This article describes the computed tomography and MR imaging features of the neoplasms of the sinonasal space. Although a pathologic diagnosis may not always be possible, knowledge of the features may help in narrowing down the differentials and establishing a malignant pathology.
Key points
- •
Diverse tissue types in the sinonasal space give rise to a variety of tumors, most of which are malignant.
- •
Although pathologic diagnosis is not always possible, knowledge of the computed tomography (CT) and MR imaging features of individual is required to arrive at a working differential.
- •
Certain tumors behave in typical fashion. Hence, the review areas for these lesions need to be closely examined for proper staging.
- •
CT and MR imaging done together may give better overall information for staging and treatment.
Introduction
Sinonasal tumors are rare. Malignant lesions are more common than benign ones and prognosis is grave. A wide variety of lesions are possible. It is unlikely that CT and MR imaging would provide a pathologic diagnosis in most cases. Role of imaging is to:
- 1.
Narrow down the imaging differential;
- 2.
Distinguish benign from malignant lesions; and
- 3.
Map the entire extent of a tumor with relations to adjacent vital structures and nerves.
This article describes the radiologic features of benign and malignant sinonasal tumors.
Benign and malignant epithelial tumors
Papilloma
The ectodermally derived Schneiderian mucosa gives rise to 3 types of benign neoplastic papillomas in the sinonasal tract:
- 1.
Fungiform or exophytic papillomas;
- 2.
Inverted papillomas (IP); and
- 3.
Oncocytic papillomas.
Overall, neoplastic papillomas constitute only 0.4% to 4.7 % of all sinonasal tumors. The fungiform and IP are commoner and some of their characteristics are summarized in Box 1 :
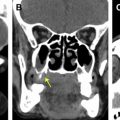
Imaging Features ( Fig. 1 )
- •
Nonspecific, small polypoid lesions to large masses with significant enhancement.

Fig. 1
Inverted papilloma. Classical convoluted cerebriform pattern is seen in the mass involving right maxillary antrum and nasal cavity ( yellow arrow ), both in T2-weighted imaging ( A ) and in postgadolinium T1-weighted imaging ( B ). Widening of maxillary ostium ( red arrow ) is noted in the coronal computed tomography (CT; C ). Presence of areas of necrosis ( yellow arrowheads in D : axial postgadolinium T1-weighted imaging), bone destruction ( red arrowhead in E : axial CT scan image), and extrasinonasal extension ( white arrowhead in D ) indicate malignant transformation.
- •
Expansion and remodeling of the nasal cavity with bowing of adjacent bony walls.
- •
Thinning, sclerosis, intratumoral bony fragments.
- •
Cerebriform or convoluted pattern in diffuse or partial form on T2-weighted images and contrast enhanced T1-weighted images.
- •
Origin of IP is a focal bony hyperostosis seen on computed tomography (CT). Drilling and resection of this area leads to reduced rates of recurrence. Recurrence rates vary from 4% to 22%.
| Type | Age (y) | Sex | Site of Origin | Malignant Potential | Incidence (%) |
|---|---|---|---|---|---|
| Fungiform | 20–50 | More common in males | Nasal septum | No | 50 |
| Inverted | 40–70 | More common in males | Lateral nasal wall near maxillary sinus, characteristic feature is extension into sinuses | Yes (2%–53%) | 47 |
| Oncocytic | 40–70 | More common in males | Lateral nasal wall | Yes (15%) | 3 |
Both synchronous and metachronous malignant change can occur in IP leading to squamous cell carcinoma ( Box 2 ). Dynamic contrast enhanced MR imaging has been shown to be useful in differentiating IP from malignant sinonasal tumors. Malignant change is also possible in oncocytic papillomas.
- •
Partial cerebriform pattern.
- •
Destructive bony changes.
- •
Necrosis.
- •
Extrasinonasal extension.
Squamous Carcinomas and Adenocarcinomas
Squamous cell carcinoma and adenocarcinoma of the sinonasal space are uncommon. The maxillary antrum is most commonly involved ( Fig. 2 ). Radiologic features are generally nonspecific for the carcinomas.

Squamous cell carcinomas are the commonest, accounting for 80% of all sinonasal tumors. They are a disease of elderly (6th to 7th decades) males.
Imaging Features ( Fig. 3 ).
- •

Fig. 3
Squamous cell carcinoma. Destructive mass with intermediate signal in T2-weighted imaging ( A ) and heterogeneous contrast enhancement ( B ) is seen in right maxillary sinus, with extrasinonasal spread to the pterygopalatine fossa, infratemporal fossa, and pterygoid muscles. Destruction of walls of maxillary sinus is seen in a corresponding computed tomography image ( C ).
- •
Large soft tissue mass with heterogeneous enhancement, necrosis, and bone destruction. Invasion of adjoining compartments.
- •
Intermediate signal on T2-weighted imaging.
- •
Perineural spread.
- •
Less than 15% show nodal disease at presentation despite locally advanced disease.
Adenocarcinomas are of intestinal and nonintestinal variety and occur in the fifth to 6th decades of life. The intestinal type may be occupation related or sporadic. The ones that are occupation related occur more in males and are associated with wood and leather dust inhalation. The latent period is of several decades and the risk for woodworkers is increased by 900 times. Because inhalation is the route of insult, ethmoidal region and nasal vault are the common sites. Early onset of clinical features at these sites leads to better prognosis. The sporadic forms are common in women and maxillary sinus is frequently involved. They present late and prognosis is poor.
Imaging Features
- •
Site: occupation related: nasal vault and ethmoid sinus.
- •
Site: sporadic: maxillary sinus.
- •
Large soft tissue mass with or without bony destruction, nonspecific.
- •
Intermediate signal on T2-weighted imaging.
- •
Mucous producing; the mucous causes mixed solid and fluid signals. Diffusion-weighted and contrast images help to differentiate from inspissated collection in adjacent blocked sinus.
Staging of carcinomas are site specific according to the American Joint Committee on Cancer (AJCC) staging system manual 7th edition published in 2010. Separate staging systems exist for maxillary sinus ( Box 3 ) and nasoethmoidal region. Owing to rarity, frontal and sphenoid sinus carcinomas do not have a staging system.
| Stage | Description |
|---|---|
| Tis | Carcinoma in situ |
| T1 | Carcinoma limited to mucous lining |
| T2 | Bone erosion or destruction limited to the hard palate and middle meatus |
| T3 | Bone erosion or destruction of the posterior wall of maxillary sinus, floor and medial wall of orbit; tumor growth into the pterygoid fossa or ethmoid sinus |
| T4a | Tumor growth into the anterior orbit, pterygoid plates, infratemporal fossa, cribriform plate, frontal sinus, sphenoid sinus, or skin of cheek |
| T4b | Tumor growth into the orbital apex, dura, brain, middle cranial fossa, cranial nerves other than V2, nasopharynx and clivus |
Nasal and ethmoidal carcinomas are staged together in the AJCC staging system ( Box 4 ). Primary lesions as well as secondary extensions are seen in the ethmoidal sinuses. The nasoethmoid lesions are subdivided into several subsites for the benefit of staging. The 2 sides of the ethmoid sinus are taken as 2 subsites separated by the perpendicular plate of the ethmoid, which is a part of the nasal septum. The septum, floor, lateral wall, and vestibule are the 4 subsites proposed in the nasal cavity.
| Stage | Description |
|---|---|
| Tis | Carcinoma in situ |
| T1 | Tumor restricted to a single subsite, with or without bone erosion |
| T2 | Tumor involving 2 subsites in a single region within the nasoethmoidal complex, with or without bone erosion |
| T3 | Tumor invades medial wall or floor of orbit, maxillary sinus, palate or cribriform plate |
| T4a | Tumor growth into the anterior orbit, skin of nose or cheek, minimal invasion onto anterior cranial fossa, pterygoid plates, sphenoid or frontal sinuses |
| T4b | Tumor invades any of the following: orbital apex, dura, brain, middle cranial fossa, cranial nerves other than V2, nasopharynx or clivus |
Salivary Gland Neoplasms
There are many minor salivary glands in the sinonasal tract and palate. The most common benign salivary gland neoplasm of the sinonasal space is pleomorphic adenoma.
Imaging Features
- •
Site: nasal septum and lateral nasal wall, maxillary sinus.
- •
Spherical, bone remodeling.
- •
Cellular tumors, intermediate signals on T2-weighted imaging.
Adenoid cystic carcinomas are, overall, the most common salivary gland neoplasm in the sinonasal space. Common in the fifth decade of life, they are slow growing, with a propensity to recur after a long latent period. Recurrence rates are usually in the range of 60%.
Imaging Features ( Figs. 4 and 5 )
- •
Site: palate with secondary invasion of sinonasal space is commonest. Maxillary antrum, nasal cavity.

Fig. 4
Low-grade adenoid cystic carcinoma. High signal intensity is seen in T2-weighted image ( A ), suggesting a low grade tumor. T1-weighted image ( B ) shows hypointense mass with heterogeneous enhancement in postgadolinium image ( C ).

Fig. 5
High-grade adenoid cystic carcinoma. Destructive mass with predominant intermediate signal intensity in T2-weighted imaging ( A ) is seen in right maxilla and right nasal cavity. The mass is isointense to muscles in T1-weighted imaging ( B ), shows marked enhancement in postgadolinium T1-weighted imaging ( C ), and extensive bone destruction in axial computed tomography image ( D ).
- •
Low grade: polypoidal, bone remodeling, high signal on T2-weighted imaging (paucicellular).
- •
High grade: locally aggressive, bone destruction, intermediate signal on T2-weighted imaging (highly cellular).
- •
Perineural spread is characteristic; submucosal and subperiosteal spread.
Mucoepidermoid carcinomas and adenocarcinomas not otherwise specified are the other lesions arising from the minor salivary glands in the sinonasal space. They have no specific imaging features and may mimic squamous cell carcinoma.
Neuroendocrine, neuroectodermal, nerve sheath, and neuronal tumors
The spectrum of the neuroendocrine tumors of the sinonasal tract has at 1 end the well-differentiated form, olfactory neuroblastoma (OLNB). At the other end are the undifferentiated forms called the sinonasal undifferentiated carcinomas. Sinonasal neuroendocrine carcinoma is somewhere between the 2 with more carcinomatous features and less differentiation than OLNB. All of these lesions usually affect the superior nasal cavity, ethmoids and nasal fossa.
Olfactory Neuroblastoma
Also called esthesioneuroblastoma, these are rare and account for 2% of all sinonasal tumors. The lesions have a bimodal age incidence occurring in the 2nd and 6th decade with a slight male predilection.
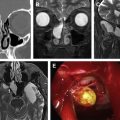
Imaging Features ( Fig. 6 )
- •
Site: olfactory epithelium at roof of ethmoidal sinus and adjoining cribriform plate, upper part of nasal septum, superior turbinates.

Fig. 6
Olfactory neuroblastoma. Sagittal T2-weighted imaging ( A ) and postcontrast coronal ( B ) and sagittal ( C ) T1-weighted imaging in a 3-year-old boy show a lobulated, well-defined, heterogeneously enhancing mass involving both nasal cavities, left ethmoidal air cells, extending into left maxillary antrum, clivus, and with dural involvement ( yellow arrowhead ). Breach of cribriform plate ( white arrowhead ) and intraorbital extension ( red arrowhead ) are seen in coronal T2-weighted imaging ( D ). Destruction of the cribriform plate, nasal septum, left lamina papyracea and orbital floor, and widening of left maxillary ostium are well demonstrated in the coronal computed tomography (CT) image ( E ). Coronal CT scan ( F ) in another 14-year-old boy shows an early tumor demonstrated by filling up of left olfactory recess and ethmoidal air cells ( yellow arrow ).
- •
Large soft tissue mass with intense enhancement.
- •
Intermediate signal on T1-weighted imaging. Hyperintense on T2-weighted imaging.
- •
Calcification, bone destruction, and intracranial and intraorbital extension.
- •
Cysts at interface between brain and tumor.
Craniofacial surgical management is among the preferred modalities in cases of intracranial disease without brain involvement. On imaging, the involvement of the dura needs careful assessment. A small dural postoperative defect can usually be covered by pericranial sheath. If a large dural defect is anticipated, a free flap needs to be harvested. The radiologist needs to alert the surgeon, because free flap harvest is a major undertaking. Staging of OLNB is by the Kadish system and is enumerated in Box 5 . Dulgerov proposed a new staging system for OLNB, which takes in to account the nodal status. This system seems to correlate better with survival and recurrence.
Sinonasal Neuroendocrine Carcinoma and Sinonasal Undifferentiated Carcinoma
The relatively more undifferentiated forms of neuroendocrine carcinomas are classified under sinonasal neuroendocrine carcinoma and sinonasal undifferentiated carcinoma. As the name suggests, sinonasal undifferentiated carcinomas are the most undifferentiated and aggressive form. These lesions have a slight male preponderance and are seen in the fifth and 6th decades of life.
Imaging Features ( Fig. 7 )
- •
Site: upper nasal cavity, ethmoids.

Fig. 7
Sinonasal undifferentiated carcinoma. Coronal T2-weighted imaging ( A ), computed tomography (CT) image ( B ), axial T2-weighted imaging ( C ), and CT scan image ( D ) show a mass ( yellow arrows ) in right anterior ethmoidal air cells and nasal cavity, with bone destruction.
- •
Large soft tissue mass, destruction of sinonasal skeleton, invasion of skull base and orbits. No calcification, unlike OLNB.
- •
Isointense on T1-weighted imaging, isointense to hyperintense on T2-weighted imaging.
- •
Heterogenous enhancement.
- •
May have nodal disease and secondaries at presentation.
Early local recurrence and general aggressiveness are the reasons for poor prognosis of these neoplasms.
Melanoma
The primary malignant melanomas of the sinonasal tract are of the mucosal variety, contrary to the cutaneous ones found elsewhere, which are associated with sun exposure. The precursor melanocytes of the nasal mucosa migrate from the neural crest during embryologic development. The other sites for the development of the primary malignant mucosal melanomas (PMMM) are upper aerodigestive tract, anorectal region, and genitourinary tract.
PMMM are rare and account for only 3.5% of all sinonasal malignancies. They carry a grave prognosis with 40% presenting with nodal disease at diagnosis. The 5-year survival varies between 25% and 40%. Local recurrence is up to 64% in 1 year after surgery. Distant metastasis is also a common cause for treatment failure. Most of the sinonasal PMMM are melanotic; however, 10% to 30% can be amelanotic as well.
Imaging Features ( Fig. 8 )
- •
Site: mucocutaneous junction of the anterior nasal septum, lateral nasal wall, inferior turbinate and maxillary sinus.

Fig. 8
Sinonasal malignant melanoma. Axial T2-weighted ( A ) and postgadolinium T1-weighted ( B ) MR images show a homogeneously enhancing soft tissue mass arising from the anterior right nasal cavity. Axial computed tomography (CT) in the same patient ( C ) shows bone remodeling ( yellow arrow ). CT scan in another patient with melanoma ( D ) shows bone destruction ( yellow arrowhead ).
- •
Polypoidal with well-defined margins. Bone remodeling or destruction.
- •
Intermediate to hypointense on T2-weighted imaging. Hyperintense on T1-weighted imaging owing to melanin or hemorrhage.
- •
Flow voids, intense enhancement, perineural spread in desmoplastic variety after a period of latency.
The AJCC 7th edition has included PMMM in the TNM classification and staging as a separate chapter. In the new system, the extent and depth of the disease has been taken into account rather than the site, as is the case with other sinonasal tumors. In the new system, there is no T1 or T2 disease and hence no stage I or stage II ( Box 6 ). Nodal disease qualifies the lesion as stage IV in the new system. However, no significant survival benefit was observed using the new classification system.