Abstract
Sirenomelia is characterized by a single lower limb, bilateral renal agenesis, and single umbilical artery contiguous with the aorta. Internal and/or external genitalia anomalies as well as oligo/anhydramnios may also be present. First-trimester ultrasound is likely to be of greater utility in making this diagnosis compared to second-trimester ultrasound. This condition was previously considered lethal because of the associated anomalies, particularly bilateral renal agenesis. However, several case reports now exist of survival past the neonatal period. A key feature to distinguish between sirenomelia and caudal regression syndrome is the anatomy of the umbilical cord. Sirenomelia is a rare disorder (1.5 : 100,000–4.2 : 100,000 births) and is 100–150 times more likely to occur in monozygotic twins versus singletons. This condition is thought to be sporadic in nature, and affected fetuses usually have normal karyotype analysis. Recurrence risk is thought not to be higher than the general population/baseline risk.
Keywords
sirenomelia, vitelline remnant, renal agenesis, mermaid syndrome
Introduction
Sirenomelia is a rare congenital disorder that was previously considered a severe form of caudal regression, although it is currently considered a completely different entity. Also known as the mermaid syndrome , it is characterized by a variable degree of atrophy of the lower limbs, with the resultant appearance of a mermaid tail or fin ( Fig. 144.1 ). Because of the associated anomalies (particularly bilateral renal agenesis), the syndrome is typically considered lethal; however, several case reports now exist of survival to several years of life.

Disorder
Definition
Sirenomelia is characterized by three common findings: a single lower limb, bilateral renal agenesis, and a single umbilical artery contiguous with the aorta. Multiple other severe anomalies may present. Reported associated findings include ambiguous or absent external genitalia, absent internal genitalia, absent bladder, absence of the anus and rectum, and sacral agenesis.
Two methods of classifying sirenomelia have been proposed. The first categorizes cases into three groups based on the number of feet present: symelia apus, symelia unipus, and symelia dipus. Symelia apus is the most common and is characterized by a single lower extremity and absent or rudimentary feet. Symelia unipus shows a single foot with two femurs, tibiae, and fibulae. With symelia dipus both feet are present but are malrotated, thus resembling fins.
The second classification system is based on the presence or absence of bones in the lower limb. Type I sirenomelia has all the bones of the limb present (two femurs, two tibiae, two fibulae). Type II has two femurs and two tibiae but fused fibulae, and in type III the fibulae are completely absent. Types IV and V are both characterized by partially fused femurs and are distinguished by the presence of fused fibulae in type IV and absent fibulae in type V. In type VI, a fused femur and fused tibia are present, and type VII has a fused femur and no tibia.
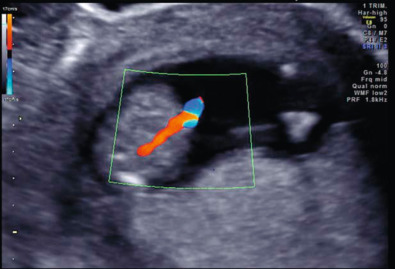
A key feature to distinguish sirenomelia from caudal regression syndrome is the anatomy of the umbilical artery. In sirenomelia, a large artery arises from the aorta and functions as a single umbilical artery ( Fig. 144.2 ). This artery is likely a remnant of the vitelline artery complex and is almost always associated with sirenomelia. In contrast, cases of caudal regression may be distinguished by the presence of two umbilical arteries, nonlethal renal anomalies, and two hypoplastic lower limbs.
Prevalence and Epidemiology
Sirenomelia is a rare disorder, occurring in 1.5 : 100,000–4.2 : 100,000 births. It is 100–150 times more common in monozygotic twins than singletons. The sirenomelia spectrum of defects includes external and internal genital defects. Because of the absence of external genital and infrequent information on gonadal or chromosomal sex, data on sex distribution are very scarce; however, the limited information that is available indicates male sex preference or does not indicate any substantial sex preference.
Sirenomelia is also strongly associated with maternal pregestational diabetes; 2% of reported cases are in diabetic mothers. A recent epidemiologic study by Orioli et al. observed a higher prevalence (2.36 : 100,000) of sirenomelia in the Mexican registry (one of 19 birth defect surveillance systems analyzed worldwide) with an increased prevalence with maternal age less than 20 years. Considering twinning and maternal diabetes are both associated with sirenomelia, and both conditions are more common in older gravidae, the higher prevalence of sirenomelia found in younger mothers in this study was unexpected.
Etiology, Pathophysiology, and Embryology
Although this has been described as “fused lower limbs,” it more likely represents failure of blastogenesis of the lower limb buds. Two theories exist as to the etiology. The first is the vascular steal theory developed by Stevenson et al. This theory posits that blood flow is diverted from the embryo, caudal to the origin of the aberrant vitelline remnant. As a result, tissues distal to this site are either malformed or not formed because of lack of oxygen and nutrients. As the vitelline remnant normally arises superior to the inferior mesenteric and renal arteries, the affected tissues typically include the kidneys, lower intestine, sacrum, and lower extremities. For this theory to be accurate, the vascular steal must occur before day 23 of development, which is before the cleavage of the lower limb bud.
More attention is now being focused on an alternative theory; the concept of primary development field defects. During blastogenesis, the caudal eminence gives rise to the lower limb buds as well as the perineum, somites, and vertebrae. An insult at the caudal neuropore could give rise to the spectrum of anomalies seen in sirenomelia.
Mutations in the superfamily of CYP genes have been noted in animal models (mice) with sirenomelia. Specifically, CYP26A1 is the receptor of retinoic acid, and lower vertebral column malformations have been reported in pregnancies after exposure to high doses of retinoic acid at different gestational ages, linking sirenomelia and retinoic acid intoxication. Another observation is the link between bone morphogenic protein 7 (BMP7) and twisted gastrulation (Tsg); loss of BMP7 combined with a complete loss or half-dose of Tsg in mice models is associated with sirenomelia. These studies have not been replicated in humans.
Sirenomelia is considered to be a sporadic event. Affected fetuses typically have a normal karyotype, and the recurrence risk is not thought to be greater than that of the general population. No instances of familial recurrence of sirenomelia have been reported; however, under the pathogenetic concept of sirenomelia as part of caudal regression syndrome, familial cases are known. Teratogenic exposures may play a role. Animal models demonstrate associations between sirenomelia and exposure to retinoic acid, cadmium, lithium, diethylpropion, lead, hyperthermia, and radiation. In addition, there are case reports of sirenomelia after cocaine use.
Manifestations of Disease
Clinical Presentation
Sirenomelia is characterized by the presence of a single lower limb. Inspection of the umbilical cord will reveal a single umbilical artery, which is connected directly to the aorta. Renal agenesis leads to anhydramnios in utero and a subsequent Potter sequence, resulting in dysmorphic facies and pulmonary hypoplasia. Other severe anomalies are likely to be present. In the lower half of the fetus: ambiguous or absent external genitalia, absent internal genitalia, absent bladder, absence of the anus and rectum, neural tube defect, and sacral agenesis. In addition, upper body/limb malformations have been reported, albeit rarely, and include cardiovascular abnormalities, cleft palate, pulmonary hypoplasia, abdominal wall defects, scoliosis, and other skeletal deformities.
Imaging Technique and Findings
Ultrasound.
Uniquely, sirenomelia may be best diagnosed on a first-trimester ultrasound (US) rather than the second trimester. In the second trimester, amniotic fluid production is reliant on functional kidneys and a normal urinary outflow tract. Renal agenesis is typical with sirenomelia, and the subsequent oligohydramnios or anhydramnios in the second trimester makes a detailed anatomic survey difficult. Consequently, a first-trimester US usually provides more detail in cases where renal agenesis is present.
Several authors report cases of sirenomelia diagnosed in the first trimester, as early as 9 weeks’ gestation. Findings at this time include a thickened nuchal translucency, fused lower extremities ( Fig. 144.3 ), a single umbilical artery contiguous with the aorta (see Fig. 144.2 ), and absent fetal bladder.











