning. In (B), note how the patient is in between the practitioner performing the procedure and the machine. This facilitates visualization of both areas and easy access to the injection field and the controls of the machine. 1) Avoid excessive grip and pressure with the transducer and hold it at its base. 2) Keep contact with the patient with the hand holding the transducer while scanning. 3) Learn the technique of toggling and heal-to-toe rocking with the transducer to reduce anisotropic artifact. 4) Use good ergonomics to provide a comfortable position for both the examiner and patient to improve ease of scanning.
Scanning Techniques and Ergonomics
INTRODUCTION
USE OF THE TRANSDUCER
ERGONOMICS

REMEMBER
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree