Shoulder Joint
Bigliani Classification of Acromial Morphology
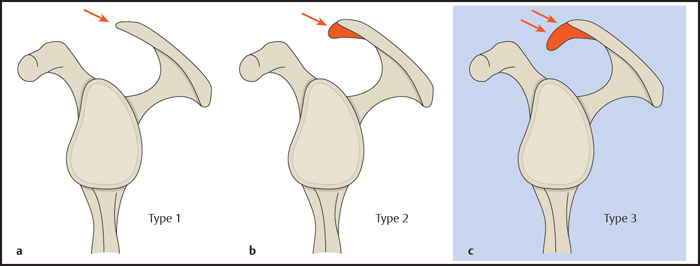
Bigliani et al (1986) identified three anatomic variants of acromial morphology in cadaver specimens based on radiographic outlet views of the shoulder joint ( Fig. 5.1 ):
Type 1: flat
Type 2: curved
Type 3: hooked
Moreover, a correlation was found between the type 3 acromion (and, to a lesser degree, type 2) and the development of rotator cuff tears.
Following the technique of Bigliani et al, acromial shape is evaluated on the outlet view radiograph (y view).
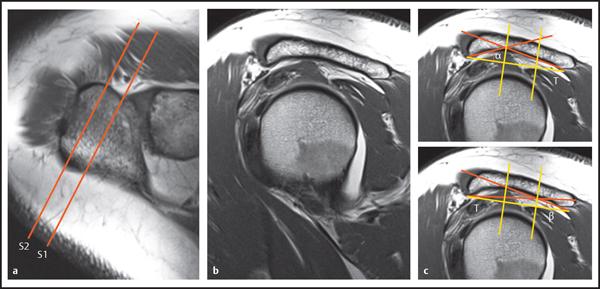
If magnetic resonance imaging (MRI) is used, acromial shape is evaluated on sagittal oblique images perpendicular to the supraspinatus muscle belly. The accuracy of this method is limited by the fact that the appearance of acromial shape varies somewhat with the position of the MRI plane. Mayerhofer et al performed a comparative study to determine the slice position that is most representative for depicting acromial shape ( Fig. 5.2 ). When just one sagittal MRI slice is used to evaluate acromial shape, the slice position S1 should be just lateral to the acromioclavicular joint. The image plane should not cut the joint capsule or acromioclavicular ligament. Accuracy can be increased by evaluating a second slice at a more lateral position, S2 (~ 4 mm lateral to the acromial margin). The shape of the acromion is assessed on slice S1. If a type 3 acromion is suspected, then the S2 slice is additionally evaluated because it is more specific for a type 3 morphology. This means that if S2 does not confirm type 3, a type 2 acromion is present.
A quantitative method is also available for determining acromial type. First a sagittal oblique slice is acquired, and a line tangent to the undersurface of the acromion is drawn and divided into thirds with two orthogonal lines as shown in Fig. 5.2 . Then the angle α between the anterior third and the posterior two-thirds of the acromion is measured. If α > 20°, then the angle between the anterior two-thirds and the posterior third (β) is also measured. The findings are interpreted as follows:
Acromial types
| α ≤ 10° |
| 10 < α ≤ 20° or α > 20° and β > 10° |
| α > 20° and β ≤ 10° |
The analysis is most accurate when the arithmetic means of the angles measured in S1 and S2 are calculated.
Bigliani et al also found a slight correlation between the type 2 acromion and rotator cuff tears, but subsequent studies were unable to confirm this finding. At present, only type 3 is considered a predisposing factor for subacromial impingement and rotator cuff tears. It appears, however, that the type 3 acromion is acquired rather than congenital, i.e., that the downward bony prominence results from age-related degenerative processes, usually involving the presence of enthesophytes at the attachment of the coracoacromial ligament.
Types of Os Acromiale
The acromion is preformed in cartilage. Three ossification centers appear in the acromion between 10 and 18 years of age and fuse by age 25 ( Fig. 5.3 ). A persistent ossification center (with a corresponding unfused growth plate) is called an os acromiale. The three acromial ossification centers are named as follows:
Preacromion
Mesoacromion
Meta-acromion
Park et al distinguished seven types of os acromiale based on the location of the fusion defect ( Fig. 5.3 ). Type I, caused by failure of fusion between the mesoacromion and meta-acromion, is by far the most common form. With conventional radiography, an os acromiale is most clearly depicted on axial views of the shoulder joint. With MRI and computed tomography (CT), transverse and coronal oblique images can be used to classify the type of os acromiale.
Os acromiale is important because it might be a predisposing factor for subacromial impingement.

Glenoid Version
Glenoid version or inclination is described by the scapuloglenoid angle, which is formed by the glenohumeral articular surface and a plane perpendicular to the body of the scapula ( Fig. 5.4 ). The scapuloglenoid angle can be measured on a transverse CT or MRI section that is perpendicular to the glenohumeral joint or glenoid articular surface and passes through the center of the glenoid fossa.
First the following reference lines are drawn: The first line (a) is tangent to the anterior and posterior glenoid rims. The second line (b) runs through the center of the glenoid and through the posterior margin of the scapular body. Glenoid version is then measured between line a and line b’, which is perpendicular to b.
Glenoid version
| 0–9° of retroversion |
| Retroversion > 15° |
| Anteversion > 5° |
Note: These reference values have been determined in an experimental setting.
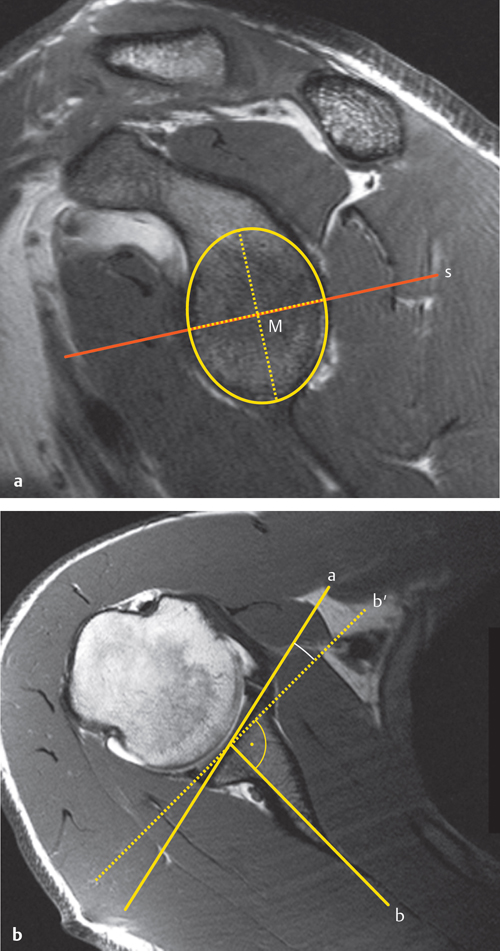
Abnormally increased retroversion is a significant causal factor in posterior instability. With glenoid dysplasia, retroversion is increased as the result of hypoplasia of the posteroinferior glenoid. The presence of 15° or more retroversion signifies at least an incomplete form of glenoid dysplasia. Increased anteversion (rare) may promote anterior instability of the glenohumeral joint.
Acromiohumeral Distance
Large rotator cuff tears and fatty degeneration of the constituent muscles may lead to secondary superior migration of the humeral head. The degree of this upward migration can be quantified on conventional radiographs by measuring the acromiohumeral distance (AHD; Fig. 5.5 ).
The AHD can be measured on an anteroposterior (AP) radiograph of the shoulder joint in neutral rotation, the Rockwood view, or the outlet view (y-view). The advantage of the Rockwood view is that the central ray is tangent to the slope of the acromion. Nevertheless, an AP radiograph in neutral rotation is still the most widely recommended view in the literature. The patient′s back is angled 30–45° to the film plane to give a tangential projection of the glenohumeral joint. The AHD is measured as the distance between the superior margin of the humeral head and the undersurface of the acromion. The reference values are as follows:

Acromiohumeral distance
| AHD = 1.05 cm |
| AHD ≤ 7 mm |
If the acromiohumeral distance is at or below the cutoff value of 7 mm, it should be assumed that a complete rotator cuff tear is present. In a study by Saupe et al, the size of the rotator cuff tear and the degree of fatty degeneration of the infraspinatus muscle were found to have the greatest influence on acromiohumeral distance.
Rotator Cuff Tears
General Classification
Rotator cuff tears are classified as complete or partial ( Fig. 5.6 ):
Complete tear: A complete tear is defined as one that extends through the full thickness of the tendon (from the articular to the bursal surface). It is sufficient for the tear to involve the entire thickness of the tendon at a single site. Thus, “complete” does not necessarily mean that the tendon is completely severed over its entire width.
Partial tear: Partial tears are partial-thickness lesions. They are further classified by their location as bursal-sided tears, articular-sided tears, and intratendinous tears. These types are most easily identified on oblique coronal MRI images angled parallel to the supraspinatus muscle.
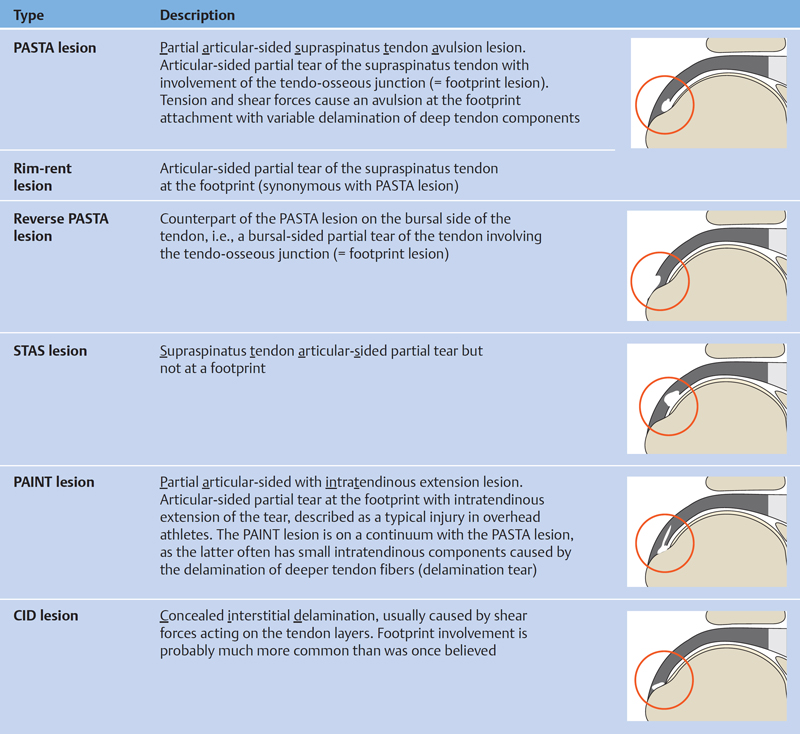
Specific Types of Rotator Cuff Tears
Recent discoveries on the location, pathogenic mechanism, and treatment implications of rotator cuff tears have led to subclassifications that stress the importance of specific lesion types. Because a uniform classification does not exist, lesions that are the same or very similar are sometimes described with different terms and are often designated by acronyms.
Several types of tear are described and illustrated in Fig. 5.7 .
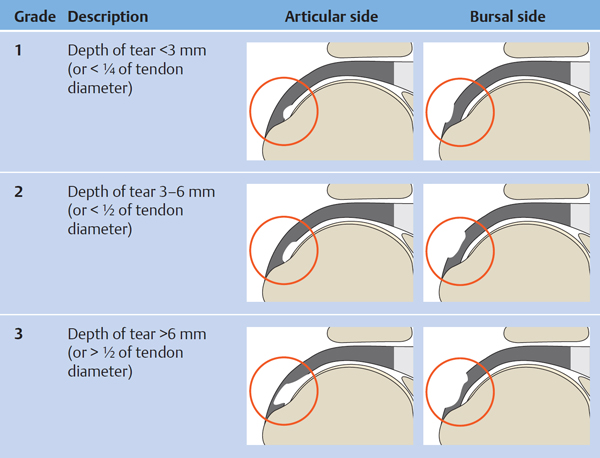
Ellman Classification of Rotator Cuff Tears
Partial rotator cuff tears can be classified by the depth of the tear ( Fig. 5.8 ). The diameter of an intact tendon is 1.0–1.2 cm. The Ellman classification also indicates which side of the tendon is affected (A = Articular side, B = Bursal side).
Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res 1990;254(254):64–74Snyder Classification of Rotator Cuff Tears
The Snyder or SCOI (Southern California Orthopedic Institute) classification of rotator cuff tears is widely used in orthopedics. The initial letter of the designation indicates whether the lesion is an articular-sided partial tear (A), a bursal-sided partial tear (B), or a complete tear (C). The letter is followed by a number indicating the degree of tendon damage visible at arthroscopy.
Table 5.1 shows the numerical designations used for partial tears, and Table 5.2 shows the designations used for complete tears.
Since the evaluation of tendon damage in this classification is based on arthroscopic appearance, the designations are not fully applicable to radiologic findings.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree