KEY FACTS
Terminology
- •
Synonyms: Pancreatic serous cystic neoplasm, microcystic adenoma of pancreas
Imaging
- •
Commonly in body and tail; 30% in pancreatic head
- •
Variable size; mean: 4.9 cm
- •
Well-demarcated, lobulated, heterogeneous mass with posterior acoustic enhancement
- •
Microcystic type: “Honeycomb” cystic mass with septa and solid-appearing component
- ○
Cluster of > 6 cysts; each typically < 1 cm
- ○
Central echogenic scar (30%); ± calcification
- ○
Solid, echogenic appearance due to interfaces between microcysts
- ○
- •
Macrocystic type: Unilocular or fewer larger cysts (> 2 cm)
- •
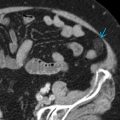
CT: Better characterization of classic honeycomb pattern
- ○
Cluster of > 6 cysts; each typically < 1-2 cm
- ○
Coalescing enhancing septa → central scar ± calcification
- ○
May mimic solid mass
- ○
- •
MR: Can better identify T2-hyperintense cysts separated by T2-hypointense septa
- •
Endoscopic ultrasound: May allow for presumptive diagnosis based on typical features
- ○
Higher spatial resolution than transabdominal ultrasound → often diagnostic for microcystic form
- ○
Can be used to guide fine-needle aspiration of cyst fluid for indeterminate cases e.g., macrocystic variant
- ○
- •
Pancreatic and common bile duct dilatation not typical
- •
Increased vascularity within septa
Top Differential Diagnoses
- •
Pancreatic pseudocyst
- •
Mucinous cystadenoma of pancreas
- •
Intraductal papillary mucinous neoplasm
- •
Cystic neuroendocrine tumor
- •
Ductal pancreatic carcinoma
- •
Solid pseudopapillary neoplasm
Pathology
- •
Cysts lined by small cuboidal epithelial cells with clear cytoplasm and minimal mucin
- •
Subtypes: Microcystic and oligocystic/macrocystic
- ○
WHO classification
- –
Serous microcystic adenoma: Sponge-like/honeycomb or polycystic mass with central scar
- –
Serous oligocystic adenoma/macrocystic variant: Unilocular or with few large cysts (less common)
- –
- ○
- •
Benign epithelial neoplasm arising from centroacinar cells of exocrine pancreas and composed of small cysts containing proteinaceous fluid separated by fibrovascular connective tissue septa
- •
May be multiple in von Hippel-Lindau disease
Clinical Issues
- •
20% of all cystic pancreatic lesions; 1% of pancreatic neoplasms
- •
Middle and elderly age group; mean: 61.5 years, M:F = 1:4
- •
Typically asymptomatic or vague epigastric pain; may present with nausea, vomiting, weight loss, palpable mass, jaundice
- •
Typically benign and slow growing
- •
Nearly no malignant potential
- •
Very rare tumors may behave aggressively or become symptomatic (large lesions or lesions in head)
- •
Asymptomatic and small tumors: Imaging surveillance at 6- to 12-month intervals until stability demonstrated over 2-year period
- •
Symptomatic and large tumors → complete surgical excision
Scanning Tips
- •
Depending on body habitus, consider higher frequency transducers to depict characteristic cluster of small cysts within mass