The number of adults with congenital heart disease living in the United States is estimated to be at least 1.4 million, and at least 300,000 of these people have complex forms of congenital heart disease. The majority of these patients have undergone surgical repairs in childhood, and lifelong follow-up is recommended. Many adults with congenital heart disease do not recognize subtle changes in exercise capacity and serial imaging of adults with congenital heart disease is important to monitor for hemodynamic and anatomic sequelae. Cardiovascular magnetic resonance (CMR) imaging has become an attractive imaging modality for surveillance of the long-term cardiac complications in this population because of its excellent tissue border delineation, tissue characterization, and quantification of biventricular volumes and valvular regurgitation. CMR allows for serial comparisons without the need for ionizing radiation or iodinated contrast. The objective of this chapter is to review select congenital heart disease diagnoses that are referred for CMR imaging. For each congenital heart disease condition, we will present a suggested CMR protocol with the acknowledgement that a there is considerable anatomic variability and individualization of protocols is often required. Knowledge of the patient’s anatomy, surgical interventions, and prior imaging is critical to focus the protocol so that the essential information is obtained within a reasonable amount of time, as many of these adults will undergo serial examinations.
Ebstein Anomaly
Anatomy and Natural History
Ebstein anomaly is a malformation of the tricuspid valve and right ventricle, which encompasses a large spectrum of disease severity. There is failure of delamination of the septal and posterior tricuspid valve leaflets from the myocardium, resulting in apical displacement of the tricuspid valve (≥0.8 cm/m 2 relative to the anterior mitral leaflet insertion site). The portion of the right ventricle proximal to the functional tricuspid valve becomes “atrialized.” The anterior leaflet of the tricuspid valve is large and redundant, and often has fenestrations and tethering attachments to the right ventricular (RV) free wall. The posterior leaflet is often dysplastic and atrially displaced.
The etiology of Ebstein anomaly is not known; however, in rare cases, genetic factors such as mutations in the transcription factor NKX2.5,10p13–p14 deletion, or 1p34.3–p36.11 deletion have been described. The most severe cases of Ebstein anomaly result in fetal hydrops and fetal demise. Patients with Ebstein anomaly often develop progressive right heart failure and exercise intolerance. However, some individuals with mild forms of this disease can be asymptomatic into adulthood.
Surgical Repairs
When possible, the surgical intervention for Ebstein anomaly involves tricuspid valve repair. In the current era, the repair generally involves a right atrial (RA) reduction, plication of the atrialized right ventricle and a tricuspid valve repair involving the creation of a monocusp tricuspid valve using the redundant anterior tricuspid valve leaflet with a posterior annuloplasty (cone procedure). In patients who are unsuitable for tricuspid valve repair, a bioprosthetic tricuspid valve replacement is generally performed. Evaluation of the patient after Ebstein repair involves assessing the degree of residual tricuspid regurgitation or stenosis, assessing RA size and the RV size and function. The right coronary artery lies in close proximity to the repaired tricuspid valve annulus site and it is important to assess for evidence of late gadolinium enhancement (LGE) following surgery for Ebstein anomaly.
Cardiovascular Magnetic Resonance Evaluation of Ebstein Anomaly
Tricuspid Valve Anatomy and Tricuspid Regurgitation Fraction
An accurate assessment of the tricuspid valve anatomy, including assessing the leaflet sizes, the subvalvar apparatus, the presence of tethering attachments of the anterior leaflet to the RV free wall, and the location of the tricuspid valve functional annulus, is important for planning repair. Understanding the amount and structure of the tricuspid leaflet tissue provides the surgeon information on whether enough leaflet tissue is accessible to repair, rather than replace, the tricuspid valve.
Balanced steady-state free precession (bSSFP) cine imaging of the tricuspid valve can be performed in the four-chamber view and the RV two-chamber view. It is important to determine the orientation of the tricuspid valve inflow because it may be oriented toward the right ventricular outflow tract (RVOT) or directed at the RV apex; therefore off-axis views are often required. Determining the severity of tricuspid regurgitation may be challenging in patients with Ebstein anomaly but may be quantified with phase contrast CMR (PCMR).
Right Atrial and Right Ventricular Size and Function
Progressive tricuspid regurgitation and abnormal RV myocardium lead to right heart dilation. Measurements of RA and RV volumes are typically performed in axial or short-axis orientation with endocardial contours drawn in end systole and end diastole. When contouring the right ventricle, it can be useful to assess the functional RV size that excludes the atrialized right ventricle and only includes the RV volume distal to the functional tricuspid valve annulus and coaptation point. Many centers will report both the functional RV size and function and the anatomic RV size and function (using the anatomic tricuspid annulus as a landmark). The ability to accurately and reproducibly measure RV volume is important because RV size has been associated with clinical outcomes in patients with Ebstein anomaly. Additionally, mismeasurement of RV stroke volume can result in errors when calculating tricuspid regurgitation severity.
Progressive RV dilation or dysfunction in the setting of severe tricuspid regurgitation is imaging criteria for tricuspid valve surgical intervention. The index of right-sided to left-sided heart volumes derived from CMR has been shown to correlate well with other established markers of heart failure. Contouring the end-diastolic volume measurements of the right ventricle, RA, left ventricle, and left atrium (LA) can provide a total right/left-volume index ( Fig. 41.1 ):
Total right/left-volume index=(right atrium+atrialized right ventricle+functional right ventricle)/(LA+left ventricle)


Indexes such as these may eventually be used to help guide timing of tricuspid valve intervention.
Associated Cardiac Abnormalities
Patients with Ebstein anomaly commonly have atrial septal defects (ASDs), and may occasionally have RVOT obstruction, or myocardial noncompaction. CMR can be used to assess the morphology of the interatrial septum and to calculate the Qp:Qs ratio by performing PCMR across the aorta and pulmonary artery.
A suggested CMR protocol for adults with Ebstein anomaly is presented in Box 41.1 .
Localizers
Electrocardiogram-gated cine balanced steady-state free precession
- •
Axial stack through the heart and branch pulmonary arteries
- •
Three-chamber right ventricular stack, two-chamber left, four-chamber views
- •
Ventricular short-axis stack from the base to the apex
- •
Right ventricular outflow tract view parallel to the right ventricular outflow tract
- •
Right ventricular two-chamber view
- •
Oblique planes to image tricuspid valve inflow orientation
- •
Oblique sagittal plane to image the atrial septum
- •
Contrast-enhanced three-dimensional magnetic resonance angiogram a
a In general, our practice is to obtain a gadolinium-enhanced three-dimensional magnetic resonance angiogram with the first cardiovascular magnetic resonance (CMR) examination, and then optional for subsequent examinations.
Electrocardiogram-gated phase contrast through-plane flow in the main pulmonary artery, aorta, tricuspid and mitral valves b
b In cases where Qp:Qs ratio is of interest, flow across the branch pulmonary arteries, superior vena cava, and inferior vena cava/descending thoracic aorta may be assessed to improve level of confidence.
Late gadolinium enhancement to assess for myocardial fibrosis c
c In general, our practice is to obtain late gadolinium enhancement (LGE) imaging to assess for myocardial fibrosis with the first CMR examination, and the frequency of repeating this technique in subsequent examinations is dependent on the initial findings and specific condition. For example, some CMR laboratories repeat LGE imaging every 3 years in patients with conotruncal anomalies (tetralogy of Fallot, transposition of the great arteries, double outlet right ventricle).
These protocols were adapted from Boston Children’s Hospital Cardiac Magnetic Resonance Imaging Program.
Coarctation of the Aorta
Anatomy and Natural History
Coarctation of the aorta is typically a fibrous ridge in the aortic isthmus, just distal to the insertion of the left subclavian artery. Although often discrete, aortic coarctation can also be long segment or associated with a diffusely hypoplastic transverse aorta. Aortic coarctation is associated with a diffuse vascular abnormality and is associated with aortic aneurysm, cerebral aneurysms, or endothelial dysfunction. Awareness of these abnormalities is important because the entire aorta and cerebral vessels should be imaged in patients with aortic coarctation.
Aortic coarctation sometimes presents in adulthood as difficult-to-manage systemic hypertension and the diagnosis may be suspected from a murmur, diminished lower extremity pulses, or arm–arm or arm–leg blood pressure discrepancy. Those who had an aortic coarctation repair early in life have up to a 5% risk of re-coarctation in adulthood and present similarly.
Surgical Repairs
There are several types of surgical repairs for native aortic coarctation, and they are dictated by the anatomy. For patients with a discrete coarctation, an end-to-end anastomosis is performed. If there is associated transverse aortic arch hypoplasia, an extended end-to-end procedure may be required.
Some patients with complex aortic coarctation have undergone interposition graft repairs, and those with Dacron material are particularly susceptible to aneurysm formation. The subclavian flap procedure was performed in the early surgical experience, and involved transecting the left subclavian artery and placing it over the narrowed portion of the descending aorta. Patients who have undergone this procedure will no longer have the left subclavian artery attached to the transverse arch.
Cardiovascular Magnetic Resonance Evaluation of Aortic Coarctation
Aortic Arch
CMR imaging of native and re-coarctation will be discussed together. The anatomic features of aortic coarctation can be seen with bright-blood cine or double-inversion black-blood spin echo images in the oblique sagittal plane. Gadolinium-enhanced magnetic resonance angiography (MRA) also demonstrates the coarctation ( Fig. 41.2 ) and double oblique reformats can be used to measure the minimal luminal diameter and the reference vessel size. If collateral vessels are seen on contrast-enhanced (CE) MRA or PCMR demonstrates flow augmentation in the descending aorta, the obstruction is probably hemodynamically important. A prolonged deceleration time of the systolic flow in the distal descending thoracic aorta also indicates hemodynamically significant aortic coarctation.

Four-dimensional velocity mapping is not widely available but is an emerging technique to show turbulence at the coarctation site, and characterize altered aortic velocity profiles, providing insight into which patients may be at higher risk for aortic wall complications, such as dissection.
Patients with aortic coarctation are prone to aneurysms in the ascending aorta, cerebral vasculature, and at the site of surgical repair. Aneurysms at the site of previous Dacron patch repair are particularly prone to rupture and should be managed aggressively. Screening for cerebral aneurysms is recommended, although neither optimal management nor frequency of surveillance is well defined.
Left Ventricular Cavity Size and Function
Patients with native or re-coarctation are predisposed to systemic hypertension, particularly exercise-induced hypertension. Therefore standard measurements of left ventricular (LV) mass and function should be performed.
Associated Cardiac Lesions
Over 50% of those with aortic coarctation have a bicommissural aortic valve and these patients are at greater risk for ascending aortic aneurysms. Patients may also have subaortic stenosis, mitral valve abnormalities (e.g., parachute mitral valve and/or mitral stenosis) or ventricular septal defect (VSD).
A suggested CMR protocol for adults with aortic coarctation is presented in Box 41.2 .
Localizers
Electrocardiogram-gated cine balanced steady-state free precession
- •
Four-chamber view, left ventricular two-chamber and, left ventricular long-axis view to the aorta
- •
Ventricular short-axis stack from the base to the apex
- •
Oblique sagittal view of the aortic arch (“candy-cane” view)
- •
Consider double-inversion recovery black-blood images in the oblique sagittal plane if artifact on balanced steady-state free precession imaging
Contrast-enhanced three-dimensional magnetic resonance angiogram in sagittal orientation with first acquisition timed to the aorta a
a In general, our practice is to obtain a gadolinium-enhanced three-dimensional magnetic resonance angiogram with the first cardiovascular magnetic resonance (CMR) examination, and then optional for subsequent examinations.
Electrocardiogram-gated phase contrast through-plane flow in the main pulmonary artery, aorta and consider proximal descending aorta proximal to the coarctation (distal to left subclavian artery) and descending aorta at the level of the diaphragm
Late gadolinium enhancement to assess for myocardial fibrosis b
b In general, our practice is to obtain late gadolinium enhancement (LGE) imaging to assess for myocardial fibrosis with the first CMR examination, and the frequency of repeating this technique in subsequent examinations is dependent on the initial findings and specific condition. For example, some CMR laboratories repeat LGE imaging every 3 years in patients with conotruncal anomalies (tetralogy of Fallot, transposition of the great arteries, double outlet right ventricle).
These protocols were adapted from Boston Children’s Hospital Cardiac Magnetic Resonance Imaging Program.
Tetralogy of Fallot
Anatomy and Natural History
Evaluation of patients with repaired tetralogy of Fallot (TOF) is one of the most common adult congenital heart disease diagnoses referred for CMR. TOF represents the most common form of cyanotic congenital heart disease affecting up to 0.5 per 1000 live births. Survival following TOF repair is excellent, but there is a 3-fold increase in mortality beginning in the third postoperative decade of life, and 14% of patients develop markedly impaired functional status late after surgical repair, highlighting the importance of regular surveillance of these patients. This congenital anomaly results from the anterior deviation of the conal septum, resulting in varying degrees of RVOT obstruction, VSD, an overriding aorta, and RV hypertrophy. Importantly, the degree of RVOT obstruction can range from only mild subpulmonary stenosis to the most severe form involving complete absence of the main pulmonary artery (TOF/pulmonary atresia), which occurs in approximately 15% of patients with TOF.
Surgical Repairs
In the current era, the majority of patients undergo surgical repair in infancy or childhood, although older adults may have first undergone a palliative shunt (Blalock-Taussig, Waterston, or Potts shunt) as a young child and then undergone a complete repair at an older age. Strategies to repair TOF have evolved over time. The early experience involved placing a transannular patch to eliminate the RVOT obstruction; however, current strategies have been modified to alleviate most of the RVOT obstruction while trying to preserve some of the integrity of the pulmonary valve. Patients with TOF/pulmonary atresia and those with anomalous left coronary artery from the right sinus may undergo an RV-to-pulmonary artery (RV-PA) conduit. Knowledge of the patient’s surgical history before CMR is ideal because it will determine the specific CMR protocol to employ, focusing on the potential residual lesions.
Many patients with repaired TOF undergo a pulmonary valve replacement in adulthood. CMR is increasingly being used to aid in the decision making of timing of these interventions. Box 41.3 lists suggested imaging criteria for consideration of pulmonary valve replacement in asymptomatic patients with severe pulmonary regurgitation (PR).
- •
Right ventricular end-diastolic volume index >150 mL/m 2 or Z-score >4. In patients whose body surface area falls outside published normal data: right ventricle/left ventricle end-diastolic volume ratio >2
- •
Right ventricular end-systolic volume index >80 mL/m 2
- •
Right ventricular ejection fraction <47%
- •
Left ventricle ejection fraction <55%
- •
Large right ventricular outflow tract aneurysm
- •
Other significant hemodynamic abnormalities:
- •
Right ventricular outflow tract obstruction with right ventricular systolic pressure >2/3 systemic
- •
Severe branch pulmonary artery stenosis (<30% flow to affected lung)
- •
More than moderate tricuspid regurgitation
- •
- •
Left-to-right shunt from residual ventricular or atrial septal defect with pulmonary to aortic flow ratio >1.5
- •
Severe aortic regurgitation
- •
Severe aortic root dilation (>5 cm)
Cardiovascular Magnetic Resonance Evaluation of Tetralogy of Fallot Repair
Right Ventricular Outflow Tract Obstruction and Pulmonary Arteries
A goal of TOF surgery is to relieve the RVOT obstruction, yet many patients are left with varying degrees of obstruction that may be located in the subpulmonary area, at the level of the pulmonary valve, or more distally in the main or branch pulmonary arteries (PA). Transannular patch repairs can result in RVOT regional wall motion abnormalities and aneurysms ( Fig. 41.3 ). RVOT aneurysms are not only associated with decreased RV ejection fraction (EF) but are also associated with unfavorable ventricular interactions, resulting in a reduced LVEF.

Visualization of the entire RVOT is important using specific RVOT long-axis ( Fig. 41.4A ) and two-chamber RV cine views ( Fig. 41.4B ). The RV two-chamber view allows visualization of the right atrium, tricuspid valve, RV, and main pulmonary artery all in one plane. Assessing for downstream stenosis in the branch pulmonary arteries can be performed with either a bSSFP stack in an axial plane or an MRA.


Newer catheter-based pulmonary valves are promising developments for patients with congenital heart disease affecting the right heart. At the current time, most percutaneous valves are placed inside existing RV-PA conduits or dysfunctional bioprosthetic valves. CMR is useful to determine the geometry of the RVOT and identify potential candidates for percutaneous pulmonary valve placement. Delineation of the coronary artery course is essential before any RVOT intervention because 5% to 7% of patients with TOF have an anomalous left coronary artery that may course across the RVOT which can complicate both surgical or transcatheter pulmonic valve implantation. Cardiac and respiratory-gated MRA images have sufficient spatial resolution to assess the origins and proximal coronary artery courses.
Pulmonary Regurgitation
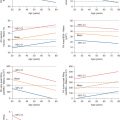
Pulmonary regurgitation is the most common sequelae of TOF repair and is often associated with RV dilation ( Fig. 41.5 ), predisposing to RV dysfunction, arrhythmias, and death. PCMR sequences assess antegrade and retrograde flow across the main pulmonary artery ( Fig. 41.6 ), and studies demonstrate this to be a highly reproducible technique for quantifying pulmonary regurgitation volume. Pulmonary regurgitation fraction is calculated as retrograde flow volume divided by antegrade flow volume and, in our laboratory, a pulmonary regurgitation fraction greater than 40% is considered severe.




Right Ventricular Size and Function
Accurate quantification of RV size, function, and mass is particularly important in repaired TOF patients because RV dilatation, dysfunction, and hypertrophy are associated with adverse outcomes in this group. Pulmonary valve replacement usually eliminates significant pulmonary regurgitation; however, optimal timing of pulmonic valve replacement to prevent the adverse sequelae of RV dilation and dysfunction remains unclear. Pulmonic valve replacement usually results in dramatic decreases in RV volumes and improvement in functional status, but studies have demonstrated that RV systolic function generally remains unchanged.
CMR is the gold standard for quantifying RV size and function in patients with repaired TOF and results in significantly better interobserver variability than transthoracic echocardiography (TTE). LV dysfunction is present in >20% of adults with TOF repair, particularly those who were repaired later in life, had prior palliative shunts, or concomitant RV dysfunction. LV dysfunction has been associated with sudden cardiac death in this patient population.
Tricuspid Regurgitation
There are several mechanisms that lead to tricuspid regurgitation in repaired TOF patients, including annular dilation, structural valve abnormalities, or as a consequence of valve disruption during prior TOF repair. CMR allows for quantification of tricuspid regurgitation, and significant tricuspid regurgitation should be considered in surgical plans at the time of pulmonic valve replacement.
Ascending Aorta
Ascending aortic dilation is common in adults with repaired TOF. However, despite large aortic dimensions, aortic dissection is exceedingly rare. In fact, up to 25% of adults with repaired TOF have an aortic root diameter >4 cm; however, only 2.3% have an aortic diameter >5 cm. Some patients develop progressive dilation of the aortic root that can lead to significant aortic regurgitation.
Myocardial Fibrosis
LGE occurs commonly in locations of prior surgery (RVOT, VSD patch). Repaired TOF patients with greater degrees of LGE are at a higher risk of sustained symptomatic arrhythmia; however, it is unclear if LGE is associated with increased mortality in this patient population. LGE in the area of the VSD patch, RVOT patch, or septal insertion sites are not associated with worse outcomes. Novel techniques such as T1 mapping (see Chapter 2 ), which acts as a marker for diffuse fibrosis, may also prove to act as prognostic indicators in patients with TOF; however, T1 mapping in the RV can be difficult, and definitive studies are lacking.
A suggested CMR protocol for adults after TOF repair is presented in Box 41.4 .
Localizers
Electrocardiogram-gated cine balanced steady-state free precession
- •
Four-chamber view and two-chamber left ventricular, right ventricular views
- •
Ventricular short-axis stack from the base to the apex
- •
Right ventricular outflow tract outflow view parallel to the right ventricular outflow tract, then a second view orthogonal to the first right ventricular outflow tract view, right ventricular outflow tract short-axis view
- •
Axial stack to assess for branch pulmonary arteries and outflow tracts
- •
Three-dimensional contrast-enhanced magnetic resonance angiogram a
a In general, our practice is to obtain a gadolinium-enhanced three-dimensional magnetic resonance angiogram with the first cardiovascular magnetic resonance (CMR) examination, and then optional for subsequent examinations.
Electrocardiogram-gated phase contrast through-plane flow in the main pulmonary artery, aorta, atrioventricular valves b
b In cases where Qp:Qs ratio is of interest, flow across the branch pulmonary arteries, superior vena cava, and inferior vena cava/descending thoracic aorta may be assessed to improve level of confidence.
Late gadolinium enhancement to assess for myocardial fibrosis c
c In general, our practice is to obtain late gadolinium enhancement (LGE) imaging to assess for myocardial fibrosis with the first CMR examination, and the frequency of repeating this technique in subsequent examinations is dependent on the initial findings and specific condition. For example, some CMR laboratories repeat LGE imaging every 3 years in patients with conotruncal anomalies (tetralogy of Fallot, transposition of the great arteries, double outlet right ventricle).
Consider coronary artery imaging with electrocardiogram and respiratory navigator gated three-dimensional balanced steady-state free precession
Consider T1 mapping to assess for diffuse fibrosis
These protocols were adapted from Boston Children’s Hospital Cardiac Magnetic Resonance Imaging Program.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree