Skeletal “Don’t Touch” Lesions
Clyde A. Helms
Skeletal “don’t touch” lesions are those processes that are so radiographically characteristic that a biopsy or additional diagnostic tests are unnecessary. Not only does the biopsy result in unnecessary morbidity and cost, but in some instances, as is discussed in this chapter, a biopsy can also be frankly misleading and lead to additional unnecessary surgery.
Most radiology training stresses giving a differential diagnosis of a lesion, leaving it up to the clinician to decide between the various entities. For the “don’t touch” lesions, however, a differential list is inappropriate as that often makes the next step in the decision-making process a biopsy. Because these lesions do not need to undergo biopsy for a final diagnosis, a radiologic diagnosis should be made without a list of differential possibilities. These lesions can be classified into three categories: (1) posttraumatic lesions, (2) normal variants, and (3) lesions that are real but obviously benign.
Posttraumatic Lesions
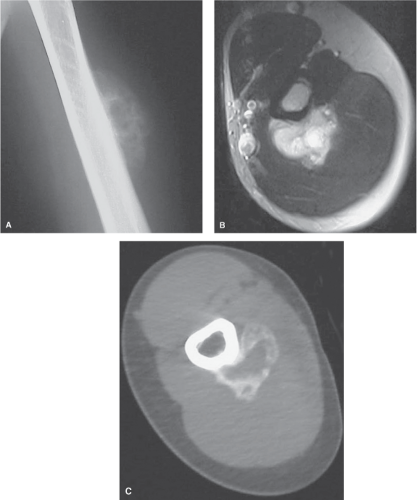
Myositis ossificans is an example of a lesion that should not undergo biopsy because its aggressive histologic appearance can often mimic a sarcoma (1). Unfortunately, radical surgery has been performed based on the histologic appearance of myositis ossificans when the radiologic appearance was diagnostic. The typical radiologic appearance of myositis ossificans is circumferential calcification with a lucent center (Fig. 45.1). This is often best appreciated on a computed tomographic scan. A malignant tumor that mimics myositis ossificans has an ill-defined periphery and a calcified or ossific center (Fig. 45.2). Periosteal reaction can be seen with myositis ossificans or with a tumor. Occasionally, the peripheral calcification of myositis ossificans can be too faint to appreciate; in these cases, a computed tomographic scan should help, or delayed films 1 or 2 weeks later are recommended. Biopsy should be avoided when myositis ossificans is a clinical consideration. MRI can be misleading because the peripheral calcification is not as well seen, and edema in the soft tissues can extend beyond the calcific rim (Fig. 45.3).
Avulsion Injury. Another posttraumatic entity in which a biopsy can be misleading is any avulsion injury (2,3). These injuries can have an aggressive radiographic appearance, but because of their characteristic location at ligament and tendon insertion sites (e.g., anterior-inferior iliac spine or ischial tuberosity), they should be recognized as benign (Figs. 45.4, 45.5). As with myositis ossificans, delayed films of several weeks will usually allow the problem case to become more radiographically clear. Biopsy can lead to the mistaken diagnosis of a sarcoma and should therefore be avoided. Any area undergoing healing can have a high nuclear-to-chromatin ratio and a high mitotic figure count, thereby occasionally simulating a malignancy histologically.
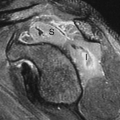
Cortical desmoid is a process on the medial supracondylar ridge of the distal femur that is considered by many to be the result of an avulsion of the adductor magnus muscle. It occasionally simulates an aggressive lesion radiographically, and, histologically, it can look malignant (4). In many instances, biopsy has led to amputation for this benign, radiographically characteristic lesion (Figs. 45.6, 45.7). Cortical desmoids occur only on the posteromedial condyle of the femur. They might or might not be associated with pain and can have increased radionuclide uptake on a bone scan. They might or might not exhibit periosteal new bone and usually occur in young people. Biopsy should be avoided in all cases. Painful cortical desmoids should become asymptomatic with rest. They are often seen as an incidental finding on MRI of the knee and have a characteristic appearance (Fig. 45.8).
Trauma can lead to large, cystic geodes or subchondral cysts near joints and can be mistaken for other lesions, resulting in a biopsy being ordered. Although the biopsy specimen is not likely to mimic a malignant process, it is nevertheless avoidable. Because geodes from degenerative disease almost always are associated with additional findings such as joint space narrowing, sclerosis, and osteophytes, a diagnosis should be made radiographically (Fig. 45.9). On occasion, however, the additional findings are subtle and can be missed (Fig. 45.10). Geodes can also occur in the setting of calcium pyrophosphate dihydrate crystal disease, rheumatoid arthritis, and avascular necrosis (5,6).
Discogenic Vertebral Sclerosis. An entity that is often confused for metastatic disease to the spine is discogenic vertebral disease. It can mimic metastatic disease very closely, and unless the radiologist is familiar with this process, it can lead to an unnecessary biopsy (7). Discogenic vertebral disease most often is sclerotic and focal (Fig. 45.11). It is always adjacent to the endplate, and the associated disc space should be narrow. Osteophytosis is invariably present. It really is a variant of a Schmorl node and should not be confused with
a metastatic focus. On occasion, it can be lytic or even mixed lytic-sclerotic. The typical clinical setting is a middle-aged woman with chronic low back pain. Old films often confirm the benign nature of this process. In the setting of disc space narrowing and osteophytosis, focal sclerosis adjacent to an endplate should not undergo biopsy (8).
a metastatic focus. On occasion, it can be lytic or even mixed lytic-sclerotic. The typical clinical setting is a middle-aged woman with chronic low back pain. Old films often confirm the benign nature of this process. In the setting of disc space narrowing and osteophytosis, focal sclerosis adjacent to an endplate should not undergo biopsy (8).
Fracture. Occasionally, a fracture will be the cause of extensive osteosclerosis and periostitis, which can mimic a primary bone tumor (Fig. 45.12). Lack of immobilization can result in exuberant callus, which can be misinterpreted as aggressive periostitis or even new tumor bone. Results of a biopsy in such a case might resemble a malignant lesion; therefore, any case associated with trauma should be carefully reviewed for a fracture.
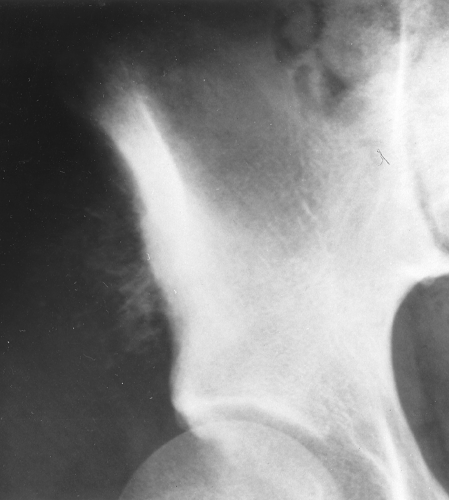
Pseudodislocation of the Humerus. Another traumatic process that can be misdiagnosed radiologically, leading to inappropriate treatment and morbidity, is a pseudodislocation of the humerus (Fig. 45.13). This results from a fracture with hemarthrosis, which causes distension of the joint and migration of the humeral head inferiorly (9). An axial or transscapular view shows it is not anteriorly or posteriorly dislocated (the usual forms of shoulder dislocation) but merely inferiorly subluxated. On an anteroposterior view, it can mimic a posterior dislocation
in that the normal superimposition of the humeral head and the glenoid is missing. Often, attempts are made to “relocate” the humeral head, which, of course, are both fruitless (because it is not dislocated) and painful. A fracture is invariably present, and if not seen on the initial films, it should be sought after with additional views. The transscapular or the axial view is the key to making the diagnosis of a pseudodislocation. If necessary, the joint can be aspirated to confirm the presence of a bloody effusion and to show the normal position of the humeral head when fluid has been removed from the joint.
in that the normal superimposition of the humeral head and the glenoid is missing. Often, attempts are made to “relocate” the humeral head, which, of course, are both fruitless (because it is not dislocated) and painful. A fracture is invariably present, and if not seen on the initial films, it should be sought after with additional views. The transscapular or the axial view is the key to making the diagnosis of a pseudodislocation. If necessary, the joint can be aspirated to confirm the presence of a bloody effusion and to show the normal position of the humeral head when fluid has been removed from the joint.
 Figure 45.4. Avulsion Injury. Cortical irregularity (arrows) at the ischial tuberosity in this patient with pain over this region raises the question of possible tumor. This is a classic appearance, however, for an avulsion injury from this region, and a biopsy should be avoided.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|