How to Image the Shoulder
See the shoulder protocols at the end of the chapter.
- •
Coils and patient position: A surface coil is required to obtain high-resolution, detailed images. The patient is positioned supine with the arm at the side in neutral position or slight external rotation for a standard examination. The arm position influences how well different structures can be identified on MRI. ,
- •
Image orientation ( Box 10-1 ): A small field of view (12 cm) and 3- to 4-mm-thick slices are obtained in three imaging planes: (1) coronal oblique, (2) axial, and (3) sagittal oblique. The coronal oblique images are acquired with cuts made parallel to the supraspinatus tendon, which is seen on an axial cut through the superior portion of the shoulder; alternatively, they may be acquired in a plane perpendicular to the articular surface of the glenoid, as seen on axial images. The axial images are obtained from the top of the acromion to the bottom of the glenohumeral joint using a coronal scout image as a localizer. The sagittal oblique images are acquired with cuts parallel to the articular surface of the glenoid as seen on axial images, from the scapular neck through the lateral margin of the humerus.
BOX 10-1
Shoulder Structures to Evaluate in Different Planes
Coronal Oblique
Infraspinatus muscle and tendon: Longitudinally
Supraspinatus muscle and tendon: Longitudinally
Acromioclavicular joint
Acromion
Glenohumeral joint
Subacromial/subdeltoid bursa
Labrum (superior and inferior portions)
Sagittal Oblique
Supraspinatus muscle and tendon: In cross section
Infraspinatus muscle and tendon: In cross section
Teres minor muscle and tendon: In cross section
Long head of biceps tendon (proximal portion): In cross section
Subscapularis muscle and tendon: In cross section
Rotator interval
Acromion
Coracoacromial ligament
Coracoacromial arch
Glenohumeral ligaments
Axial
Long head of biceps tendon: In cross section through bicipital groove
Subscapularis muscle and tendon: Longitudinally
Labrum (anterior and posterior portions)
Capsule
Glenohumeral joint
Glenohumeral ligaments
- •
Pulse sequences and regions of interest: Several different pulse sequences are used for the evaluation of internal derangements of the shoulder joint. They depend on whether the shoulder is imaged with or without intra-articular gadolinium. The pulse sequences we use for standard shoulder MRI are (1) sagittal oblique T1W and FSE T2 with fat suppression, (2) coronal oblique FSE T2 with fat suppression, and (3) axial FSE T2 with fat suppression and FSE proton density with fat suppression. The T1W sagittal oblique is used to assess the size of the cuff muscles and to look for fatty infiltration of the muscles. The FSE T2 sagittal oblique is used to look for muscle edema and fluid in the various bursae around the shoulder. The rotator cuff insertion onto the greater tuberosity also is nicely displayed, and partial-thickness or full-thickness cuff tears can be readily identified. The oblique coronal FSE T2 sequence confirms the cuff tears in the supraspinatus or infraspinatus tendons seen on the sagittal images. It also shows the superior labrum. The axial images show the anterior and posterior labrum, the long head of the biceps tendon, and the subscapularis tendon and muscle. The FSE T2 sequence seems to show the labrum better when there is a joint effusion, whereas the FSE proton density (or gradient echo) sequence shows the labrum better if there is no joint effusion. With gadolinium arthrography, we do three planes of T1W with fat suppression and oblique coronal and axial FSE T2 with fat suppression. We also do a non–fat-suppressed T1W oblique sagittal sequence.
- •
Contrast: We previously did standard shoulder MRI routinely without intra-articular gadolinium. We found ourselves struggling to be certain in many cases, and correlations with arthroscopic or surgical findings were suboptimal. For this reason, we now do shoulder MR arthrography whenever possible. As more and more of our referring physicians learn to look at their patients’ MRI studies, they realize, as we do, that pathology and normal anatomy are better visualized if fluid is distending the joint. Referring physicians soon begin ordering shoulder MRI studies with arthrography. Several of our orthopedic surgeons order 100% of their shoulder MRI studies with arthrograms. Shoulder MR arthrography is required in the evaluation of patients with instability. In our experience, it also is extremely useful in showing subtle and sometimes not so subtle full-thickness tears of the rotator cuff. Shoulder MR arthrography is performed after intra-articular injection of gadopentetate dimeglumine (gadolinium). The solution used for the arthrogram consists of 0.1 mL of gadolinium mixed with 20 mL of normal saline and 3 mL of iodinated contrast material. About 10 to 12 mL of the mixture is injected into the shoulder joint before MRI using fluoroscopic guidance and the same approach as for a conventional shoulder arthrogram.
Tendons and the Coracoacromial Arch
NORMAL ANATOMY
Tendons
The rotator cuff typically is considered to be composed of four tendons:
- 1.
Supraspinatus
- 2.
Infraspinatus
- 3.
Teres minor
- 4.
Subscapularis
The rotator cuff is a laminated structure formed by the joint capsule and the ligaments in addition to the four tendons listed. The four tendons of the rotator cuff have cylindrical and flat portions that fan out and interdigitate with each other to form a continuous tendinous hood at their insertions onto the tuberosities of the humerus. There are no synovial tendon sheaths or surrounding paratenon investing the rotator cuff tendons. The coracohumeral ligament extends from the coracoid process to insert onto the lesser and greater tuberosities and the intervening transverse humeral ligament on the humerus. The coracohumeral ligament is located superficial to the joint capsule and the supraspinatus and infraspinatus tendons. These structures constitute the multiple layers of the rotator cuff.
The supraspinatus tendon runs between the undersurface of the acromion and the top of the humeral head. It inserts into fibrocartilage (not hyaline cartilage) on top of the greater tuberosity of the humerus. Located posteriorly on the greater tuberosity, from a superior to an inferior position, are the infraspinatus and the teres minor tendons; running anterior to the shoulder joint is the subscapularis tendon, which attaches to the lesser tuberosity. The supraspinatus muscle acts with the deltoid muscle to abduct the arm. The infraspinatus muscle and the teres minor muscle externally rotate the humerus, and contraction of the subscapularis muscle results in internal rotation of the humerus.
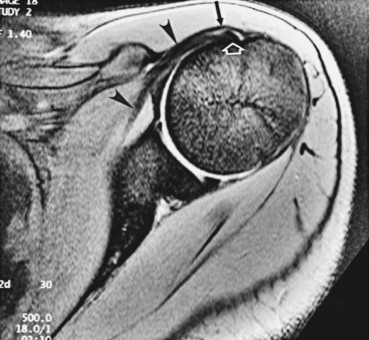
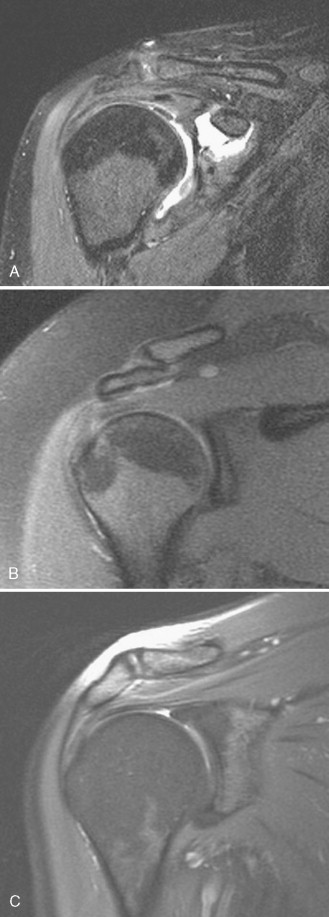
The entire length of two of the rotator cuff tendons, the supraspinatus and infraspinatus, can be seen well in the coronal oblique plane. Posterior to the humeral head, the infraspinatus tendon can be seen coursing obliquely in a craniocaudal direction at about a 45-degree angle to attach to the posterior portion of the greater tuberosity ( Fig. 10-1 ). On more anterior slices, the horizontally oriented supraspinatus muscle and tendon are always seen on the same cuts that best show the acromioclavicular joint. The musculotendinous junction of the supraspinatus normally is located just lateral to the acromioclavicular joint ( Fig. 10-2 ). The supraspinatus runs at an angle of approximately 45 degrees relative to the coronal plane.


Other tendons that also can be evaluated well on coronal oblique images are the deltoid tendon slips that attach to the superior and inferior margins of the acromion ( Fig. 10-3 ) and portions of the long head of the biceps tendon. The coracoacromial ligament is another low signal intensity structure that inserts on the lateral and inferior aspect of the acromion, appearing similar to the deltoid tendon attachment. The long head of the biceps tendon can be seen on far anterior cuts through the shoulder, from its origin at the superior labrum (the so-called biceps anchor) ( Fig. 10-4A ), and inferiorly in the bicipital groove. We have found that with internal rotation of the humerus, which is the position most patients assume, the bicipital groove is a good anatomic landmark to key on for inspecting the leading edge of the supraspinatus. The supraspinatus tendon inserts just lateral to the bicipital groove, and commonly tears begin or are isolated at this location and are frequently overlooked (see Fig. 10-4B ).

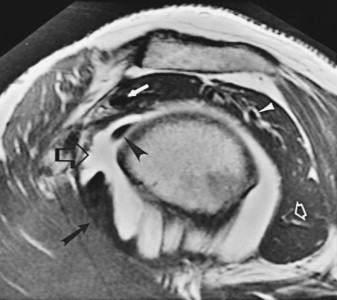
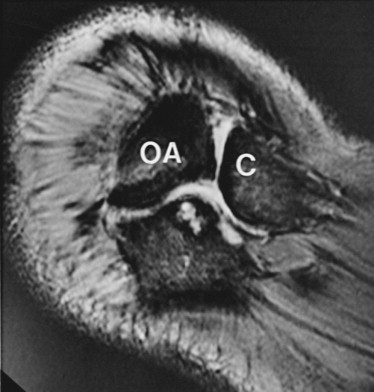
The subscapularis muscle runs anterior to the shoulder, and its tendon attaches to the lesser tuberosity. The length of the subscapularis tendon and muscle can be shown best on axial images ( Fig. 10-5 ). Its attachment blends with the transverse humeral ligament, which bridges the lesser and greater tuberosities and holds the long head of the biceps tendon in the bicipital groove.
The portion of the long head of the biceps tendon that is located within the bicipital groove is cut transversely on axial images and is a round or oval structure. In some cases, it blends with the low signal intensity cortex of the humerus and may be difficult to identify. A small amount of fluid is seen in the dependent side of the long head of the biceps tendon sheath normally; with a shoulder joint effusion, fluid may encircle the biceps tendon because the tendon sheath is in direct communication with the shoulder joint. One or two rounded fluid collections may be seen lateral to the biceps tendon, which represent the anterolateral branch of the anterior circumflex artery and vein ( Fig. 10-6 ).

On sagittal oblique images, the tendons of the supraspinatus, infraspinatus, teres minor, and most proximal portion of the long head of the biceps, and the multiple tendon slips of the subscapularis all are imaged in cross section, surrounded by their associated muscles ( Fig. 10-7 ). This plane of imaging is valuable for confirming the status of tendons when abnormalities are seen or suspected in the other planes of imaging, where the tendons are viewed longitudinally. The space between the supraspinatus tendon and the subscapularis tendon, which also is seen well on sagittal oblique images, is known as the rotator interval.
Tendons are normally low signal intensity on all pulse sequences; however, increased signal intensity in normal tendons may be caused by the magic angle phenomenon. , The magic angle phenomenon occurs when collagen fibers are oriented at about 55 degrees to the constant magnetic induction field. This orientation results in an intermediate signal intensity within the otherwise low signal intensity tendon on TE sequences such as T1W, proton density, and gradient echo (T2*) images. In the shoulder, this phenomenon occurs commonly about 1 cm proximal to the insertion of the supraspinatus tendon on the greater tuberosity, which is the hypovascular region of the tendon, also known as the critical zone. ,
The intermediate signal intensity from the magic angle phenomenon disappears with long TE sequences, such as T2W images, making it possible to differentiate magic angle from an abnormal tendon. A good rule to distinguish the magic angle phenomenon from a tear on T2 * images is that the signal intensity within the tendon is never higher than the signal intensity within the adjacent muscle if it is from the magic angle phenomenon (see Fig. 10-2 ), whereas with a tendon tear, the signal intensity is higher than that of muscle. Other potential causes of increased signal intensity in a normal supraspinatus tendon besides the magic angle phenomenon include the presence of connective tissue between tendon fascicles, partial volume averaging effect, and overlap of the supraspinatus and infraspinatus tendons from imaging with the arm in internal rotation ( Box 10-2 ).
- •
Magic angle (short TE sequences only)
- •
Overlap of supraspinatus and infraspinatus tendons (internal rotation)
- •
Connective tissue between tendon fibers
- •
Partial volume averaging
- •
Tendon degeneration
- •
Tendon tears (high signal on long TE sequences)
Coracoacromial Arch
The coracoacromial arch is formed by the humeral head posteriorly, the acromion superiorly, and the coracoid process and the intervening coracoacromial ligament anteriorly. Located within the coracoacromial arch, from superior to inferior, are the subacromial/subdeltoid bursa, the supraspinatus tendon and muscle, and the long head of the biceps tendon. The coracoacromial ligament restricts anterior and superior motion of the humeral head and overlying tendons ( Fig. 10-8 ; see Fig. 10-7 ). Anything that decreases the space within the coracoacromial arch could lead to symptoms of impingement. Structures that form or are contained by the coracoacromial arch must be evaluated carefully in the different planes of imaging.
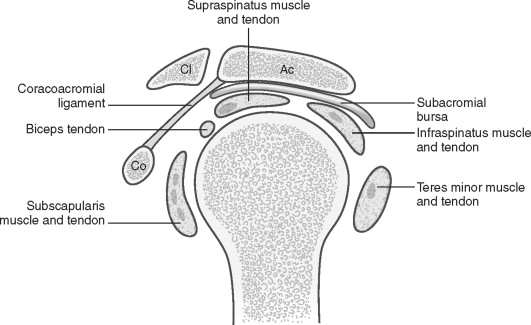
On sagittal oblique images, the coracoacromial ligament is seen as a taut, thin band with parallel margins. Typical of all ligaments, it has low signal intensity on all pulse sequences ( Fig. 10-9 ).

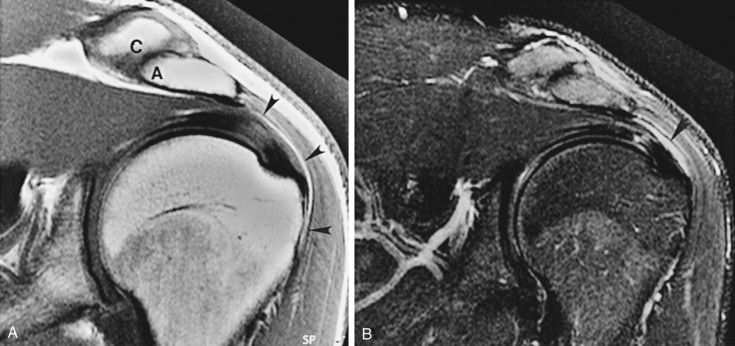
The configuration and the orientation of the acromion are evaluated in the coronal and the sagittal oblique planes. Normally, the anterior and the most posterior aspects of the inferior black cortical line of the acromion on a sagittal oblique view should be nearly horizontal or else curved, paralleling the humeral head (see Fig. 10-9 ). On coronal oblique images, the anterior aspect of the acromion should be horizontal and at the same level as the clavicle ( Fig. 10-10 ). The normal acromioclavicular joint has a smooth undersurface, with both bones running in a smooth horizontal plane. Similarly, the undersurface of the acromion should be smooth and without spurs.

A boomerang-shaped fat plane surrounding the subacromial/subdeltoid bursa is evident between the acromioclavicular joint and the underlying supraspinatus tendon and muscle on coronal oblique images ( Fig. 10-11 ). The subacromial/subdeltoid bursa normally is evident only because it is outlined by fat. The bursa should have no fluid, or only a small wisp of fluid; it should not be distended with fluid. Another fat plane that is separate from that of the subacromial/subdeltoid bursa normally is evident, separating the supraspinatus muscle and tendon from the undersurfaces of the overlying acromion and acromioclavicular joint (see Fig. 10-10 ).
SHOULDER IMPINGEMENT
In 1972, Neer, an orthopedic surgeon, proposed the concept that tears of the supraspinatus tendon are related to impingement on the tendon by the structures that form the coracoacromial arch. Any condition that limits the space within the coracoacromial arch can produce impingement on the subacromial bursa, the supraspinatus tendon, and the long head of the biceps tendon. Neer proposed surgical decompression to treat this impingement syndrome, consisting of an anteroinferior acromioplasty and resection of the coracoacromial ligament, decompressing and creating more room for the supraspinatus tendon and other affected structures. Abnormalities from impingement that affect the supraspinatus tendon and surrounding structures range from edema to full-thickness tendon tears. All of these abnormalities are associated with symptoms of pain and collectively are referred to as the impingement syndrome . The syndrome is characterized clinically by acute or chronic shoulder pain induced by movements of abduction and external rotation or by elevation and internal rotation of the shoulder. It can occur in young athletes involved with repetitive movements of elevation and abduction of the shoulder, or in elderly individuals from degenerative changes of the acromioclavicular joint and formation of subacromial spurs. Generally, impingement is more common with increasing age ( Box 10-3 ).
Symptoms
- •
Pain
- •
Abduction and external rotation
- •
Elevation and internal rotation
- •
Causes (Anything Decreasing Size of Coracoacromial Arch)
- •
Acromial shape
- •
Type III: Inferiorly projecting hook (sagittal oblique)
- •
- •
Acromial orientation
- •
Anterior down-sloping (sagittal oblique)
- •
Inferolateral tilt (coronal oblique)
- •
Low-lying (coronal oblique)
- •
- •
Acromioclavicular degenerative joint disease
- •
Os acromiale
- •
Thick coracoacromial ligament
- •
Post-traumatic osseous deformity
- •
Instability
- •
Muscle overdevelopment
Potential Consequences
Tendons
- •
Supraspinatus tendon
- •
Degeneration, partial tear, complete tear
- •
- •
Proximal long head, biceps brachii tendon
- •
Degeneration, partial tear, complete tear
- •
Bones
- •
Degenerative cysts, sclerosis of greater tuberosity or humeral head or both
Bursa
- •
Subacromial/subdeltoid bursitis
Causes
The supraspinatus tendon is reportedly predisposed to impingement from several sources that can be identified with MRI , :
- 1.
Abnormal configuration of the anterior acromion
- 2.
Anterior downsloping of the acromion
- 3.
Low-lying acromion
- 4.
Inferolateral tilt of the acromion
- 5.
Os acromiale
- 6.
Acromioclavicular degenerative joint disease
- 7.
Thickening of the coracoacromial ligament
- 8.
Post-traumatic osseous deformity
- 9.
Instability
- 10.
Muscle overdevelopment
Several of these believed causes have been discredited and are not considered to be predisposing factors for cuff pathology. They are discussed individually.
Acromial Configuration.
Bigliani and colleagues described three predominant shapes of the acromion based on scapular Y view radiographs of the shoulder and believed the shape was an important factor contributing to impingement. A type I acromion has a flat undersurface. Type II acromion has a concave undersurface with the inferior acromial cortex parallel to the cortex of the underlying humeral head. Type III acromion has an inferiorly projecting anterior hook that narrows the space between the acromion and the humerus. It was thought that type II and III acromions had an increased incidence of cuff pathology, but this has not borne out in practice. Our surgeons do not inquire about the shape of the acromion, and acromion type is no longer considered to be an important factor relating to cuff pathology.
Acromial Slope.
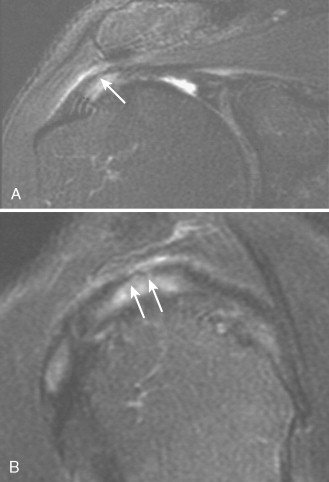
The slope of the acromion can be evaluated on sagittal and coronal oblique images. Normally, the lateral aspect of the acromion is oriented nearly horizontal or slopes downward posteriorly on sagittal oblique images. An anteriorly downsloping acromion occurs when the inferior cortex of the anterior acromion is located more caudally than the inferior cortex of the posterior aspect of the acromion ( Fig. 10-12 ). Another abnormal slope to the acromion consists of an inferolateral tilt, which can be detected on coronal oblique images. An inferolateral tilt or slope occurs when the most lateral portion of the acromion is tilted inferiorly relative to the clavicle ( Fig. 10-13 ). Sloping of the acromion in either direction increases the risk for impingement from mechanical trauma to the underlying distal supraspinatus tendon ( Fig. 10-14 ).


Acromial Position.
Normally, the inferior cortex of the acromion is in line with the inferior cortex of the clavicle on coronal oblique views. A low-lying acromion exists when its inferior cortex is positioned below the inferior cortex of the clavicle (see Fig. 10-11 ). This positioning causes narrowing of the acromiohumeral space, which may predispose to impingement.
Os Acromiale.
Os acromiale is an accessory ossification center of the acromion that is normally fused by 25 years of age. An unfused os acromiale after this age may be seen in 15% of the population; its presence is associated with an increased incidence of impingement and rotator cuff tears, presumably because the os is mobile and decreases the space in the coracoacromial arch with motion. The os acromiale is best identified on axial images, although it can be seen in all imaging planes ( Fig. 10-15 ).
Acromioclavicular Joint Degenerative Changes.
Degenerative joint disease of the acromioclavicular joint may manifest as inferiorly projecting osteophytes, fibrous overgrowth of the capsule, or both ( Fig. 10-16 ). , On radiographs, osteophytes are underestimated, and fibrous overgrowth is not depicted at all; MRI directly shows the presence, severity, and extent of these structures that may cause impingement. Obliteration of the fat between the supraspinatus muscle or tendon and the overlying acromioclavicular joint and indentation of the supraspinatus tendon or muscle by abnormalities of the acromioclavicular joint are indications that the degenerative changes are considerable and may contribute to impingement.
Coracoacromial Ligament.
Focal thickening of the coracoacromial ligament may be observed on sagittal oblique MRI, but has never been shown to be related to impingement. Evaluation of the coracoacromial ligament is not part of our interpretation of shoulder MRI.
Post-traumatic Deformity.
As a result of hypertrophic callus formation or malalignment of fracture fragments that involve the bones adjacent to the coracoacromial arch, there may be narrowing of the coracoacromial arch with resultant impingement, although this is uncommon.
Instability.
Glenohumeral degenerative changes can be caused by shoulder instability, and instability can be a contributing factor to impingement. Instability and impingement are two conditions that often coexist; this is discussed later in this chapter.
Muscle Overdevelopment.
Supraspinatus muscle enlargement, as seen in weightlifters, swimmers, and other athletes, may induce impingement even if the coracoacromial arch and acromiohumeral intervals are normal because the large muscle decreases the space available for the tendon to glide between the structures of the coracoacromial arch. A deformity (indentation) of the superior surface of the supraspinatus muscle caused by the acromioclavicular joint is the only abnormality seen with MRI.
Effects of Impingement ( Box 10-4 )
Tendons.
The supraspinatus tendon is affected far more commonly than other tendons in the shoulder. Impingement on the supraspinatus tendon from any source can cause tendon degeneration and partial-thickness or full-thickness tears. Conversely, the same tendon abnormalities may exist without evidence of structural or mechanical causes of impingement. Most partial-thickness tears of the supraspinatus tendon occur on the undersurface (articular) aspect of the tendon, rather than on the superior (bursal) surface where abnormalities in the coracoacromial arch would logically be expected to cause early partial tears. The proximal long head of the biceps tendon may be affected by impingement in the same ways as the supraspinatus tendon because of its similar location and course just beneath the supraspinatus tendon within the shoulder joint.
- •
Identification of mechanical causes
- •
Evaluation of tendon integrity
- •
Abnormal high signal intensity (degeneration/partial tears)
- •
Abnormal shape: Thin, thick, irregular (partial tears)
- •
Discontinuity (complete tears)
- •
- •
Subacromial/subdeltoid bursal fluid
- •
Glenohumeral degenerative joint disease
Degenerative Osseous Cysts.
Although the supraspinatus tendon is the structure most often affected by impingement, certain associated osseous findings are very common as well. Cortical hypertrophy, sclerosis, and small degenerative cysts in the greater tuberosity often are present and may precede MRI evidence of abnormalities within the tendons. The osseous degenerative changes have been found histologically to be associated with microtears of the adjacent tendon.
Subacromial/Subdeltoid Bursitis.
Irritation of the subacromial/subdeltoid bursa can occur from impingement. When this occurs, the bursa becomes distended with fluid and is painful (see Fig. 10-11 ). Normally, there is no fluid, or only a trace of detectable fluid, in this bursa. Bursal fluid is common in the presence of rotator cuff tears. Bursal fluid cannot be seen without a T2W sequence, so this sequence is needed even when an MR arthrogram is performed.
TENDON TEARS, DEGENERATION, AND DISLOCATION
Supraspinatus ( Box 10-5 )
Degeneration and Partial Tendon Tears.
Degeneration and partial tendon tears generally are indistinguishable from one another on T1W images, where they appear as focal or diffuse regions of intratendinous intermediate signal intensity, which is one of the reasons we no longer acquire T1W images in the coronal plane. If these areas maintain the same signal intensity as muscle on T2W images, they are most consistent with tendon degeneration; if these areas become high signal intensity, similar to fluid on T2W images, they represent partial tendon tears. It frequently is difficult to distinguish between degeneration or partial tendon tears, and in such a situation the general term tendinopathy may be used to describe the abnormalities. Tendon degeneration and partial tears often coexist.
Full-Thickness Tear
- •
Direct signs
- •
Tendon discontinuity
- •
Fluid signal in tendon gap
- •
Retraction of musculotendinous junction
- •
- •
Associated findings
- •
Subacromial/subdeltoid bursal fluid
- •
Muscle atrophy
- •
Partial-Thickness Tear
- •
Increased signal T1 and T2, joint or bursal surface
- •
Higher signal than muscle on T2 (similar to joint fluid)
- •
Degeneration
- •
Intrasubstance increased signal T1 and T2
- •
Not as high signal as joint fluid
- •
Magic angle phenomenon has similar signal characteristics as tendon partial tears or degeneration on short TE images. The findings, however, are focal instead of diffuse, are at a specific location (1 cm from the insertion of the supraspinatus tendon on the greater tuberosity) and, most importantly, disappear on long TE images. , In addition, the signal changes are not associated with thinning, thickening, or irregularity of the tendon.
A partial tear on the undersurface (joint surface) of the tendon fills with high signal intensity gadolinium solution on MR arthrograms ( Fig. 10-17 ). Partial-thickness tears on the upper (bursal) surface of the tendon need to be evaluated similar to regular shoulder MRI without arthrography because gadolinium cannot enter the tear in that location. Partial-thickness tears generally start on the undersurface of the distal end of the supraspinatus tendon; the inferior layers may retract medially, whereas the superior layers remain intact.
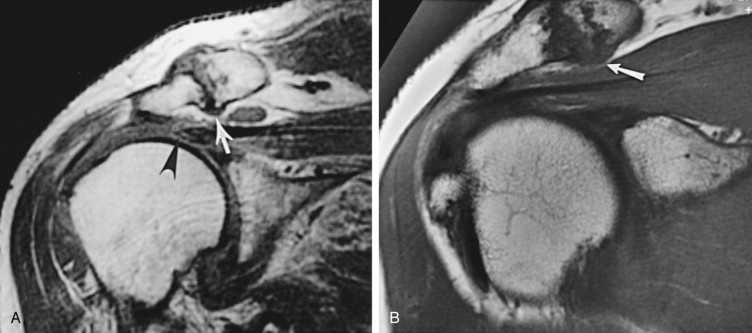
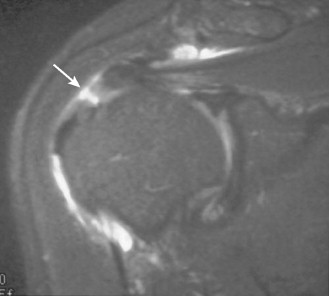
The most common partial tear, which is the most common cuff tear of all kinds, is one in which the insertional fibers of the cuff on the greater tuberosity are disrupted from the bone ( Fig. 10-18 ). This has been termed a rim rent tear. It was first described by an orthopedic surgeon, Codman, in 1934. It was found in about 10% of cases by Tuite and coworkers, but we believe it is seen more commonly in our practice. In a series of 200 consecutive shoulder MRI studies, we found 117 cuff tears, 70 (60%) of which were partial cuff tears. Only 2 of the 70 were bursal-sided tears. Bursal-sided tears are much less common than joint-sided tears. Of the 70 partial tears, 49 (42%) were rim rent tears.
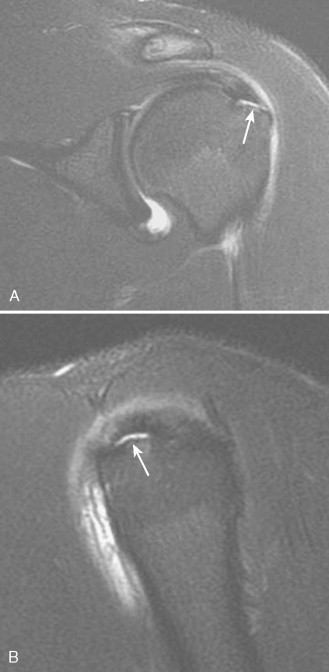
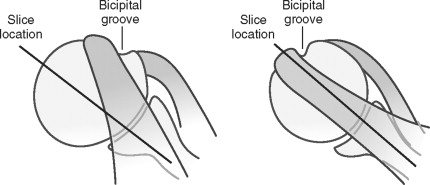
We had overlooked many of these tears on our original interpretations primarily because we did not appreciate the significance of internal rotation of the humerus. The anteriormost fibers of the supraspinatus tendon insert just lateral to the bicipital groove and can be overlooked easily on the oblique coronal images if the shoulder is internally rotated ( Fig. 10-19 ). If one finds the biceps on the most anterior coronal images, the more anterior fibers of the cuff can be seen just adjacent to the bicipital groove ( Fig. 10-20 ). When these fibers are disrupted, the tear can be seen as an interruption of the normal tissue adjacent to the bicipital groove ( Fig. 10-21 ). The tear can be confirmed on sagittal oblique images, but because the biceps is so close to the tear it is often difficult to tell if fluid in the cuff is from partial volume averaging with fluid in the bicipital groove (see Fig. 10-21C ).

We believe that the most common cuff tear is a partial-thickness tear at the insertion of the cuff fibers onto the greater tuberosity, many of which progress to a fullthickness tear. These tears can occur anteriorly on the greater tuberosity involving the supraspinatus, or posteriorly on the greater tuberosity involving the infraspinatus. These joint-sided or articular-sided tears are much more common than bursal-sided partial tears. Tears at the so-called critical zone, 1 to 1.5 cm proximal to the tendon insertion, are not as common as previously believed.
Detection of tendon abnormalities before the development of a full-thickness tear is important because the process may be arrested with conservative therapy, débridement, and decompression surgery. A full-thickness tear, in addition to pain, results in limited active movements of abduction and requires more involved surgery than that performed for a partial tear. MRI is reportedly less sensitive for detecting partial-thickness tears of the supraspinatus tendon than full-thickness tears. The specificity is in the range of 90%, but the sensitivity of standard MRI for detecting partial-thickness tears is reported to be 35% to 90%; these figures are significantly improved with MR arthrography.
Full-Thickness Tears.
Direct evidence of a full-thickness tear by conventional MRI (not MR arthrography) consists of discontinuity of the tendon with high signal intensity fluid traversing the gap between the tendon fragments from the articular to the bursal surfaces of the tendon on T2W sequences ( Fig. 10-22 ). MR arthrography shows high signal gadolinium on T1W images in the glenohumeral joint and in the subacromial/subdeltoid bursa with discontinuity of the tendon and gadolinium filling the gap between disrupted tendon fragments ( Fig. 10-23 ). MRI also can show the size of the tear, the degree of retraction of fragments, the quality of the remaining tendon fragments, and if there is associated muscle atrophy or osseous abnormalities; these features should be commented on in the report. Muscle atrophy is seen as high signal intensity within the muscle on T1W images ( Fig. 10-24 ), whether in the sagittal or the coronal plane.

A supraspinatus tendon tear usually is located distally in the supraspinatus tendon, either near its attachment to the greater tuberosity or in the critical zone of the tendon located about 1 cm proximal to its insertion. Tears usually start in the anterior portion of the distal supraspinatus tendon as rim rent tears and propagate posteriorly. Complete disruption of fibers in the craniocaudal direction with communication between the joint and bursa indicates a full-thickness tear, even if it has not separated the tendons completely in the anteroposterior direction.
Disruption of the supraspinatus tendon is not always clearly evident or easy to diagnose by standard MRI. Granulation tissue or debris may obscure the tear, the tear may be very small, or it may be located far anteriorly, all of which make the diagnosis much more difficult. These difficulties can be alleviated with MR arthrography, which provides much more information (see Fig. 10-23 ). It is unusual, however, for us to see gadolinium in the subacromialsubdeltoid bursa without seeing a gap in the tendon. One could propose not using gadolinium in the arthrogram solution—only injecting saline for joint distention. We think this is a reasonable approach; it would shorten imaging time considerably and decrease cost, but this hypothesis needs to be tested because the current standard of care for MR shoulder arthrography entails gadolinium.
The sensitivity and specificity for full-thickness rotator cuff tears by MRI are greater than 90%. MR arthrography improves these figures and increases the confidence with which the diagnoses are made. The ability of MRI to show complete tears of the rotator cuff tendons is significantly better than its ability to show partial-thickness tears.
Long Head of the Biceps ( Box 10-6 )
Tears.
The long head of the biceps tendon is completely torn in about 7% of patients with supraspinatus tendon tears and is abnormal (degeneration or partial tears) in about one third. Its proximity to the supraspinatus tendon makes it vulnerable to forces of impingement identical to forces affecting the supraspinatus tendon. Long head of the biceps tendon tears associated with supraspinatus tendon tears involve the impingement zone just proximal to the bicipital groove, and usually occur in older individuals. The distal tendon fragment and the muscle may retract distally, and an empty bicipital groove may be shown on axial MRIs of the shoulder ( Fig. 10-25 ). Acute tears of the long head of the biceps tendon may occur with severe trauma in young individuals or in older weekend athletes. Acute tears unrelated to impingement generally occur distally in the tendon, near the musculotendinous junction.
Tears/Degeneration
- •
Attachment to superior labrum
- •
Associated with SLAP lesions
- •
- •
Proximal to bicipital groove
- •
Associated with impingement
- •
Older population
- •
- •
Musculotendinous junction
- •
Acute, traumatic injuries
- •
Younger population
- •
Dislocation
- •
Associated disruptions
- •
Transverse humeral ligament
- •
Usually subscapularis tendon
- •
- •
MRI
- •
Empty bicipital groove (axial)
- •
Tendon displaced medially, either anterior to or within the glenohumeral joint
- •
Biceps tendon may be anterior to, posterior to, or within a torn subscapularis tendon
- •
Subscapularis tendon avulsed from tuberosity (or may be intact)
- •
Dislocation.
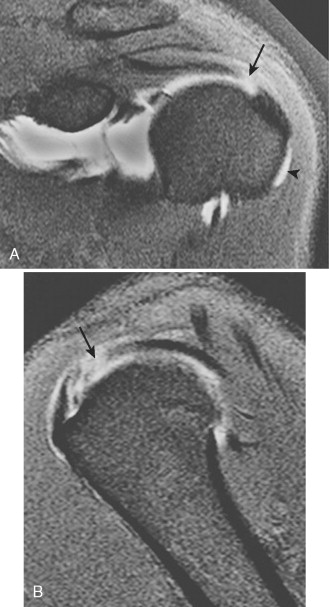
Other abnormalities of the long head of the biceps tendon may occur, unassociated with impingement. Acute trauma can cause avulsion, subluxation, and dislocation of the tendon, all of which need to be repaired surgically. For subluxation or dislocation to exist, there must be disruption of the transverse humeral ligament that normally bridges the lesser and greater tuberosities and holds the long head of the biceps tendon in place. Usually, a tear of the subscapularis tendon also coexists. With dislocation, the long head of the biceps tendon may displace anteromedially, which may or may not be associated with an intact subscapularis tendon. It may dislocate medially within the shoulder joint, which is always associated with a tear of the subscapularis tendon at its attachment to the lesser tuberosity. , Biceps tendon subluxation and dislocation are shown best on axial MRIs, where the bicipital groove is empty, and the low signal round tendon is seen at variable distances medial to the groove, either deep or superficial to the subscapularis tendon ( Fig. 10-26 ).

Infraspinatus
Infraspinatus tendon tears can be seen in isolation after acute trauma (although this is rare), can occur in association with massive tears of the supraspinatus tendon, or can be associated with posterosuperior impingement of the shoulder ( Fig. 10-27 ). We have found isolated rim rent tears to be common ; however, because isolated full-thickness tears of the infraspinatus are rare, the rim rent tears must not progress to full-thickness tears as often as in the supraspinatus.
Posterosuperior Impingement ( Box 10-7 ).
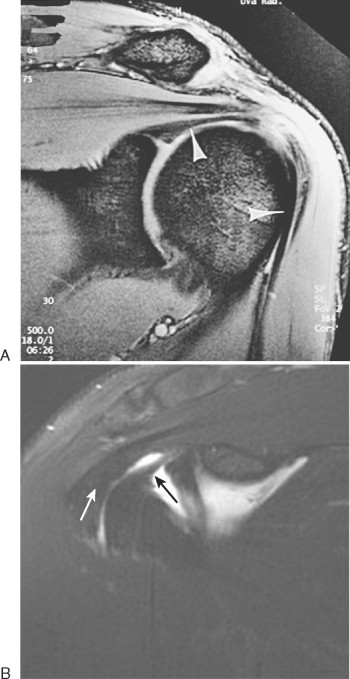
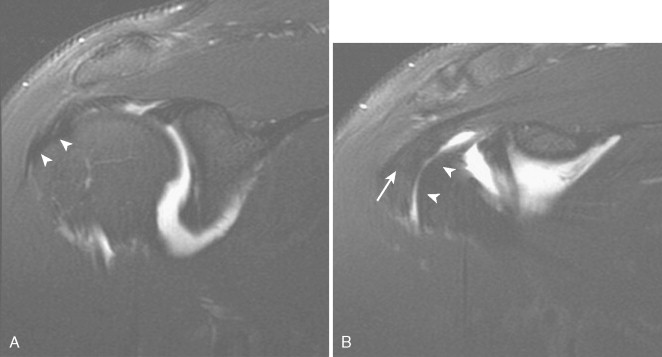
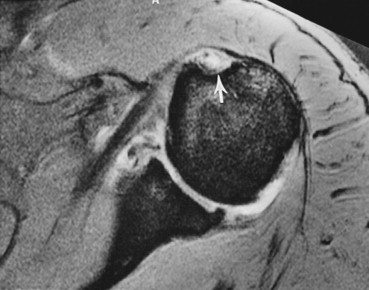
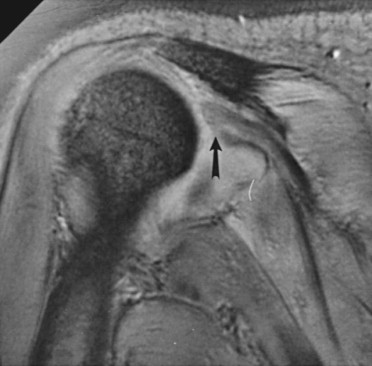
Posterosuperior impingement refers to impingement of the supraspinatus tendon, and mainly of the infraspinatus tendon, between the humeral head and the posterior glenoid rim during overhead movements with abduction and external rotation, such as pitching. , Posterosuperior impingement results in abnormalities affecting the rotator cuff, most commonly the infraspinatus tendon, the posterosuperior labrum, and the humeral head at the point of impaction with the posterosuperior glenoid. Patients present with posterior shoulder pain and may have associated anterior shoulder instability. MRI findings include degenerative cysts on the posterior aspect of the humeral head near the insertion of the infraspinatus tendon; fraying, partial, or complete tears of the infraspinatus tendon or supraspinatus tendon; and fraying or tears of the posterior glenoid labrum ( Fig. 10-28 ).
Clinical
- •
Impingement of infraspinatus and supraspinatus tendons between humeral head and posterosuperior labrum
- •
Occurs in late cocking phase of pitching
- •
Occurs with maximum abduction and external rotation
- •
Posterosuperior pain and anterior instability
MRI
- •
Humeral cysts adjacent to infraspinatus tendon insertion
- •
Infraspinatus (and supraspinatus) tendon undersurface tears
- •
Posterosuperior labral tear
Subscapularis ( Box 10-8 )
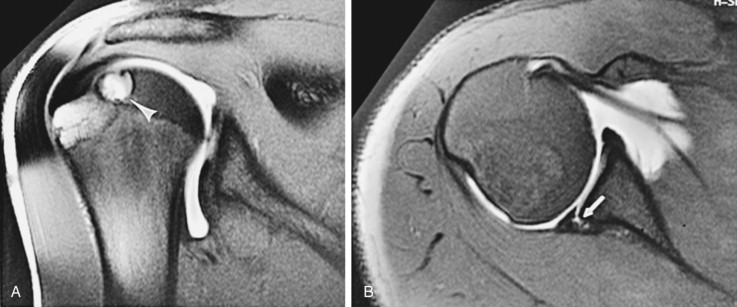
Subscapularis tendon tears are common. They can result from acute trauma on an adducted arm in hyperextension or in external rotation. They can result from an anterior shoulder dislocation, they can be associated with massive tears of the rotator cuff and with biceps tendon dislocations, or they can result from subcoracoid impingement. Subcoracoid impingement is caused by narrowing of the space between the tip of the coracoid process and the humerus, which may be congenital in origin or may result from a coracoid fracture or surgery. The narrowed space can result in impingement on, and resultant tears of, the subscapularis tendon ( Fig. 10-29 ). ,
Associations
- •
Anterior shoulder dislocations
- •
Long head, biceps tendon dislocations
- •
Massive rotator cuff tears
- •
Subcoracoid impingement
MRI
- •
Evaluate on axial images
- •
Detachment from lesser tuberosity
- •
Increased signal, thin, thick
- •
Contrast enhancement over the lesser tuberosity
- •
Associated tendon abnormalities
- •
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree