Chapter 18 Sedation and monitoring
Sedation
Sedation is the use of a drug or drugs to produce a state of depression of the central nervous system that enables interventional procedures or treatment to be carried out. Over recent years the complexity and number of interventional procedures in radiology departments has increased; often these patients are frail or medically unfit for surgery. Sedation is only part of a ‘package’ of care comprising pre-assessment, properly informed consent, adequate facilities, good techniques and risk avoidance.1
Sedative drugs may be combined with drugs used for pain relief (analgesia). Some drugs, such as benzodiazepines, have purely sedative effects but others, such as opioids, have combined sedative and analgesic effects. Although sedative and analgesic agents are generally safe, catastrophic complications related to their use can occur, often as a result of incorrect drug administration or inadequate patient monitoring.2 The incidence of adverse outcomes is reduced by improved understanding of the pharmacology of drugs used, appropriate monitoring of sedated patients and by recognizing those at increased risk of adverse event.
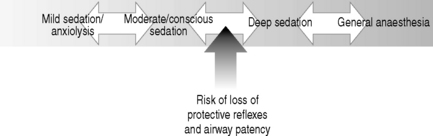
There is a continuum between the main types of sedation (see Fig. 18.1) defined as:
The joint Royal College of Radiologists/Royal College of Anaesthetists Working Party on Sedation and Anaesthesia in Radiology3 recommended establishment of local guidelines for sedation in radiology. These should include:
Preparation
Sympathetic patient management with an explanation of the procedure may reduce anxiety and remove the need for any medication. Sedation should be explained and consent obtained. Patients who are to be given intravenous (i.v.) sedation should undergo a period of fasting before the procedure; 6 h fasting for solid food and 2 h for clear liquids.
Resuscitation and monitoring equipment and oxygen delivery devices should be checked and venous access established.
DRUGS
As part of a sedation protocol the following may be used:
Analgesic drugs
Analgesic drugs are used for pain control and improve patient comfort. For some procedures local anaesthesia or oral analgesia (using paracetamol 1 g or ibuprofen 400 mg taken 1–2 h before the procedure) will be appropriate. For more invasive interventional radiology procedures the use of intravenous analgesia may be required.
LOCAL ANAESTHESIA
For recommended doses see Table 18.1.
Table 18.1 Recommended doses of local anaesthetic drugs
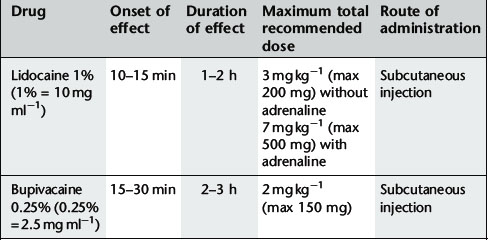
Commonly used local anaesthetics for subcutaneous infiltration are:
INHALATIONAL ANALGESIA
A mixture of 50% nitrous oxide and 50% oxygen (Entonox®) may be used. This has both analgesic and sedative properties.
INTRAVENOUS ANALGESIA
These drugs are used for pain control but also have a dose-dependant sedative effect. Most commonly used are the opioid drugs morphine, pethidine and fentanyl. These drugs must be given in small, divided doses and dose titrated to the patient’s need. It is extremely important to titrate the dosage to effect rather than assume a fixed dose based on body weight. The maximum recommended dose must not be exceeded because of the risk of adverse events, particularly respiratory depression. For recommended dosage see Table 18.2.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree