Chapter Outline
Ultrasound Examination Technique
Position 1: Long Head of Biceps Brachii Tendon
Position 2: Subscapularis and Biceps Tendon Dislocation
Position 3: Supraspinatus and Infraspinatus
Position 4: Acromioclavicular Joint, Subacromial-Subdeltoid Bursa, and Dynamic Evaluation
Position 5: Infraspinatus, Teres Minor, and Posterior Glenoid Labrum
Supraspinatus Tears and Tendinosis
Infraspinatus Tears and Tendinosis
Subscapularis Tears and Tendinosis
Pitfalls in Rotator Cuff Ultrasound
Glenoid Labrum and Paralabral Cyst
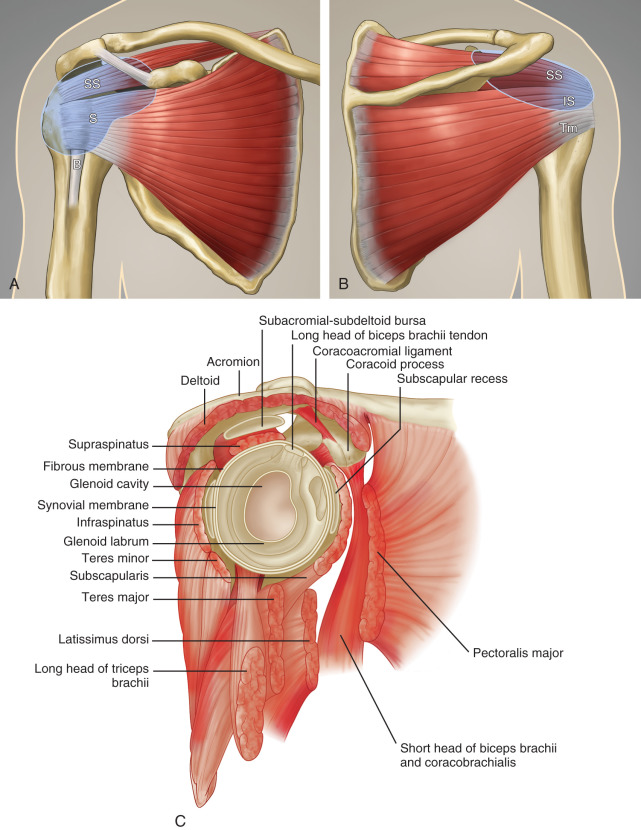
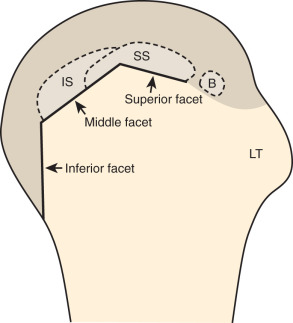
The rotator cuff is composed of four tendons ( Fig. 3.1 ). Anteriorly, the subscapularis with its tendons converges onto the lesser tuberosity. Superiorly, the supraspinatus inserts on the superior aspect of the greater tuberosity; its footprint or attachment averages 2.25 cm anterior to posterior, which covers the superior facet and the anterior portion of the middle facet of the greater tuberosity ( Fig. 3.2 ). Uncommonly, anterior fibers of the supraspinatus may extend anterior to the lesser tuberosity. Posterior to the scapula and inferior to the scapular spine, the infraspinatus tendon inserts on the middle facet of the greater tuberosity, overlapping the posterior aspect of the supraspinatus tendon. The smaller and more inferior teres minor tendon inserts on the inferior facet of the greater tuberosity. Between the lesser and greater tuberosities anteriorly is the bicipital groove, which contains the long head of the biceps brachii tendon; although not a part of the rotator cuff, its proximal intra-articular portion courses through a space between the supraspinatus and subscapularis tendons, called the rotator interval . The intra-articular portion of the biceps tendon is stabilized by the biceps reflection pulley comprised of the superior glenohumeral ligament and the coracohumeral ligament, which are essentially thickened reflections of the joint capsule. The glenohumeral joint normally communicates with the biceps brachii long head tendon sheath. Several joint recesses also exist and include the axillary recess, which extends inferiorly, and the subscapularis recess, which extends medially through the rotator interval to be located inferior to the coracoid process at the superior aspect of the subscapularis tendon in an inverted U shape. In contrast, the subcoracoid bursa is located anterior to the subscapularis and does not communicate with the glenohumeral joint. The subacromial-subdeltoid bursa is located between the rotator cuff and the overlying deltoid muscle and acromion ( Fig. 3.1 ). The glenoid labrum represents a rim of fibrocartilage at the periphery of the glenoid.
Ultrasound Examination Technique
Table 3.1 is a shoulder ultrasound examination checklist. Examples of diagnostic shoulder ultrasound reports are shown in Boxes 3.1 and 3.2 .
Examination: Ultrasound of the Shoulder
Date of Study: March 11, 2017
Patient Name: Juan Atkins
Registration Number: 8675309
History: Shoulder pain, evaluate for rotator cuff abnormality
Findings: No evidence of joint effusion. The biceps brachii long head tendon is normal without tendinosis, tear, tenosynovitis, or subluxation/dislocation. The supraspinatus, infraspinatus, subscapularis, and teres minor tendons are also normal. No subacromial-subdeltoid bursal abnormality and no sonographic evidence for subacromial impingement with dynamic maneuvers. The posterior labrum is unremarkable. Additional focused evaluation at site of maximal symptoms was unrevealing.
Impression: Unremarkable ultrasound examination of the shoulder. No rotator cuff abnormality.
Examination: Ultrasound of the Shoulder
Date of Study: March 11, 2017
Patient Name: Chazz Michael Michaels
Registration Number: 8675309
History: Shoulder pain, evaluate for rotator cuff abnormality
Findings: There is a focal anechoic tear of the anterior, distal aspect of the supraspinatus tendon measuring 1 cm short axis by 1.5 cm long axis. The anterior margin of the tear is adjacent to the rotator interval. There is no involvement of the subscapularis, infraspinatus, or rotator interval. A moderate amount of infraspinatus and supraspinatus fatty degeneration is present. There is a small joint effusion distending the biceps brachii tendon sheath and moderate distention of the subacromial-subdeltoid bursa. No biceps brachii long head tendon abnormality and no subluxation/dislocation. Mild osteoarthritis of the acromioclavicular joint. Additional focused evaluation at site of maximal symptoms was unrevealing.
Impression: Focal or incomplete full-thickness tear of the supraspinatus tendon with infraspinatus and supraspinatus muscle atrophy.
General Comments
For ultrasound examination of the shoulder, the patient sits on a stool with low back support but without wheels, and the sonographer sits on a stool with wheels to allow easy maneuvering. For examination of the patient’s left shoulder when holding the transducer with the right hand, the patient faces the ultrasound machine, with the sonographer sitting somewhat between the patient and ultrasound machine ( Fig. 3.3A ). For examination of the patient’s right shoulder, the patient turns toward the left and faces the sonographer ( Fig. 3.3B ). The transducer frequency for the shoulder is generally at least 10 to 15 MHz, although one may need to use a lower frequency in evaluation of the deeper structures such as the posterior glenoid labrum or if the patient has a large body habitus. Following a sequence of steps will ensure a complete and thorough evaluation. Although a targeted approach is often used in other peripheral joints, this is not recommended with the shoulder because pain is often diffuse or referred. It is recommended, however, that every sonographic evaluation be followed by targeted evaluation over any area with point tenderness or focal symptoms.

Position 1: Long Head of Biceps Brachii Tendon
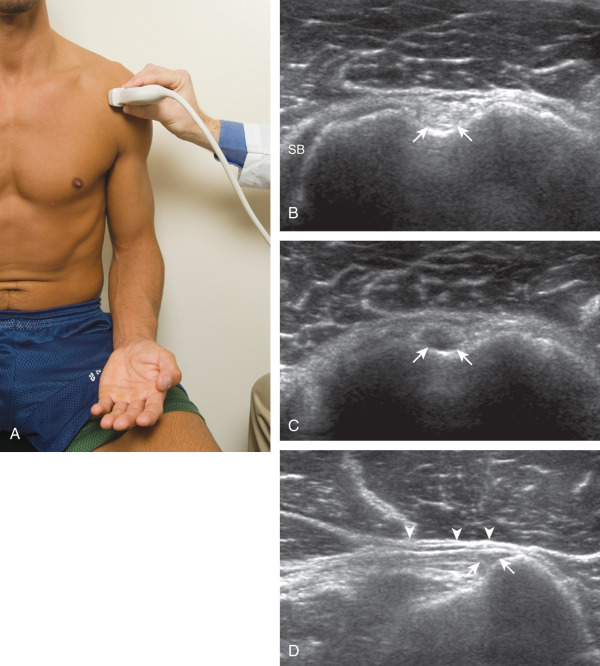
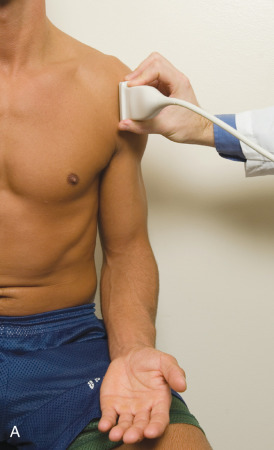
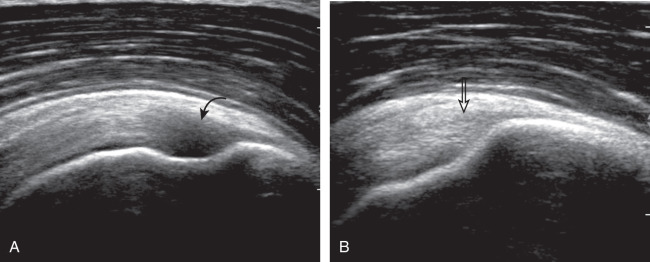
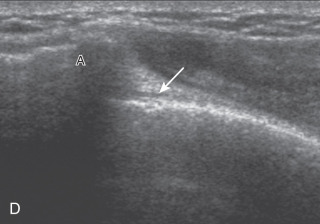
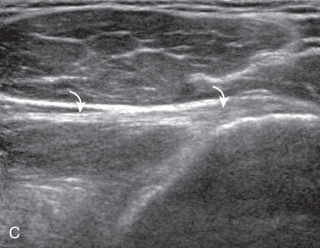
The patient places the hand on his or her leg ( Fig. 3.4A ). This position rotates the bicipital groove anteriorly, an important bone landmark. The hand may be in any position as this has no effect on the humerus. The transducer is placed in the transverse plane on the patient, and the long head of the biceps brachii tendon is seen within the bicipital groove in short axis ( Fig. 3.4B ) ( ). Because the distal biceps tendon courses deep, tendon obliquity to the transducer sound beam commonly creates anisotropy and an artifactual hypoechoic appearance of the normal tendon ( Fig. 3.4C ). This is corrected by toggling the transducer to aim the sound beam superiorly ( ). A hyperechoic and well-defined humeral cortex in the floor of the bicipital groove indicates that the sound beam is perpendicular to the overlying biceps tendon. The biceps brachii tendon is evaluated in short axis from proximal to distal. The proximal aspect of the biceps brachii tendon over the humeral head to the level of biceps reflection pulley is evaluated as this is a common site for pathology. Proximal to the bicipital groove, the long head of the biceps brachii tendon normally appears oval in an oblique orientation, which should not be mistaken for tendon subluxation. Evaluation is also continued inferiorly to the level of the pectoralis tendon ( Fig. 3.4D ) to assess the pectoralis and biceps because complete biceps brachii long head tendon tears may retract to this level. The transducer is then turned 90 degrees to visualize the tendon in long axis from the humeral head to the pectoralis tendon ( Fig. 3.5A ) ( ). Asymmetrical pressure on the distal aspect of the transducer (or heel-toe maneuver) is typically needed to bring the biceps tendon fibers perpendicular to the transducer sound beam to eliminate anisotropy ( Fig. 3.5B and C ) ( ). An additional method to visualize the biceps tendon in long axis is to identify the characteristic pyramid shape of the lesser tuberosity ( Fig. 3.5D ); movement of the transducer laterally from this point will visualize the bicipital groove and biceps brachii long head tendon ( ).
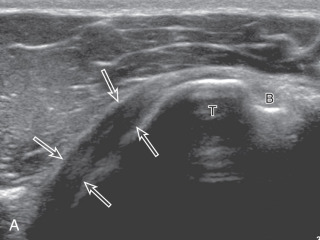
Position 2: Subscapularis and Biceps Tendon Dislocation
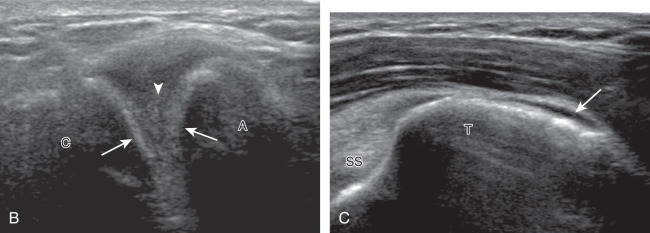
The transducer is placed in the transverse plane, as before, to first visualize the bicipital groove and then the transducer is moved medial over the lesser tuberosity (see Fig. 3.4A ). In this neutral position, although the subscapularis tendon can be seen in long axis, there is significant anisotropy ( Fig. 3.6A ). Ask the patient to rotate the shoulder externally ( Fig. 3.6B ), and this will bring the subscapularis tendon fibers into view perpendicular to the transducer sound beam and will eliminate anisotropy ( Fig. 3.6C ) ( ). The transducer is then moved superiorly and inferiorly over the lesser tuberosity to ensure complete evaluation of the subscapularis tendon. The transducer should also be moved laterally over the bicipital groove to evaluate for potential biceps brachii tendon subluxation or dislocation, which may be present only in external rotation (see Biceps Brachii Tendon, Subluxation and Dislocation). Center the transducer over the distal subscapularis tendon again, rotate the transducer 90 degrees, and assess the subscapularis tendon in short axis ( Fig. 3.7A and B ). In this view, it is common to see hypoechoic striations of muscle or interfaces between the several tendon bundles ( Fig. 3.7C ) ( ).


Position 3: Supraspinatus and Infraspinatus
The goal and challenge when imaging the supraspinatus is to evaluate the tendon precisely in long and short axis, identifying characteristic bone landmarks. This will avoid numerous diagnostic pitfalls and is an indicator that the operator has a thorough understanding of anatomy and shoulder ultrasound technique. The key to obtaining such images is to understand the anatomy of the greater tuberosity and the effects of various shoulder positioning. If one wanted to assess the supraspinatus tendon in long axis with the shoulder in neutral position, the transducer would be placed in the coronal plane over the greater tuberosity. While the distal supraspinatus and related pathology can be seen, more proximal pathology may not be visible due to shadowing from the acromion ( Fig. 3.8 ). One way to correct this is to ask the patient to place the back of his or her ipsilateral hand in the lower lumbar region and to keep the elbow close to the body (called the Crass position ) ( Fig. 3.9 ). In this position, the humerus is rotated internally such that the greater tuberosity is located anteriorly on the patient. By placing the transducer in the sagittal plane anteriorly on the patient over the greater tuberosity, a long axis view of the supraspinatus tendon is demonstrated. Rotating the transducer 90 degrees (or transverse on the patient) will produce a short axis image of the supraspinatus. The Crass position is helpful when one is first learning shoulder ultrasound technique in that long and short axis views are easily obtained; however, the significant disadvantages of this position include limited view of the rotator interval (see discussion later in chapter) and, often, significant patient discomfort. Because of this, the modified Crass position is used (I primarily use the modified Crass position and less commonly the Crass position for problem solving).

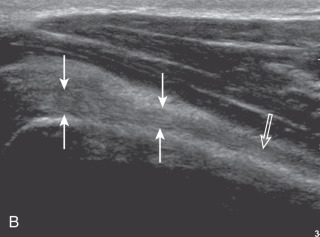
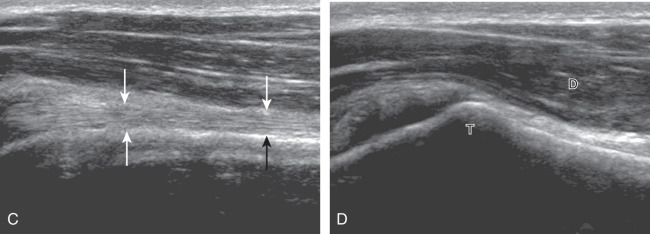
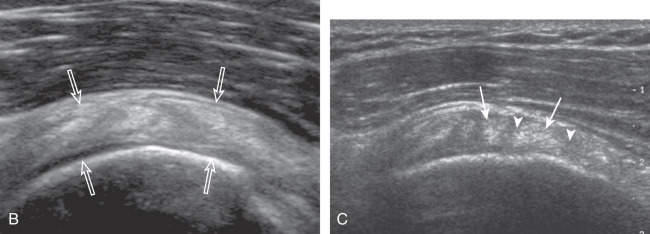
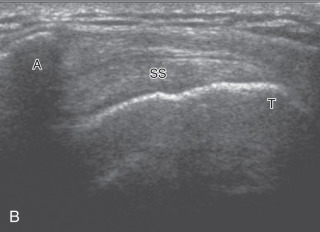
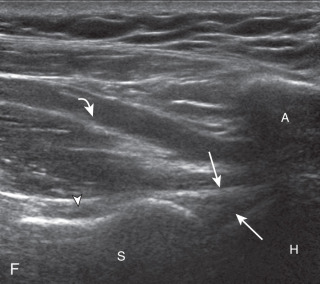
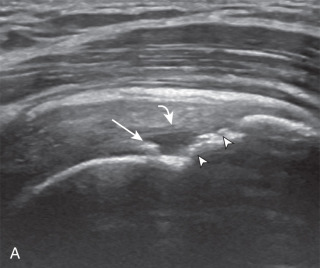
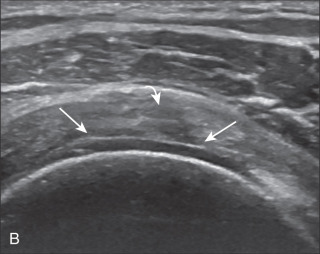
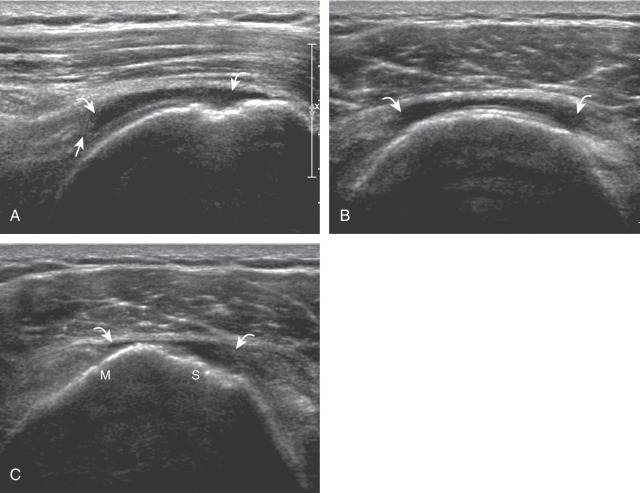
To obtain the modified Crass position, the patient is asked to place his or her hand on the ipsilateral hip area ( Fig. 3.10 ). The elbow should be pointed posteriorly to ensure some degree of shoulder external rotation compared with the Crass position; otherwise, the rotator interval may not be visible. To obtain a long axis view of the supraspinatus tendon in this position, the transducer is placed on the rounded contour of the anterior shoulder and directed superior and oblique toward the patient’s ear ( Fig. 3.10 ). Usually, the axis of the transducer is parallel to the proximal biceps tendon and humeral shaft regardless of each position when imaging the supraspinatus in long axis. With positioning of the patient in the Crass or modified Crass position, supraspinatus evaluation begins with evaluation in long axis because this important view allows visualization of the three surfaces of the supraspinatus tendon (articular, bursal, greater tuberosity) and allows for initial screening for pathology. In long axis, the normal supraspinatus will appear hyperechoic and fibrillar, with a convex superior margin ( Fig. 3.10 ) ( ). The thin hypoechoic layer over the curved humeral head represents the hyaline articular cartilage. A thin hypoechoic fibrocartilage layer over the greater tuberosity facets should not be confused with hyaline articular cartilage over the rounded humeral head. One must be aware that the distal fibers of the tendon curve downward at the greater tuberosity near the articular surface, and the transducer orientation should be adjusted using the heel-toe maneuver to eliminate anisotropy ( Fig. 3.11 ) ( ). A hyperechoic and well-defined humeral head cortex indicates that the sound beam is perpendicular to the bone and overlying tendon. The footprint of the supraspinatus tendon inserts over approximately 2.25 cm of the greater tuberosity shelf from anterior to posterior, so the transducer should be moved anterior and posterior over the greater tuberosity without changing the long axis imaging plane to ensure complete evaluation. Scanning should be continued anteriorly along the greater tuberosity until the intra-articular portion of the biceps tendon is identified to ensure that the anterior extent of the supraspinatus was evaluated, a location where supraspinatus tendon tears commonly occur. Including a long axis image of the intra-articular portion of the long head biceps brachii tendon will document that the most anterior aspect of the supraspinatus was evaluated ( Fig. 3.10C ). As the transducer is moved posteriorly over the middle facet of the greater tuberosity, the infraspinatus is also evaluated ( Fig. 3.10D ). At the middle facet, the angle between the greater tuberosity and the articular surface of the humeral head flattens, and alternating hypoechoic linear areas representing anisotropy of the infraspinatus helps to identify the infraspinatus tendon superficial to the supraspinatus tendon ( ). The transducer can then be angled more posterior to align the infraspinatus in long axis ( Fig. 3.12 ).

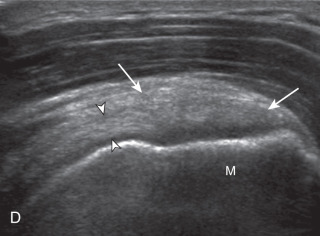

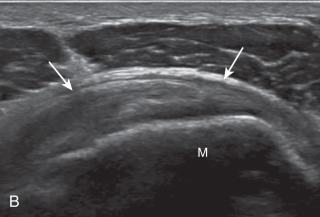
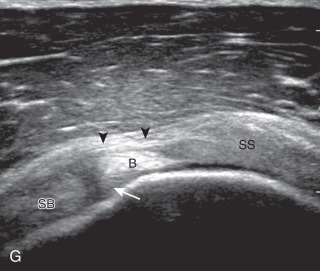
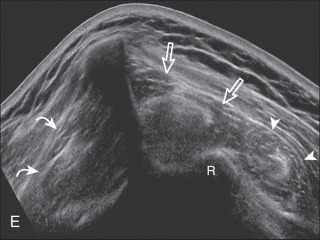
After assessment of the supraspinatus in long axis, the transducer is turned 90 degrees to evaluate the tendon in short axis ( Fig. 3.13A ) ( ). First, beginning over the proximal aspect of the supraspinatus, the humeral head should be seen as a round echogenic line with overlying hypoechoic hyaline cartilage ( Fig. 3.13B ). The transducer should be toggled until the bone cortex and overlying tendon are hyperechoic and well defined to eliminate anisotropy ( Fig. 3.14 ). At this level, the rotator cuff should be of fairly uniform thickness, similar to a tire on a wheel rim, measuring on average 6 ± 1.1 mm. This appearance indicates that the transducer is in the true short axis plane relative to the supraspinatus tendon and not in an oblique plane. The transducer is then moved distally relative to the supraspinatus tendon ( ). As the hyaline cartilage disappears from view, the round humeral head surface will be replaced with the angulated surface of the greater tuberosity facets ( Fig. 3.13C ). At this point, the tendon uniformly becomes thinner, an indication that the transducer position is now beyond the articular surface. The facets of the greater tuberosity from anterior to posterior appear as three flat surfaces: the superior, middle, and inferior facets (see Fig. 3.2 ). The supraspinatus tendon inserts on the superior facet and the superior half of the middle facet, the infraspinatus inserts on the middle facet (overlapping the supraspinatus tendon superficially), and the teres minor inserts on the inferior facet. At this point, both the distal supraspinatus and infraspinatus are assessed. Similar to long axis imaging, alternating hypoechoic lines are seen over the middle facet, which represent anisotropy of the infraspinatus tendon fibers superficial to the supraspinatus ( ). As the transducer is moved more distally, the greater tuberosity becomes square or rounded ( Fig. 3.13D ), and the rotator cuff thins even more and eventually disappears as the transducer moves beyond the greater tuberosity and the rotator cuff ( Fig. 3.13E ). Similar to evaluation of the supraspinatus tendon in long axis, the intra-articular portion of the biceps tendon (in the rotator interval) should be identified to indicate that the most anterior aspect of the supraspinatus tendon is evaluated ( Fig. 3.13G ). This is one of the advantages of the modified Crass position because the important landmark of the biceps tendon is well visualized. In addition, the superior glenohumeral ligament is seen at the anterior aspect of the biceps tendon adjacent to the humerus, and the coracohumeral ligament is identified over the biceps tendon as it courses lateral to merge with the supraspinatus tendon.
Another structure of the rotator cuff is the rotator cable, which may be identified by its characteristic shape and position ( Fig. 3.15 ). The rotator cable has a U shape when viewed from above with each limb attaching to the greater tuberosity. The curved aspect of the U is visualized with its fibers perpendicular to the supraspinatus at the articular surface. The rotator cable is more prominent in some individuals (termed cable dominant ) and outlines an area of the rotator cuff within the U , termed the rotator crescent .
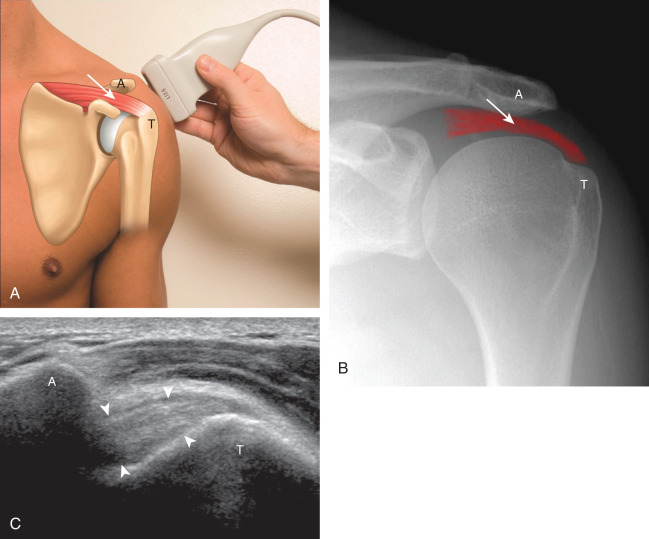
Position 4: Acromioclavicular Joint, Subacromial-Subdeltoid Bursa, and Dynamic Evaluation
The acromioclavicular joint can be located with palpation of the clavicle and placement of the transducer in the coronal-oblique plane over the distal clavicle ( Fig. 3.16A ) or by moving the transducer superiorly in the transverse plane from the bicipital groove region. The acromioclavicular joint is identified by hypoechoic joint space and bone landmarks; the clavicle is normally seen more superior relative to the acromion. A hyperechoic fibrocartilage disk may be seen between the clavicle and acromion, and the hypoechoic joint capsule is normally less than 3 mm measured superiorly ( Fig. 3.16B ). If the acromioclavicular joint is widened, the patient can place his or her hand on the opposite shoulder to assess for acromioclavicular joint widening or, conversely, narrowing, which may be associated with pain. The transducer is then moved laterally in the coronal place over the proximal humerus beyond the greater tuberosity to assess for fluid within the dependent portion of the subacromial-subdeltoid bursa ( Fig. 3.16C ).

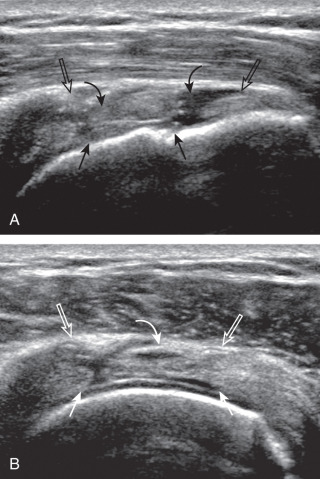
To dynamically assess for subacromial impingement, the transducer is positioned in the coronal-oblique plane to visualize the lateral border of the acromion and the adjacent greater tuberosity ( Fig. 3.17 ). The examiner assesses the supraspinatus tendon and subacromial-subdeltoid bursa dynamically first by passively abducting the arm (typically with elbow flexion). This allows the examiner to slow or stop the patient’s movement if the bone landmarks are not visualized to allow repositioning of the transducer and also trains the patient to abduct the arm at a particular speed. The movement is then repeated actively ( Fig. 3.17C and D ). Subsequent pooling of fluid within or bunching of the subacromial-subdeltoid bursa indicates subacromial impingement, although more advanced cases can show additional upward movement of the humeral head and osseous impingement. The finding of incomplete sliding of the supraspinatus beneath the acromion during this dynamic maneuver indicates adhesive capsulitis. When assessing for subacromial impingement, the transducer should also be moved anterior to the acromion to assess the region of the coracoacromial ligament for abnormal distention of the subacromial-subdeltoid bursa.


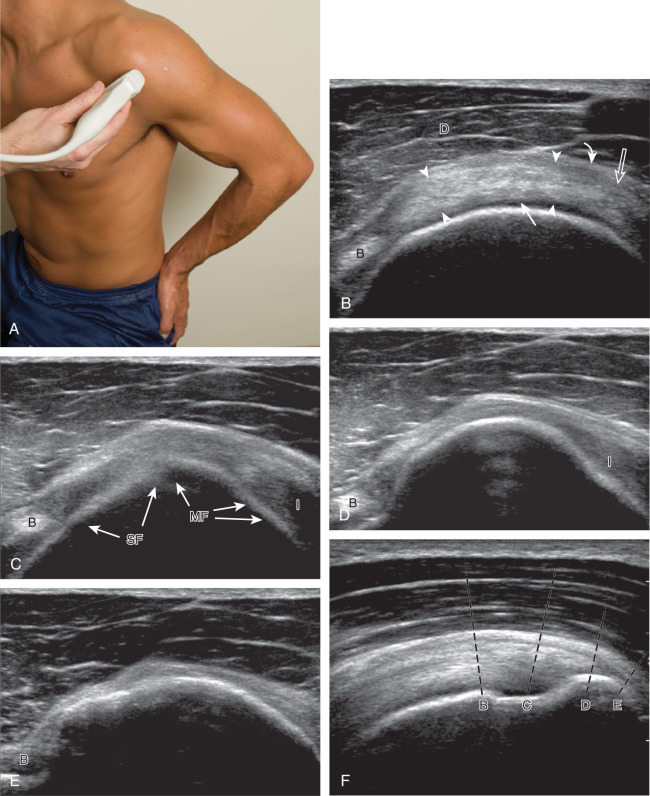
Position 5: Infraspinatus, Teres Minor, and Posterior Glenoid Labrum
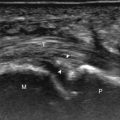
The patient rotates on the stool to permit visualization of the posterior structures of the shoulder; initially, the patient keeps his or her hand on the thigh. Place the transducer in the oblique axial plane angled superiorly toward the humeral head parallel and just inferior to the scapular spine ( Fig. 3.18 ). Position the transducer to visualize the well-defined central tendon of the infraspinatus muscle at the musculotendinous junction posterior to the glenoid to ensure an imaging plane that is long axis to the infraspinatus ( Fig. 3.18B ). The infraspinatus tendon can then be followed distally to its insertion on the middle facet at the posterior aspect of the greater tuberosity. Evaluation of the distal infraspinatus tendon supplements earlier evaluation from the modified Crass position (see Figs. 3.10D and 3.12 ). If the infraspinatus tendon is not visible because of shadowing beneath the acromion, then the patient can place the hand on the opposite shoulder to improve visualization; this maneuver is less ideal because the infraspinatus tendon, seen linear and perpendicular to the sound beam in neutral shoulder position, becomes curved, introducing anisotropy. The transducer can then be moved inferiorly to visualize the smaller teres minor, with its tendon more superficial over the muscle compared with the infraspinatus tendon ( Fig. 3.18C ). The transducer is then turned 90 degrees to evaluate the infraspinatus and teres minor in short axis ( Fig. 3.19 ). Note osseous landmarks of scapula spine and osseous ridge of posterior scapula that demarcates the supraspinatus, infraspinatus, and teres minor ( Fig. 3.19E ).

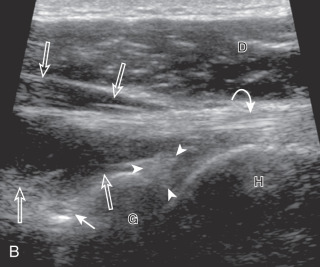

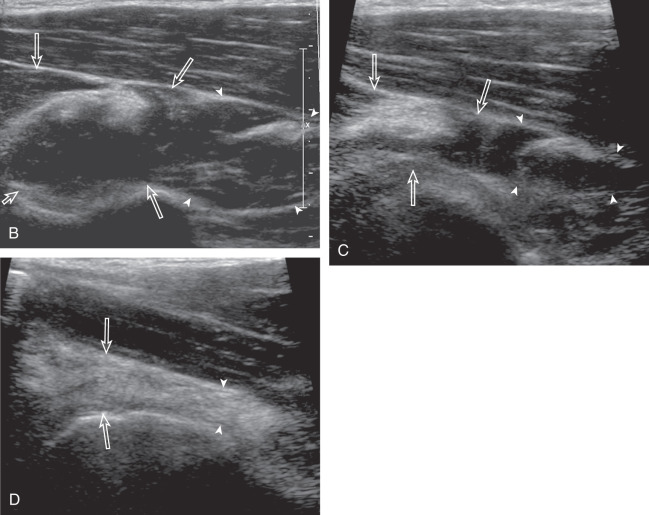
An alternate approach in identification of the infraspinatus and teres minor is to palpate the scapular spine, place the transducer sagittal on the patient over the scapular spine, and then move the transducer inferiorly. The first structure identified inferior to the scapular spine is the infraspinatus. Once the infraspinatus and teres minor are identified, the transducer is turned long axis to the infraspinatus tendon to evaluate the hyperechoic triangle-shaped posterior glenoid labrum (see Fig. 3.18B ).
The area medial to the glenohumeral joint should also be assessed to include the spinoglenoid notch, a site where paralabral cysts may be found. The patient can actively internally and externally rotate the shoulder to assess the infraspinatus tendon and posterior glenoid labrum dynamically ( ). External rotation improves visualization of joint fluid distention of the posterior recess, which also facilitates evaluation of potential paralabral tears (see Glenoid Labrum and Paralabral Cyst ). In shoulder external rotation, the suprascapular vein may dilate, and this can simulate a paralabral cyst (see Glenoid Labrum and Paralabral Cyst ) ( ), especially since blood flow is too slow to be detected at Doppler imaging. Unlike a paralabral cyst, the suprascapular vein collapses with internal rotation.
To complete the posterior shoulder examination, the transducer is turned 90 degrees and moved medial to assess the infraspinatus and teres minor in short axis globally at the musculotendinous junctions for fatty degeneration or atrophy; the infraspinatus muscle should be nearly twice the size of the teres minor over the scapular body, with normal muscle appearing relatively hypoechoic compared with hyperechoic tendon (see Fig. 3.19B ). At this site, a bony ridge is identified in the scapula, which forms a concave surface beneath each muscle and aids in their identification. The transducer can be moved superiorly to similarly assess the supraspinatus muscle in short axis for fatty infiltration and atrophy. An extended field of view image may be considered (if available on the ultrasound machine) to include the supraspinatus, infraspinatus, and teres minor in one image (see Fig. 3.19E ). The transducer is then turned 90 degrees and long axis to the supraspinatus, where the concavity of the superior scapular cortex identifies the suprascapular notch and at times portions of the superior labrum ( Fig. 3.19F ).
Rotator Cuff Abnormalities
Supraspinatus Tears and Tendinosis
General Comments
Most rotator cuff tears involve the supraspinatus tendon, although they may extend posterior to involve the infraspinatus and anterior to involve the biceps reflection pulley and subscapularis tendons. The anterior aspect of the distal supraspinatus is a common site of tear, often near the rotator interval, although a more posterior location near the supraspinatus-infraspinatus junction has been described with degenerative cuff tears. Most tendon tears are the result of chronic attrition and possible superimposed injury, and they typically occur after the age of 40 years. Such chronic supraspinatus tears occur distally and are associated with cortical irregularity of the greater tuberosity, an important indirect sign of supraspinatus tendon tear. Acute tears may occur more proximally and may or may not have associated cortical irregularity, depending on the age of the patient and the chronicity of the rotator cuff. Accurate localization of a tendon tear is essential to classify the tear properly ( Fig. 3.20 ). For example, partial-thickness tears could involve the articular or bursal surface of the tendon. A tear that is localized within the tendon or that extends only to the greater tuberosity surface (or footprint) of the supraspinatus attachment is called an interstitial or intra-substance (or concealed interstitial delamination) tear because it would not be visible at arthroscopy or bursoscopy. A tear that extends from articular to bursal surfaces is a full-thickness tear. Correct description and nomenclature are also essential. A full-thickness tear may be focal or incomplete, whereas a full-thickness tear that involves the entire width of a tendon can be termed a complete or full-width full-thickness tear. Initial evaluation in long axis of the supraspinatus is recommended in that the three surfaces of the rotator cuff (articular, bursal, greater tuberosity) and characteristic bone contours are visible and easily identified. Most tears are anechoic or hypoechoic, although acute tears will more likely appear anechoic from fluid. As a supraspinatus tendon tear becomes large, tendon retraction and volume loss of the tendon occur, with loss of the normal superior convex shape. Full-thickness tears located anteriorly are associated with tendon retraction, muscle atrophy, and propagation over time. Ultrasound and magnetic resonance imaging (MRI) have comparable accuracies in detection and measurement of rotator cuff tears. A meta-analysis of 65 articles has also shown that ultrasound and MRI are comparable in sensitivity and specificity for the diagnosis of rotator cuff tear. An algorithm approach to diagnostic imaging evaluation of suspected rotator cuff disease has been suggested that incorporates ultrasound.
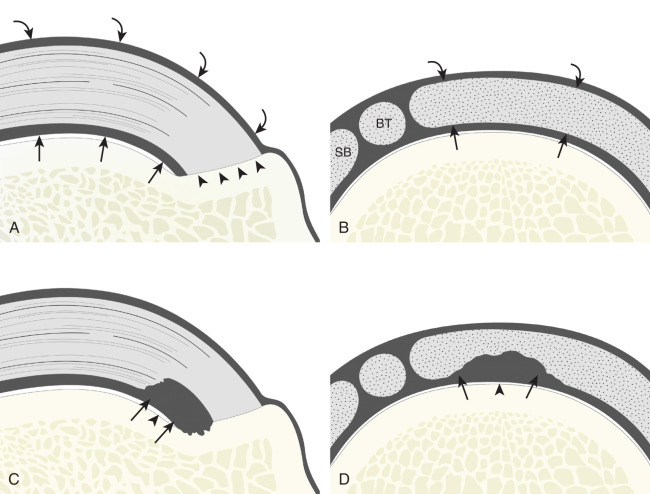
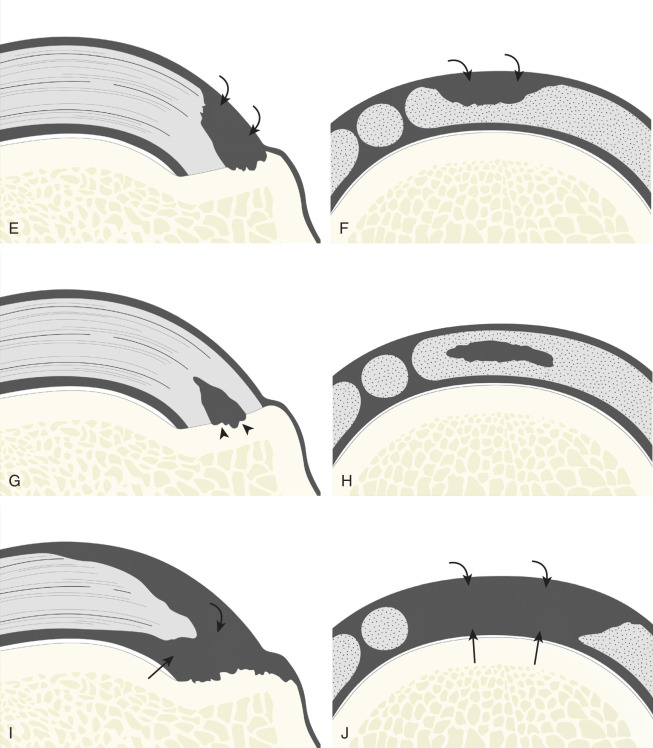
Partial-Thickness Tear
Partial-thickness supraspinatus tendon tears are characterized by a well-defined hypoechoic or anechoic abnormality that disrupts the tendon fibers, which may be articular-side or bursal-side partial-thickness tears determined by which surface of the tendon is involved. An intra-substance or interstitial tear may also be considered a form of partial-thickness tear, but one that does not extend to the articular or bursal surface.
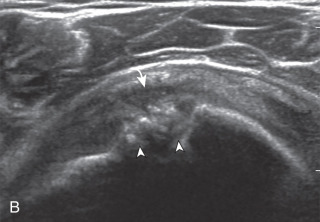
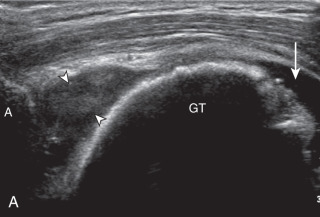
Articular-side partial-thickness tears most commonly involve the supraspinatus anteriorly and distally at the greater tuberosity and are seen with increased frequency in patients younger than 40 years. A mixed hyperechoic-hypoechoic appearance may be present, which represents hypoechoic fluid that surrounds the hyperechoic torn tendon stump ( Figs. 3.21, 3.22, 3.23, and 3.24 ). Cortical irregularity of the greater tuberosity immediately adjacent to the tendon tear is common, related to the chronic cuff attrition at the site of the tear. An acute tear of a previously normal cuff or a proximal tear ( Fig. 3.24 ) will not be associated with cortical irregularity, although these tears are less common. With an articular-side partial-thickness tear, the superior surface of the tendon remains convex because global tendon volume loss is usually absent. Articular surface extension of a tear is suggested when the tear is in direct contact with the hypoechoic hyaline cartilage. The hyperechoic interface between the tendon tear and the hyaline cartilage may be accentuated in this situation (called the cartilage interface sign ). The terms rim-rent tear and PASTA (partial articular-side supraspinatus tendon avulsion) lesion are used specifically to describe a far-distal articular-side partial-thickness tear, immediately adjacent to the greater tuberosity surface ( , . and ). Recall that the articular fibers of the distal supraspinatus tendon abruptly redirect to attach to the greater tuberosity and this tendon orientation will often create a focal hypoechoic area from anisotropy that should not be mistaken for an articular-side partial-thickness tear (see Fig. 3.69 ).
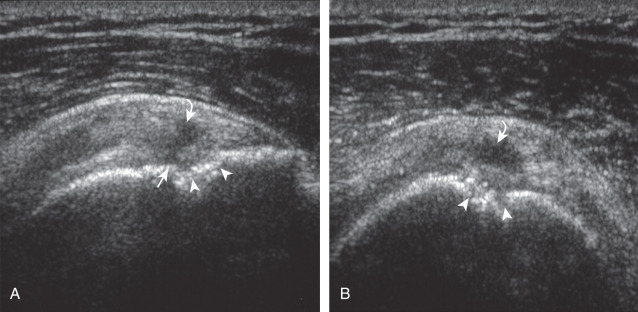
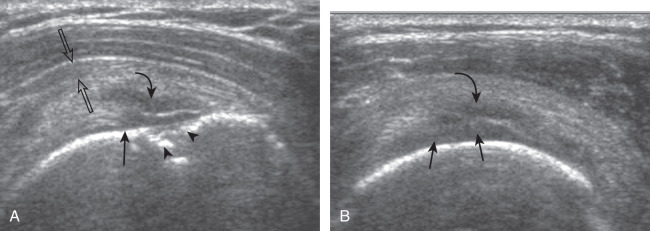
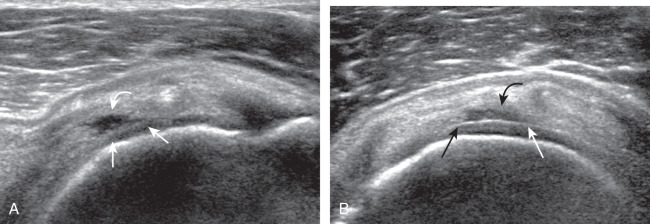
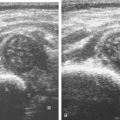
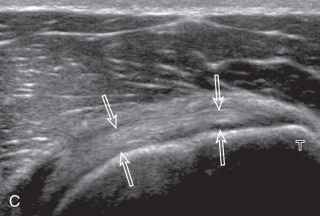
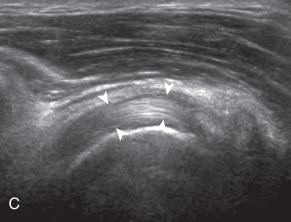
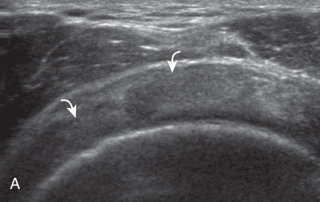
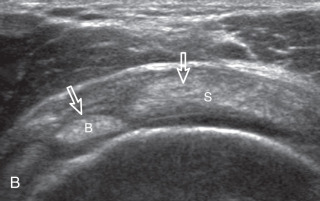
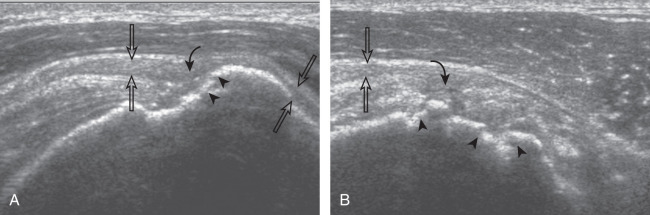
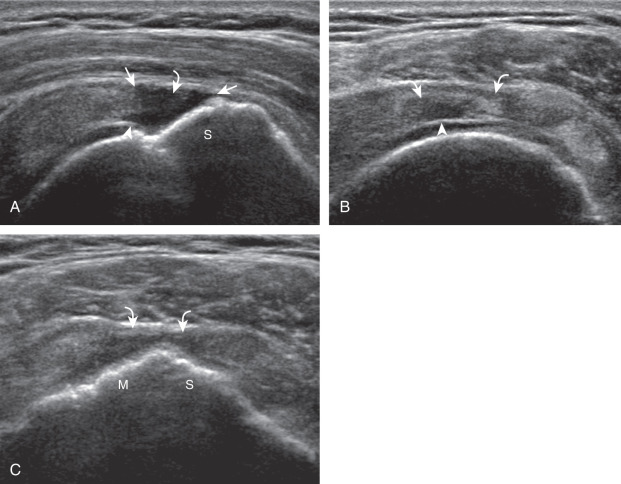
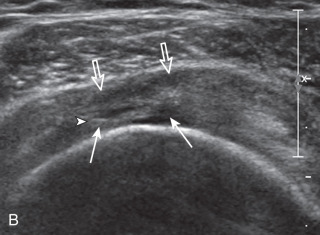
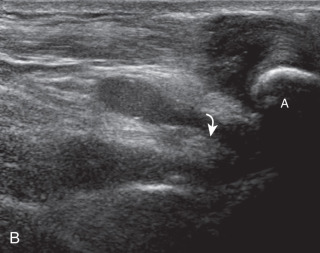
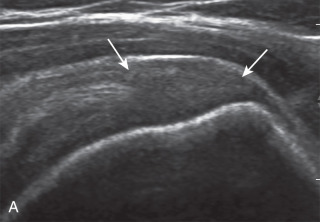
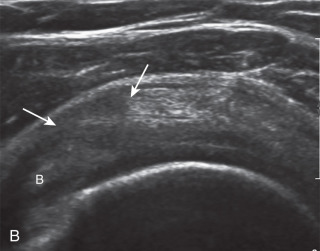
A bursal-side partial-thickness supraspinatus tendon tear is also hypoechoic or anechoic, but it is localized to the bursal surface ( Figs. 3.25, 3.26, 3.27, and 3.28 ). Tear extension from the bursal surface to the greater tuberosity surface (or tendon footprint), without extension to the articular surface, is still considered a bursal-side partial-thickness tear. This results in focal absence of tendon or uncovering of the distal greater tuberosity footprint ( ). Because of the superficial location of the tear, tendon thinning and volume loss of the cuff are usually present. This situation results in loss of the normal superior convexity of the supraspinatus tendon surface, with dipping of the deltoid muscle and subacromial-subdeltoid bursa into the torn tendon gap. Similar to other supraspinatus tendon tears, greater tuberosity cortical irregularity is typically present because the tear extends from the bursal surface to the greater tuberosity surface. If adjacent subacromial-subdeltoid bursal synovial hypertrophy is present, hypoechoic or isoechoic synovial tissue may fill the torn tendon gap, making the tear and tendon thinning less conspicuous ( Fig. 3.28 ) ( ).
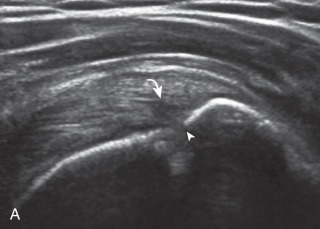
A tendon tear that does not contact the articular or bursal side of the supraspinatus is termed an intrasubstance or interstitial tear . Such tears may be anechoic or hypoechoic, located within the tendon substance or in contact with the greater tuberosity surface ( Fig. 3.29 ). Cortical irregularity is often seen in the latter situation. Volume loss of the tendon is absent. Extensive intra-substance tears may either represent or be precursors of a more extensive delamination tear. The presence of a well-defined anechoic cyst within the rotator cuff is usually associated with a supraspinatus articular-side tear.
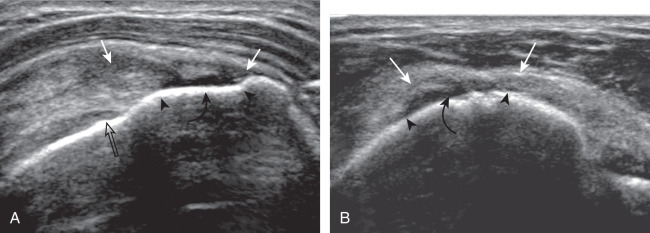
Full-Thickness Tear
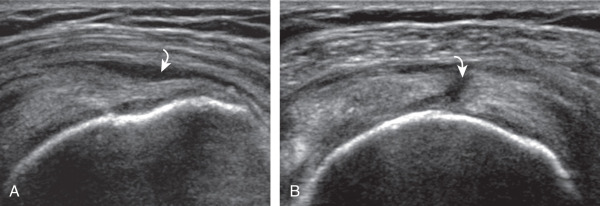
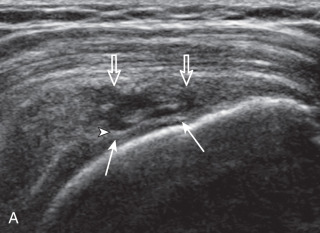
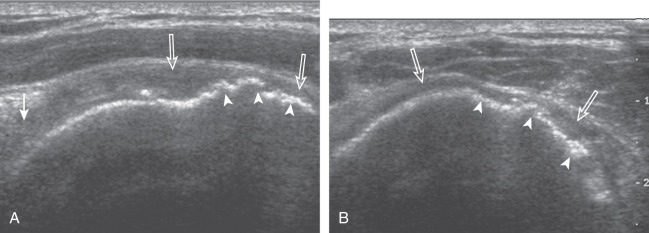
A full-thickness supraspinatus tendon tear is characterized by a well-defined hypoechoic or anechoic defect that disrupts the hyperechoic tendon fibers and extends from the articular to bursal surfaces of the tendon ( Figs. 3.30, 3.31, 3.32, 3.33, 3.34, 3.35, 3.36, 3.37, and 3.38 ). Identification of a hyperechoic interface between the hypoechoic hyaline cartilage and anechoic or hypoechoic tendon tear (cartilage interface sign) assists in the identification of the articular extent. This finding is only seen when the sound beam is perpendicular to the hyaline cartilage; the heel-toe maneuver when imaging the tendon in long axis and toggling the transducer while in short axis is helpful (see Chapter 1 ). Small full-thickness tears may not be associated with volume loss of the tendon, especially if filled with fluid. Narrow longitudinal tears are best visualized with the tendon in short axis ( Fig. 3.31 ). As a tear becomes larger, flattening or concavity of the superior supraspinatus tendon surface with volume loss is typical ( and ). Acute tears may occur more proximally, and more commonly are filled with anechoic fluid ( Fig. 3.33 ). An acute tear in a patient younger than 40 years or a proximal tear does not demonstrate cortical irregularity, although these types of tears are less common. When a tendon tear is identified, one should describe the location of the tendon tear, the dimensions of the tear in long axis and short axis, and extension to other adjacent tendons. A full-thickness tear that is small may be termed a focal or incomplete full-thickness tear , whereas a tear that involves the entire width of a tendon may be termed a complete or full-width full-thickness tear . Chronic tears may be associated with extensive remodeling of the greater tuberosity, and the distal torn tendon may be tapered without adjacent fluid but possibly with isoechoic or hyperechoic synovial hypertrophy ( Fig. 3.37 ). To determine if a supraspinatus tear involves the adjacent infraspinatus, knowledge of the greater tuberosity anatomy and tendon attachments is helpful (see Fig. 3.2 ). When imaging the cuff in short axis over the greater tuberosity, a tear that extends over the posterior aspect of the middle facet indicates infraspinatus involvement as well. A supraspinatus tendon tear may also extend anteriorly through the rotator interval to involve the cephalad fibers of the subscapularis tendon (see Subscapularis Tears and Tendinosis ). A biceps reflection pulley tear and long head of biceps brachii tendon subluxation or dislocation may also occur in this situation ( Fig. 3.39 ) ( and ). The supraspinatus and infraspinatus muscles should be assessed for fatty infiltration and atrophy in the setting of a rotator cuff tear as this finding is associated with poor surgical outcome after repair (see Rotator Cuff Atrophy ).
Tendinosis
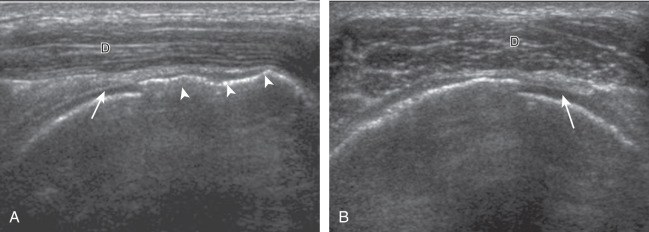
The term tendinosis is used rather than tendinitis because active inflammatory cells are absent. Instead, a degenerative process is present with eosinophilic, fibrillar, and mucoid degeneration and possible chondroid metaplasia. At ultrasound, focal tendinosis is characterized by a heterogeneous, somewhat ill-defined, hypoechoic area in the tendon without a defined tendon defect ( Fig. 3.40 ). Tendinosis must be differentiated from anisotropy as both may appear hypoechoic (see Fig. 3.11 ). Unlike tendon tear, tendinosis is usually less defined, it may be associated with increased tendon thickness, and it is usually not associated with adjacent cortical irregularity of the greater tuberosity. Diffuse tendinosis may cause the entire tendon to appear hypoechoic, nearly equal in echogenicity to adjacent muscle ( Fig. 3.41 ). Unlike a massive tendon tear, a normal convex superior surface of the supraspinatus is still seen with tendinosis.
Indirect Signs of Supraspinatus Tendon Tear
Tendon Thinning.
Thinning or volume loss of the supraspinatus tendon and flattening or superior concavity of the superior supraspinatus tendon surface typically indicate tendon fiber loss. This condition can be seen with full-thickness tendon tears, especially moderate size or larger (see Figs. 3.30 and 3.38 ), and bursal-sided partial-thickness supraspinatus tendon tears (see Figs. 3.27 and 3.28 ). The presence of tendon thinning helps to exclude tendinosis because this latter condition, in contrast, shows normal or increased tendon thickness (see Figs. 3.40 and 3.41 ).
Cortical Irregularity.
When there is cortical irregularity of the greater tuberosity immediately adjacent to a defined hypoechoic or anechoic tendon abnormality of the supraspinatus, this increases the likelihood that the tendon abnormality represents a tear (see Figs. 3.21 and 3.22 ). Therefore, if greater tuberosity cortical irregularity at the supraspinatus footprint is identified during scanning, special attention should be paid to this area. This finding is also helpful in the differentiation between tendon tear and tendinosis because both may appear as a hypoechoic tendon abnormality. With tendinosis, the hyperechoic greater tuberosity surface is typically smooth, as in the normal state (see Fig. 3.41 ). In fact, cortical irregularity of the supraspinatus footprint on radiography is associated with a rotator cuff tear in 75% of cases, while lack of cortical irregularity is associated with normal rotator cuff in 96%. Cortical irregularity is common with chronic attrition tears of the supraspinatus, but it may be absent with an acute tendon tear in a younger individual or with proximal tears (see Fig. 3.33 ). The significance of greater tuberosity cortical irregularity is specific to the attachment of the supraspinatus tendon. Cortical irregularity of the posterior aspect of the humerus involving the bare area (an area of intra-articular cortex without hyaline cartilage) beneath the infraspinatus tendon is a common finding, possibly a normal variant, and is usually without significance. However, if cortical irregularity at this site is extensive, this too can be associated with articular surface partial-thickness infraspinatus tendon tear and posterior labral tear in the setting of posterosuperior impingement syndrome. Finally, cortical irregularity of the lesser tuberosity of the subscapularis tendon insertion is also a common finding and is of little clinical significance in the absence of an adjacent tendon abnormality.
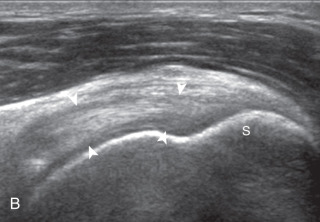
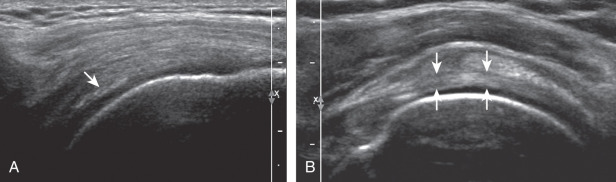
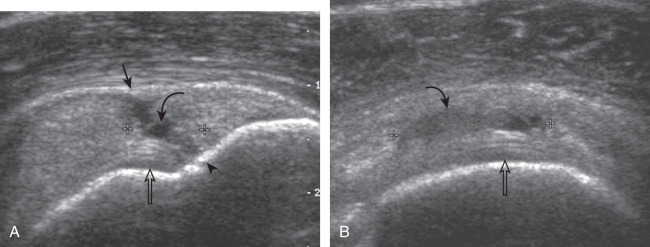
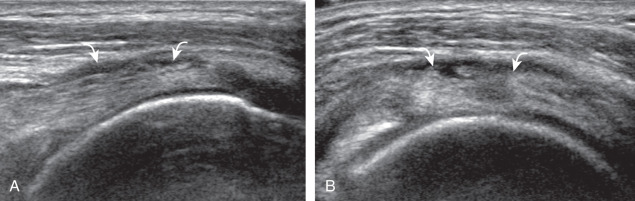
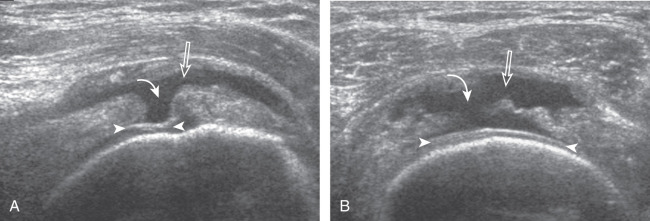
Joint Effusion and Bursal Fluid.
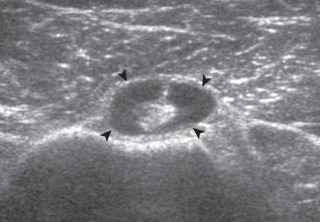
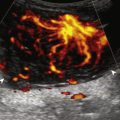
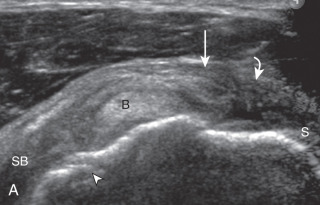
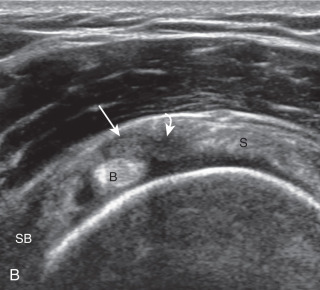
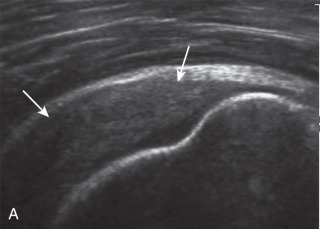
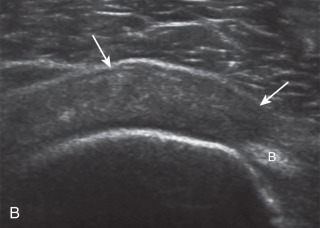
Investigators have shown that the findings of both glenohumeral joint effusion and subacromial-subdeltoid fluid suggest rotator cuff tear with a positive predictive value of 95%. To diagnose joint effusion, the long head of the biceps brachii tendon is evaluated in the bicipital groove for surrounding anechoic fluid ( Fig. 3.42 ). The long head of the biceps brachii tendon sheath normally communicates with the glenohumeral joint, so increased joint fluid will collect in this extension of the joint. A tiny sliver of fluid at one side of the biceps tendon is often seen normally, but fluid greater than this is considered abnormal, especially if it is seen circumferential to the biceps tendon. With regard to the posterior glenohumeral joint recess, small effusions may only be visible with the shoulder in external rotation ( ). With larger joint effusions, fluid in the posterior shoulder joint recess can be seen even in neutral position deep to the infraspinatus tendon ( Fig. 3.43 ). Subacromial-subdeltoid bursal fluid is diagnosed when the hyperechoic walls of the bursa are separated by more than 1 or 2 mm of anechoic fluid. Both distention of the biceps brachii long head tendon sheath and the subacromial-subdeltoid bursa may be seen over the anterior shoulder ( Fig. 3.44 ) ( ). Bursal fluid may also collect dependently, so the most inferior aspect of the bursa should also be evaluated to visualize small quantities of fluid (see Fig. 3.16C ). Although simple joint and bursal fluid is commonly anechoic, complex fluid may appear hypoechoic or even isoechoic to adjacent muscle tissue.