| High specificity* |
CMLs Rib fractures, especially posteromedial Scapular fractures Spinous process fractures Sternal fractures |
| Moderate specificity |
Multiple fractures, especially bilateral Fractures of different ages Epiphyseal separations Vertebral body fractures and subluxations Digital fractures Complex skull fractures Pelvic fractures |
| Common but low specificity |
SPNBF Clavicular fractures Long bone shaft fractures Linear skull fractures |
* Highest specificity applies in infants.
The most common fractures in abused children involve the long bones, ribs, and skull. King and associates analyzed 429 fractures in 189 abused children and found that 324 of the 429 fractures (76%) involved the long bones; only 8% each involved the skull and the rib cage (44). Only skull fractures were more common in infants than in children over one year of age. These authors found both rib fractures and distinctive metaphyseal injuries to be substantially less common than fractures of the long bone shafts. Loder and Bookout reported a somewhat different experience with 154 fractures in 75 abused children (47). They found that 49 fractures (32%) involved the skull and 31 (20%) involved the ribs. There were 69 long bone fractures (45%), of which 19 (28%) were described as corner fractures. The average age for the children with corner fractures was 4 months (range: 3 weeks to 8 months), compared with an overall average age of 16 months.
Worlock and colleagues studied 156 fractures in 35 abused infants and children (48). They compared fracture distributions in children below 18 months to those in children above 18 months of age. In the younger group, 60% of fractures involved the rib cage, as opposed to no rib fractures in children over 18 months of age. Skull fractures were found in 11% of the younger group in contrast to 40% in the older group. All metaphyseal lesions occurred in the younger group.
More recent studies of large populations of children with fractures have provided estimates of the incidence of inflicted skeletal injuries and again emphasize the important relationship to patient age. Loder and Feinberg used the US Kids’ Inpatient Database to review the demographic and injury characteristics of 2.5 million hospitalized children and found that 1794 (0.1%) were coded as abuse. Forty-nine percent were less than 1 year and 68% were under 2 years of age (1). There were 1053 fractures in the 1794 abused children (0.6 fractures/child). The number of fractures per child was greatest in infants and diminished sharply in older children (Table 2.2). The distribution of fracture by anatomic region for the younger children was as follows: 0–1 year: lower extremity (33%) > skull (26%) > upper extremity/scapula/clavicle (20%) > ribs/sternum (20%); 1–2 years: skull (31%); upper extremity/scapula/clavicle (31%) > lower extremity (23%) > ribs/sternum (9%).
| Age | |||||
|---|---|---|---|---|---|
| Fracture location | <1 year No. (%) | 1–2 years No. (%) | 3–12 years No. (%) | 13–20 years No. (%) | Total group |
| No. patients | 875 (49) | 345 (19) | 316 (18) | 258 (14) | 1794 |
| Head/torso | 370 | 81 | 16 | 21 | 488 |
| Skull | 202 | 56 | 12 | 19 | 289 |
| Rib/sternum | 159 | 16 | 4 | 1 | 180 |
| Vertebra | 9 | 6 | 0 | 0 | 15 |
| Pelvis | 0 | 3 | 0 | 1 | 4 |
| Upper extremity | 161 | 56 | 22 | 8 | 247 |
| Clavicle/scapula | 35 | 7 | 1 | 0 | 43 |
| Humerus | 74 | 28 | 6 | 3 | 111 |
| Radius/ulna | 51 | 17 | 13 | 2 | 83 |
| Carpal/metacarpal | 1 | 4 | 2 | 3 | 10 |
| Lower extremity | 257 | 41 | 16 | 4 | 318 |
| Femoral neck/femur | 150 | 26 | 12 | 1 | 189 |
| Tibia/fibula/ankle | 98 | 15 | 3 | 3 | 119 |
| Tarsal/metatarsal | 6 | 0 | 1 | 0 | 7 |
| Multiple | 3 | 0 | 0 | 0 | 3 |
| Total fractures | 788 | 178 | 54 | 33 | 1053 |
Leventhal and others also analyzed the data from the US Kids’ Inpatient Database for the years 1997, 2000, and 2003 (26). They found that proportions of cases of children hospitalized with fractures attributable to abuse decreased with increasing age. In 2003, the proportions due to abuse were 24.9% for children less than 12 months of age, 7.2% for children 12–23 months of age, and 2.9% for children 24–35 months of age. In 2003, they found that the incidence of fractures caused by abuse was 15.3 cases per 100,000 children less than 36 months of age. The incidence per 100,000 was 36.1 among children below 12 months of age, 4.8 for children aged 12–23 months, and 4.8 among children aged 24–35 months.
In a single center study, Starling and others reviewed the records of 298 children with fractures seen over a 4-year period by the institutional Child Protection Team (CPT). They found that 194 (65%) were associated with abuse (49). The age ranged from 0 months to 13.9 years, with a median age of 6 months. There were a total of 630 fractures in 194 patients (mean: 2; range: 1–31). Excluding the skull, the sites most commonly fractured were the ribs (50.2%), legs (21.8%), and arms (12.9%). Since the focus of this study was the relationship of the perpetrator to the victim, there was little further detail regarding the fracture location and patterns.
Studies that examine fractures in children less than one year of age show clear trends regarding distribution of fracture types. Skellern and others’ retrospective analysis of 99 children under 1 year of age separated cases into nonaccidental and accidental groups (28). Comparison was made between the two groups for age, sex, and type of fracture. Of the 99 infants with fractures (64 males, 35 female), the skull and femur were the most prevalent sites of injury. Twenty-six infants had fractures assessed as nonaccidental. This group was younger, but did not differ significantly in gender or site of fracture. Infants younger than 4 months had a significantly greater risk of their fracture being nonaccidental (P = 0.0007).
Banaszkiewicz and others retrospectively studied 74 infants (mean: 5 months; range: 2 weeks to 1 year) seen in the Emergency Department (ED) for fractures over a 5-year period (1995–1999) and assessed them for the likelihood of abuse (50). Forty-six had skull fractures and 28 had long bone fractures. Children were classified into one of seven categories: definite abuse, likely abuse, suspicious, likely accident, definite accident, neglect, or unknown cause. A three-tier system of grading for possible abuse was then used to analyze variance. The first tier consisted of the initial assessment by staff clinicians, the second retrospectively by an orthopedic registrar, and the third retrospectively by a designated doctor in child protection (consultant pediatrician), all using the same information from the case notes. The use of the three-tier system of grading demonstrated a variance in the diagnosis of nonaccidental injury. The possibility of abuse was underestimated at the time of the original injury in over a quarter of cases (28.4%) when compared with the assessment by the consultant pediatrician. In 34 children (46%), there was no written documentation that nonaccidental injury was ever considered. While management depends on local guidelines and arrangements, the authors advised that all children under one year of age with a fracture should be admitted to the hospital and referred to a pediatrician for child protection assessment. The American Academy of Pediatrics (AAP) has provided guidance regarding the medical necessity for the hospitalization of possible victims of child abuse (51).
In 2008, Kemp and colleagues published a systematic literature review of 32 published studies in an effort to identify factors which help distinguish abusive from accidental fractures (52). Fractures resulting from abuse were noted throughout the skeletal system, most commonly in infants and toddlers (between 1 and 3 years old). Multiple fractures were more common in cases of abuse. Once major trauma was excluded, rib fractures had the highest probability for abuse (0.71; 95% CI, 0.42–0.91). The probability of abuse in the setting of a humeral fracture was between 0.48 (95 % CI, 0.06–0.94) and 0.54 (95 % CI, 0.20–0.88), depending on the definition of abuse used. Analysis of fracture type showed that supracondylar humeral fractures were less likely to be inflicted. The probability of abuse for femoral fractures was between 0.28 (95 % CI, 0.15–0.44) and 0.43 (95 % CI, 0.32–0.54), depending on the definition of abuse used and the developmental stage of the child. The probability of abuse with skull fracture was 0.30 (95 % CI, 0.19–0.46).
In 2009, Pandya and others published a large single center 10-year retrospective review of 500 cases of abuse in children under 48 months of age and compared them to 985 accident victims (53). They found that abused children were on average younger than accidental trauma patients. In patients less than 18 months of age, the odds a fracture was due to abuse versus an accident was rib – 23.7×; tibia/fibula – 12.8×; humerus – 2.3×; and femur – 1.8×. Interestingly, in the older than 18 months age group, the risk of a fracture being accidental versus abusive was greater for the humerus (3.4×) and femur (3.3×).
In a 2010 study, Leventhal and others used the 2006 Kids’ Inpatient Database and classified accidental and abusive cases with fractures into three groups: (1) skull fractures, (2) skull and nonskull fractures, or (3) nonskull fractures (54). They found that the expected high association of fractures and abuse was demonstrable only for nonskull fractures in infants less than six month of age. In a review of the National Health System hospital episode statistics for children aged 1 week to 5 years admitted in England from 1997 to 2009, Lee and colleagues found a similar high association of abuse and long bone fractures in infants under 6 months, but they suggested that under-reporting of abuse may result in an artificial lowering of abuse cases in older children with less severe injuries (55). The authors advised that the response to high-risk injuries such as intracranial injury (ICI) and long bone fracture in young infants needs to be combined with a public health approach that recognizes that most children with maltreatment-related injury have low risk injuries.
In 2013, Maguire and colleagues revised their methodology and updated their earlier systematic review and meta-analyses (52). Their latest review emphasized the significantly higher probability of abuse when an infant younger than 18 months presents with a femoral fracture versus a child aged 12–48 months (PPV 52.6%, 95% CI, 34.6–70.5 vs. PPV 13.5%, 95% CI, 7.3–19.6). Similarly, they found that a humeral fracture is far more likely to be abusive in origin in a child younger than 18 months versus 12–48 months (PPV 55.4%, 95% CI, 39.2–71.6 vs. PPV 3.3%, 95% CI, 1.3–7.8) (56).
Skeletal surveys (SSs) performed in at-risk populations provide important information about the type and distribution of fractures. Early data derived from rigorous postmortem radiologic/histopathologic studies provide information regarding the prevalence of skeletal injury in infants dying with inflicted injury. Kleinman studied 165 fractures in 31 abused infant fatalities (Fig. 2.1). Excluding skull fractures, 84 (51%) of all fractures involved the rib cage (45). There were 72 (44%) long bone fractures, of which 64 (89%) conformed to the classic metaphyseal lesion (CML) pattern. There were only 8 (5%) long bone shaft fractures. The average age of these 31 infants was 3 months, which is substantially younger than those in earlier studies.
Figure 2.1 Distribution of 164 inflicted fractures in 31 infant fatalities. Single vertebral fracture is not shown. The skull fractures in 13 infants are not included in the analysis. (From Kleinman PK, Marks SC Jr, Richmond JM, Blackbourne BD. Inflicted skeletal injury: a postmortem radiologic–histopathologic study in 31 infants. AJR. 1995;165:647–50.)
The use of the standardized protocols recommended by the American College of Radiology (ACR) and the AAP has yielded recent comparable data regarding the overall prevalence of various fracture patterns in suspected abuse. Barber et al. explored the yield of high-detail SSs in 567 infants (median: 4.4 months; range: 4 days to 12 months) (57). The most common indication for a SS was a recognized fracture (N = 261) (Table 2.3). In 21 instances, incidentally encountered rib fractures prompted the survey. Of these 261 studies, a skull fracture was the indication for the survey in 124 instances, the long bones in 104, clavicle in 11, and the pelvis (possible fracture) in 1.
| Number (%) | ||
|---|---|---|
| Main indication | Cases | Positive SS |
| Skull fracture (with or without associated intracranial injury) | 124 (22) | 13 (10) |
| Clinically suspected and confirmed fracture (excluding skull) | 116 (20) | 31 (27) |
| Clinical features of abuse (bruising, burns, sexual abuse) | 81 (14) | 13 (16) |
| Social concern (including witnessed abuse, neglect, child protection service request) | 71 (13) | 5 (7) |
| Intracranial injury without history of trauma (suspected abusive head trauma) | 70 (12) | 24 (34) |
| Head trauma without skull fracture (including intracranial injury with discrepant mechanism) | 46 (8) | 3 (6) |
| Incidental rib fractures | 21 (3.7) | 21 (100)* |
| Abused sibling | 12 (2) | 2 (17) |
| Follow-up study in patients with initial skeletal survey from an outside hospital | 10 (1.8) | 7 (70) |
| Apparent life-threatening event | 6 (1) | 0 |
| Other (including other concerning medical presentation) | 10 (1.8) | 0 |
* Cases with incidental rib fractures were considered to be positive skeletal survey.
Twenty-one per cent (119/567) of the patients had a positive SS, defined as an initial and/or follow-up study that yielded at least one clinically unsuspected fracture (Table 2.4). This prevalence was higher than the 13% (60/457) reported by Duffy et al. for infants (58) and the 13% (124/930) noted by Karmazyn et al. for children aged less than 2 years (59), but lower than the 23.8% (417/1750) reported in children aged less than 2 years by Lindberg et al. (60) or the 25% (14/56) observed by Day et al. in infants (38).
| Number (%) of cases* | Number (%) of fractures | Number (%) of cases with positive skeletal survey | Prevalence among cases with positive skeletal survey (%) n = 119 | |||||
|---|---|---|---|---|---|---|---|---|
| Common fractures | Rib | 77 (25) | 490 (48) | 77 (100)* | 65 | |||
| Skull | 138 (44) | 138 (13) | 26 (19) | 19 | ||||
| Long bone | Shaft | 145 (46) | 110 (35) | 310 (30) | 171 (17) | 48 (44) | 40 | |
| SH-II | 13 (4) | 15 (1) | 4 (31) | 3.3 | ||||
| CMLs | 50 (16) | 124 (12) | 50 (100) | 40 | ||||
| Clavicle | 24 (8) | 28 (3) | 10 (42) | 9.2 | ||||
| Total† | 311 (99) | 966 (94) | 117 (38) | 98 | ||||
| Uncommon fractures | Hand and/or foot | 15 (5) | 36 (3) | 16 (100) | 13 | |||
| Scapula | 8 (2) | 13 (1) | 8 (100) | 6.7 | ||||
| Spine | 7 (2) | 13 (1) | 7 (100) | 5.8 | ||||
| Pelvis | 1(<1) | 1(<1) | 1 (100) | 0.8 | ||||
| Total† | 26 (8%) | 63(6%) | 26 (100) | 22 | ||||
| Total†† | 313 | 1,029 | 119 (37) | 100 | ||||
* Presence of rib fractures defined the skeletal survey as positive
† Total are cases on ISS and the new cases on follow-up skeletal survey
†† Infants with more than one fracture are considered only once CML’s classic metaphyseal lesions; SH-II Salter–Harris type 2.
In Barber et al.’s study, a total of 1029 fractures were encountered in 313 of 567 infants (55%) (Table 2.4) (57). The long bones were a site of fracture in 145 infants (26%), skull in 138 (24%), rib cage in 77 (14%), and clavicle in 24 (4.2%); uncommon locations, including the scapula, hand/foot, and pelvis, were the site of fractures in 26 children (4%). The distribution of fracture of the 1029 fractures was as follows: ribs, 490 (48%); long bones, 310 (30%); skull, 138 (13%); clavicle, 28 (3%). Sixty-three fractures (6%) involved the hands, feet, spine, scapula, or pelvis. The study highlighted the value of the follow-up SS (see Chapter 14) in fully documenting the extent of skeletal injury in cases of suspected abuse. In the 188 follow-up SSs, Barber et al. found 98 new fractures in 41 infants.
Based on the above studies, some general conclusions can be formulated regarding inflicted skeletal injuries. Overall the most common fractures in abused children involve the diaphyses of the long bones. However, in young infants, particularly those that are seriously injured, the most common inflicted skeletal injuries involve the rib cage, the metaphyses, and the skull. Studies drawn mainly from cases referred for evaluation of clinically significant orthopedic injuries may exclude cases of abuse with only rib and CMLs, fractures which are usually occult. Furthermore, because rib fractures and CMLs require high-detail imaging systems for optimal assessment, studies that fail to adhere to rigorous skeletal imaging protocols with follow-up surveys likely underestimate these strong indicators of abuse (45).
Although the appearances of extremity injuries vary with the particular bone affected, some general patterns of long bone fractures are well-recognized and are discussed in this chapter. The imaging features of specific extremity injuries (Chapters 3 and 4), thoracic (Chapter 5), spinal (Chapter 21), and cranial (and facial) injuries (Chapter 17) will be discussed separately.
Long bone injuries
A correlation of the imaging and postmortem pathologic findings of long bone injuries provides an in-depth understanding of how the morphologic alterations produce the spectrum of imaging findings and sheds light on the causative mechanisms of these important indicators of abusive injury.
Subperiosteal new bone formation
The periosteum consists of two layers, a relatively thick cambium or osteogenic layer and a thin outer structural fibrous layer. The periosteum is attached to cortical bone by anchoring collagen fibers which are much less numerous in infants than in older children (61). The periosteal type tissue that covers the physis and epiphysis is the perichondrium. LaCroix demonstrated the strong attachment of the fibrous layers of perichondrium to the epiphyseal cartilage (62). Hemorrhage beneath the periosteum of any cause mechanically elevates the periosteum from the surface of the bone. The perichondrial attachments are usually preserved, and as a result the maximal thickness of hemorrhage is along the diaphysis, and it gradually tapers toward the epiphysis (Fig. 2.2). Within several days the hemorrhage begins to undergo organization and the stimulated cells in the cambium layer of the periosteum produce trabeculae of reactive woven bone that then undergo mineralization. Importantly, subperiosteal new bone formation (SPNBF) may be a clue to a subtle underlying fracture.
Figure 2.2 Schematic representation of a subperiosteal hematoma (H), which lies between the cortex and the periosteum. New bone formation (arrows) occurs beneath the osteogenic layer of periosteum.
A variety of physical forces give rise to subperiosteal hemorrhage (SH). The early articles of Snedecor and others provide valuable insights into the pathogenesis of SH, as well as the metaphyseal lesions to be discussed (63, 64). These authors found bony alterations in neonates delivered with difficulty from breech presentations that resemble those noted in abused infants. They described excessive tractional and torsional forces applied in attempts to rotate and extract the fetus. Injuries were noted in both upper and lower extremities, and typically the involved regions were swollen after the day of delivery. Films obtained at birth were initially interpreted as normal. Radiographic changes were first noted between the fifth and seventh days. Although these findings were more dramatic than those usually encountered in abused infants, the types of forces producing both injuries are likely similar (see Chapter 11).
Drawing on these earlier observations and on personal experience, Caffey formulated his views on the pathogenesis of traumatic SPNBF in abused infants (2, 61). He postulated that severe manually administered forces result in stripping of the loosely attached periosteum along the shafts of the long bones. Such forces are applied as a limb is grabbed and pulled or twisted, or when the extremity is used as a “handle” for shaking. Identical lesions can be encountered in infants who have been shaken while being gripped around the thorax. It is possible that the accelerational forces generated as the extremities flail about cause periosteal stripping and SH. Of course, direct blows to the extremity may result in SH, but the indirectly applied forces account for many, if not most of the long bone injuries noted in abused infants.
SPNBF becomes visible radiographically as the newly formed bone mineralizes. A minimum of 5 (usually >7) days post-injury is required to see radiographic alterations (Fig. 2.3), and these radiographic alterations are often subtle and may be detectable on only one of several views of an extremity. The radiologic appearances are variable and include a hazy cortical margin, uni- or multilaminar linear opacities, or a more solid appearing zone of cortical thickening. In some cases, SPNBF is related to injury of the metaphyseal–epiphyseal complex and is greatest along the adjacent metaphyseal and diaphyseal regions. With more extensive injury, the hemorrhage elevates the periosteum along the entire shaft. When epiphyseal displacement is present, the periosteal attachment is usually maintained along the side of epiphyseal displacement and the subsequent subperiosteal new bone creates a “new” cortex aligned in a normal fashion to the displaced epiphysis (e.g., see Fig. 3.39). This finding reflects the remarkable remodeling capacity of massively injured infant long bones.
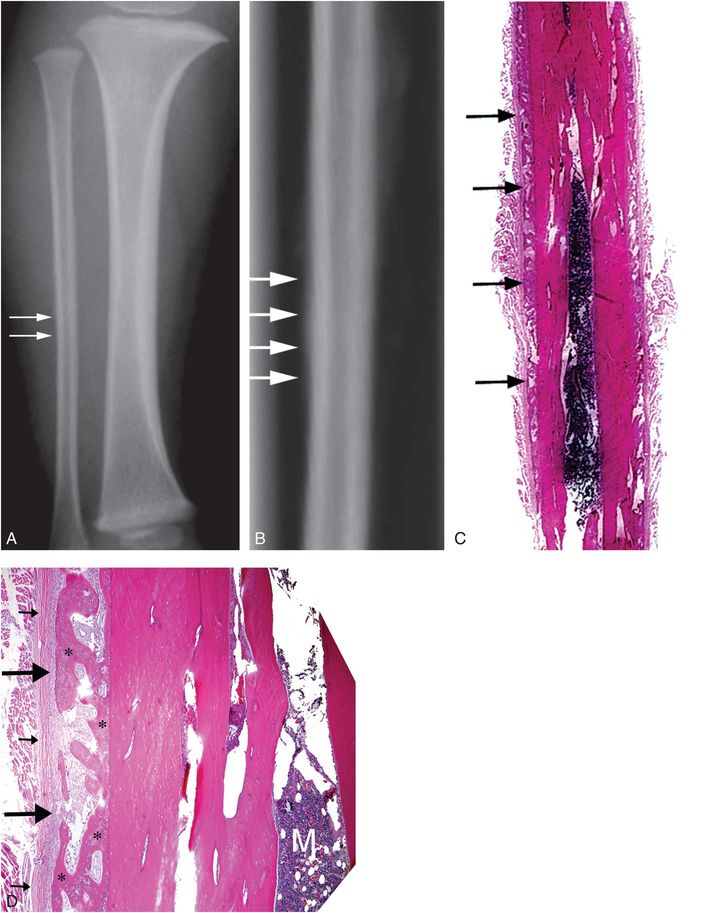
Figure 2.3 SPNBF. A 10-month-old infant with an inflicted head injury. AP view of the right lower leg from the postmortem SS (A) and the specimen radiograph (B) demonstrate focal SPNBF most evident along the lateral aspect of the mid-fibular diaphysis (arrows). C, Corresponding low power histologic section demonstrates a layer of SPNBF along the lateral margin of the bone (arrows). D, Medium power photomicrograph demonstrates elevation of the inner cambium (osteogenic) layer (large arrows) and an outer fibrous layer (small arrows) of the periosteum from the original cortex. Immature bone (*) is interspersed with fibro-vascular tissue. M, marrow.
Although SPNBF is most often observed radiographically, sonography can have an important role in the initial assessment. It may reveal subperiosteal fluid before it is evident radiographically. As healing progresses, sonography may also demonstrate a multilaminar character of the new bone (Fig. 2.4). Radionuclide bone scans are also useful in detecting early SH (Fig. 2.5) and the involved region usually shows avid uptake as organization of the blood progresses.
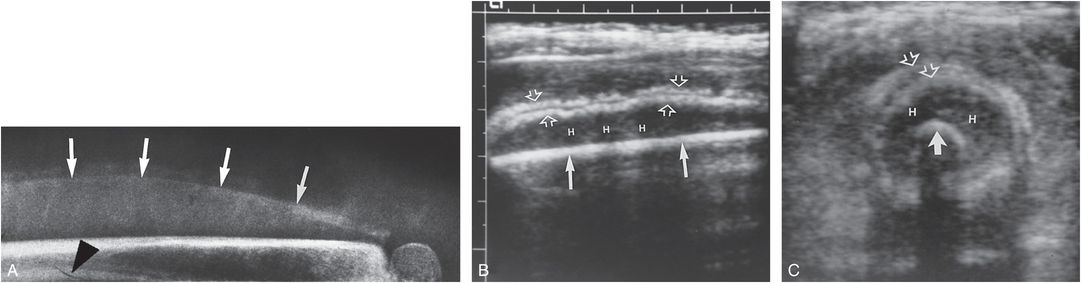
Figure 2.4 Subperiosteal hematoma: sonographic study. This infant presented with a swollen thigh and no history of trauma. A, Lateral projection of the right femur demonstrates a fine rim of SPNBF (arrows). Sagittal (B) and transverse (C) sonographic images of the femur demonstrate a hypoechoic hematoma (H) between the echogenic cortex (solid arrows) and two layers of SPNBF (open arrows). Note the subtle underlying fracture (arrowhead in A). Other studies revealed metaphyseal lesions typical of abuse. (Courtesy of Roy McCauley MD.)
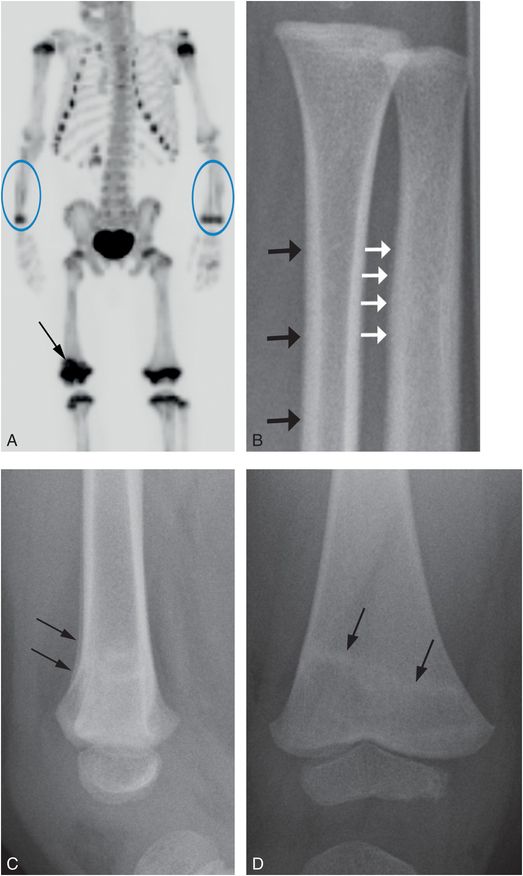
Figure 2.5 A two-year-old child with bruises and a history of domestic violence. A, Anterior maximum intensity projection (MIP) image of 18F-NaF PET bone scan demonstrates increased tracer uptake in the distal forearm bones (ovals), particularly in the left ulna, as well as increased activity in the right distal femoral metaphysis (arrow). B, Oblique radiograph of the right forearm shows fine SPNBF involving the distal ulna (white arrows) and indistinctness of the distal radial cortex (black arrows). C, Lateral view of the distal right femur show conspicuous SPNBF along the distal femoral metaphysis (arrows). The frontal projection (D) demonstrates a band of radiodensity traversing obliquely across the metaphysis consistent with a healing fracture (arrows).
When SPNBF is due to direct blows or associated with epiphyseal separation, findings are often evident clinically, with substantial swelling and occasional deformity. In contrast, isolated SPNBF occurring principally along the diaphyses of multiple long bones is generally clinically occult. Although commonly noted in abused infants, focal or generalized SPNBF is in itself a nonspecific finding and can be seen in infectious, traumatic, metabolic, and a variety of miscellaneous entities (see Chapters 7, 8). Modest diaphyseal SPNBF may be a normal “physiologic” finding in young infants. It most often involves the femur or tibia, and less commonly the humerus and forearm. It is usually bilateral and rarely exceeds 2 mm in thickness (65). Further discussion of physiologic SPNBF is found in Chapter 12.
Long bone shaft fractures
These familiar inflicted injuries are generally indistinguishable from their accidental counterparts.
Buckle fractures can occur at any site along the long bone shaft, especially in infants, but are particularly common in the metaphysis, where the cortices tend to be thinner than in the diaphysis (Fig. 2.6). The fractures usually buckle outward, but may wrinkle inward toward the medullary cavity. They are often visible only in one projection, and for this reason can be missed on the standard SS where only frontal views of the extremities are obtained (Fig. 2.7) (66).
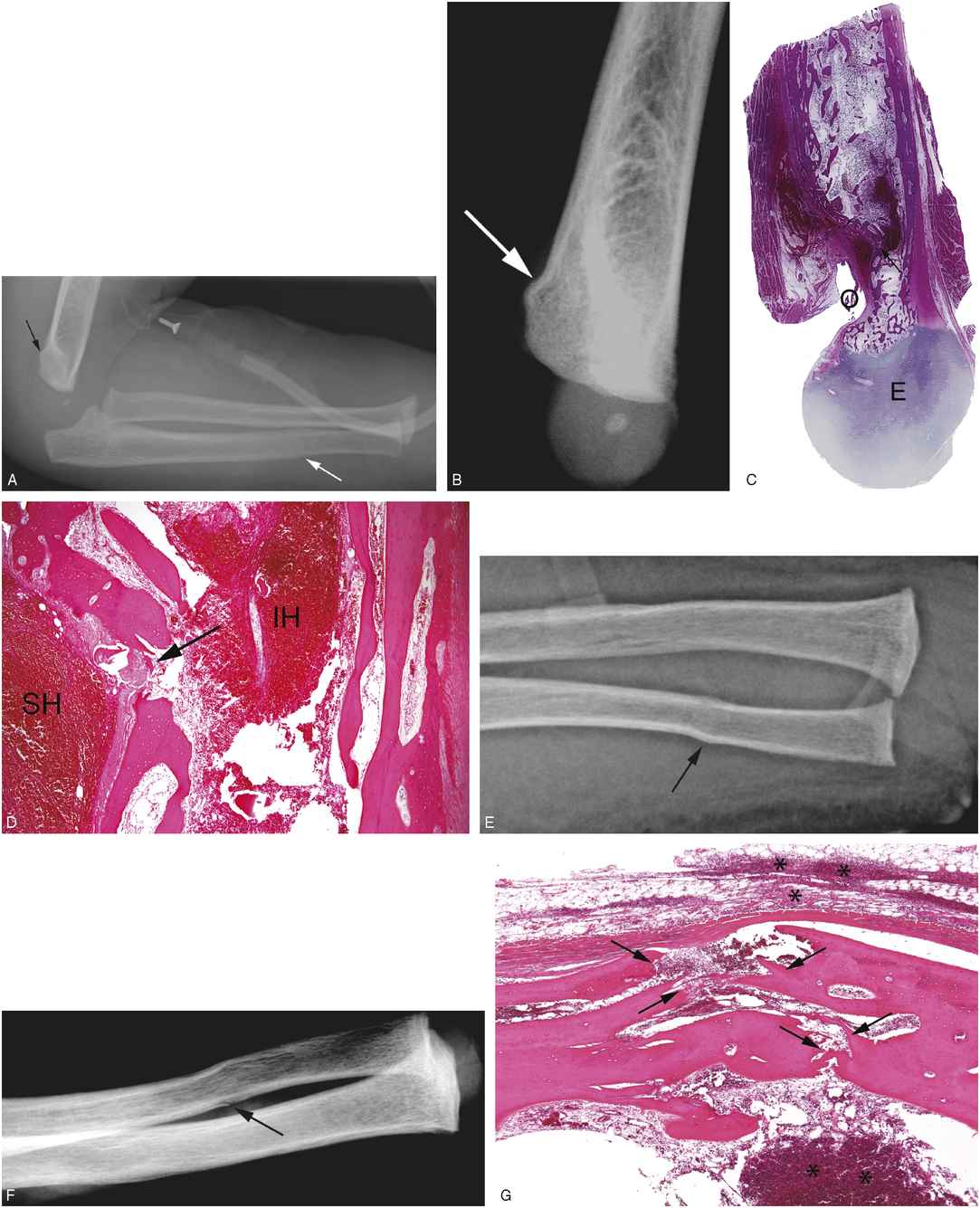
Figure 2.6 A nine-month-old infant with a fatal head injury and multiple fractures. (See same patient in Figs. 2.15, 4.3.) A, Lateral view of the left elbow and forearm two days after admission demonstrates a subtle buckling of the posterior cortex of the distal humerus (black arrow). There is also slight undulation of the distal ulnar cortex (white arrow). The infant lived for two additional days before dying. B, Lateral specimen radiograph of the distal humerus demonstrates the cortical buckle fracture to advantage (arrow). Corresponding low (C) and higher (D) power photomicrographs at the level of the olecranon fossa (O) demonstrate the cortical buckle fracture (arrows) and organizing subperiosteal hematoma (SH), as well as intramedullary hemorrhage (IH). (E = distal humeral epiphysis.) E, F, The ulnar fracture has a buckle pattern (arrow) on the frontal projection from the SS (E), and has the appearance of a greenstick fracture (arrow) on the oblique specimen radiograph (F). G, Corresponding low power photomicrograph demonstrates the fracture through the cortex of the shaft of the ulna (arrows). There is acute hemorrhage (*) in the periosteum, neighboring soft tissues, and the medullary cavity.

Figure 2.7 Buckle fracture. A 10-month-old infant with unwillingness to bear weight on left leg and no history of trauma. A, AP view of the left lower leg is normal. B, Lateral view demonstrates inward buckling of the anterior cortex of the proximal metaphysis. SS revealed three healing rib fractures.
If the applied traumatic force is distributed along the length of the bone, a so-called plastic bowing injury may result (Fig. 2.8). These are most often seen in the forearm and lower legs and may pose a diagnostic challenge. Comparison views of the opposite side may be required, and although SPNBF can be evident with healing, this is variable and a radionuclide bone scan may be required to document injury. These injuries tend to occur in the forearm and a transverse fracture in the radius or ulna should prompt close inspection of the adjacent bone for bowing deformity.
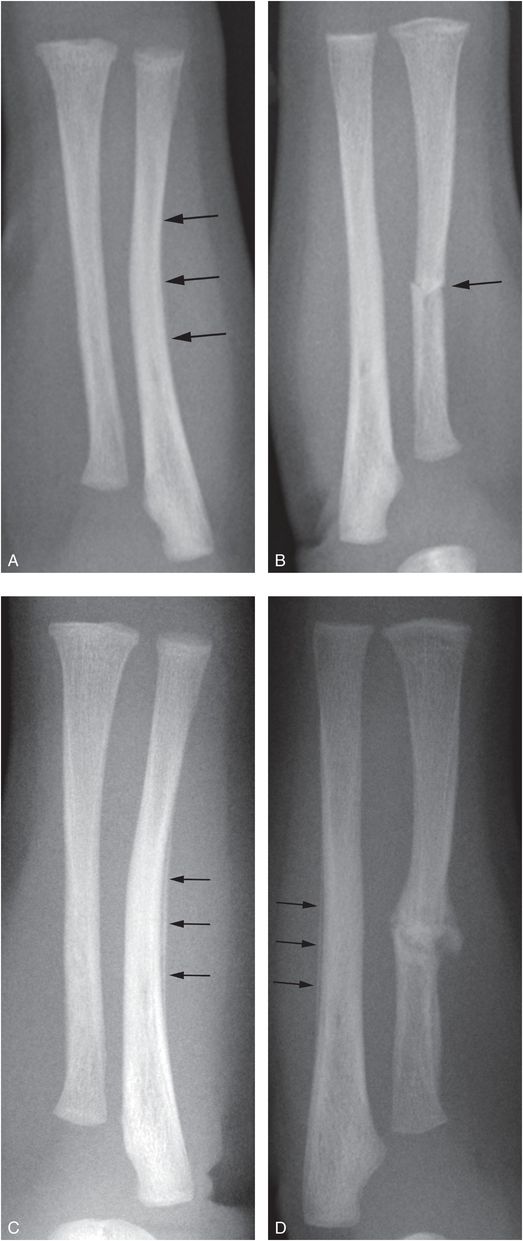
Figure 2.8 “Plastic” bowing injury. A five-week-old infant with fussiness and apparent discomfort when the right arm was moved. Radiographs done elsewhere revealed a right radial fracture. A, AP view of the left forearm demonstrates lateral bowing of the ulna (arrows). B, Contrast with the normal ulna on the right. Note the transverse fracture of the midshaft of the right radius (arrow). C, D, Follow-up SS two weeks later demonstrates post-traumatic SPNBF along the bowed midshaft of the left ulna (arrows), confirming the bowing fracture (C); healing of the right radial fracture is also evident (D). Fine SPNBF is now visible along the posterior margin of the right proximal ulna. This could be post-traumatic, but physiologic SPNBF could have a similar appearance. Further imaging revealed multiple rib fractures, CMLs, and SDH.
Greenstick fractures are also most often noted in the forearm and are manifest by disruption and angulation of one cortex and acute bending of the other. In the slender long bones, most fractures that disrupt opposite cortices are transversely oriented. On one view the fracture may appear to disrupt only one cortical margin, but on other views opposite cortices may be involved, suggesting a transverse extension across the medullary cavity (Fig. 2.6E,F).
Shaft fractures may extend completely across the medullary cavity with a transverse or oblique orientation (Fig. 2.9). Extensive SPNBF and callus may obscure the underlying fracture, but a careful search on high-detail radiographs in the region of maximal new bone formation may reveal a radiolucent fracture line (Fig. 2.10). On occasion the fracture lucency will extend into the SPNBF/callus, and this does not necessarily reflect a new fracture through old callus (Fig. 2.10); this may be the consequence of a zone of altered healing extending in continuity with the plane of the original fracture. When there is significant angulation, the fracture margins may become impacted (Fig. 2.11).
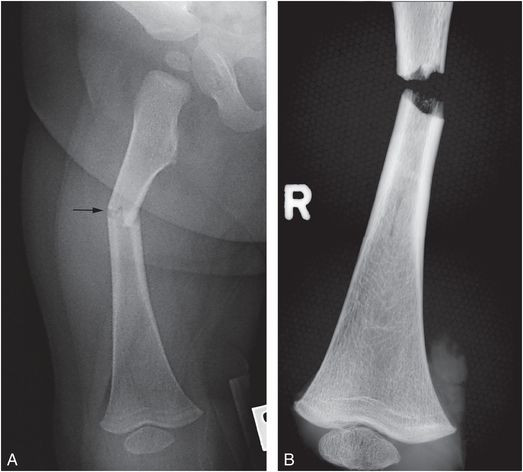
Figure 2.9 Acute transverse fracture. An eight-month-old fatally abused infant. (See same patient in Fig. 6.1.) A, AP postmortem radiograph of the right femur reveals a transverse fracture of the mid diaphysis (arrow). B, The acute fracture fragments fell apart at autopsy. The mother’s boyfriend pled guilty to beating her eight-month-old son to death in an attempt to make him stop crying. There were multiple other fractures.
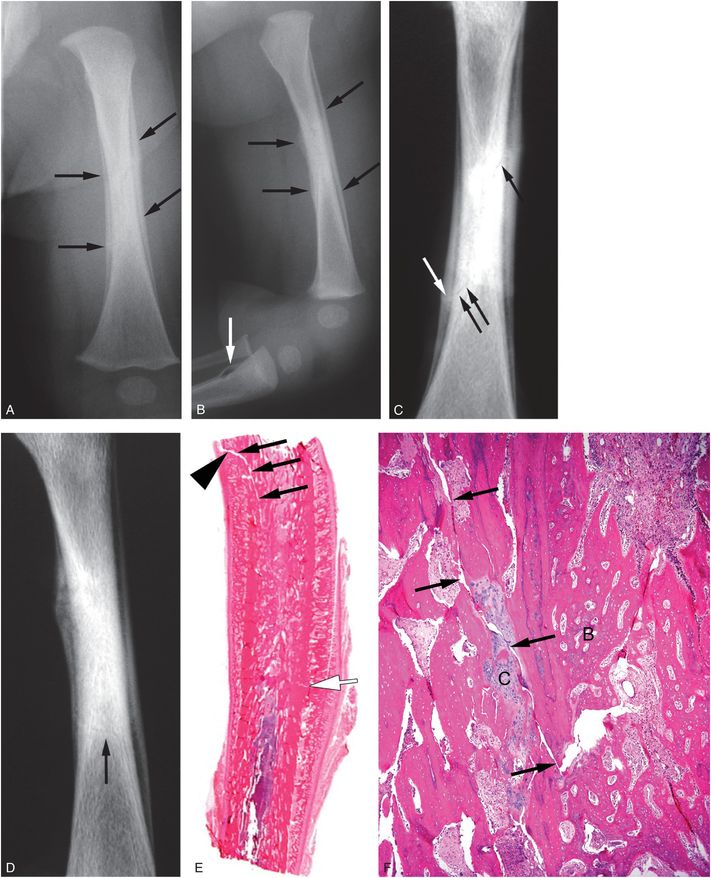
Figure 2.10 A seven-week-old infant with fatal head injury and multiple fractures. AP (A) and lateral (B) radiographs of the left femur from the postmortem SS show extensive SPNBF cloaking the diaphysis (black arrows). A definite fracture line is not visible. AP (C) and lateral (D) specimen radiographs demonstrate faint oblique intramedullary lucencies consistent with fracture (black arrows) with associated SPNBF (white arrow). E, Lower power histologic section shows extensive subperiosteal and intramedullary new bone formation. The fracture involves the posterior cortex proximally (black arrows) and the anterior cortex distally (white arrow), corresponding to the site of maximal thickness of SPNBF evident radiographically. Note that the fracture line extends into the SPNBF (arrowhead). F, A higher power view at a different level section demonstrates the fracture with adjacent cartilaginous (C) and bony (B) callus. Incidental note is made of cortical disruption of the proximal tibia (white arrow in B), presumably related to intra-osseous line placement during the resuscitation attempt.
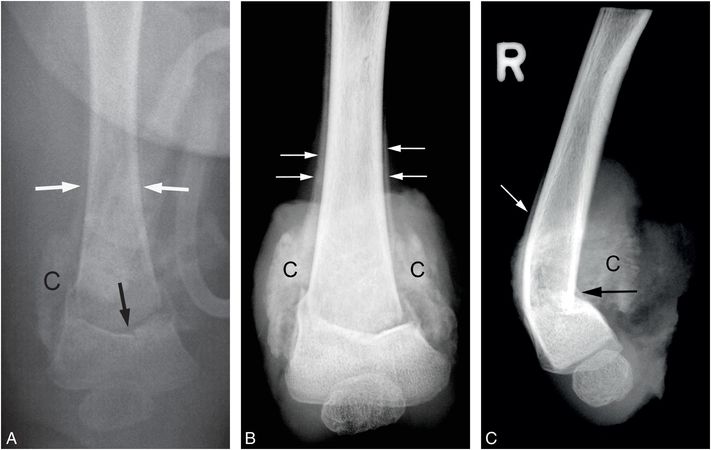
Figure 2.11 Healing impacted transverse fracture. (See same patient in Figs. 3.78, 3.87, 4.21, 4.29, 4.42.) A, AP view of the right femur from the SS in a five-month-old infant with a fatal head injury demonstrates a transverse fracture of the distal metaphysis (black arrow) with abundant callus (C) and SPNBF (white arrows). AP (B) and lateral (C) specimen radiographs demonstrate posterior impaction (black arrow), SPNBF (white arrows), and well-organized callus formation (C).
When an oblique fracture twists longitudinally through the cortex and medullary cavity, it may be referred to as a spiral fracture (see Fig. 3.16). Confusion exists regarding this terminology because a fracture line may appear to be oblique in one projection and spiral in another. Furthermore, what one observer considers a spiral fracture may be viewed by another as an oblique pattern.
Much has been written about the relationship between fracture orientation and etiology with regards to accidental versus abusive injuries (31, 32, 44, 47, 48, 67, 68). Most recent studies show a poor correlation between the pattern of shaft fracture and inflicted trauma (47, 69–71). Spiral and oblique fractures appear to result from torsional forces applied to the long bone rather than from direct injury. To the extent that many inflicted injuries in children, and probably most injuries to infants, result from indirect, often torsional forces, it is not surprising that oblique fractures are common. However, accidents may generate similar twisting forces and produce identical patterns of fracture. Importantly, these types of fractures need to be correlated carefully with the history, as well as associated clinical and imaging findings (see Chapter 10) (72). Although patient age and ambulatory status are vital factors in assessing injury significance, isolated long bone shaft fractures should be considered low-specificity injuries on purely radiologic grounds. Nonetheless, the severity of a shaft fracture is important in determining the type and magnitude of forces resulting in the injury, as well as the consistency with the purported history. A severely displaced, angulated, or comminuted shaft fracture implies a higher energy event than a simple linear fracture with minimal anatomic deformity (see Fig. 3.19). There is a growing interest in the biomechanics of long bone shaft fractures, and insights gained from these laboratory studies may be of value in characterizing the forces required to produce injuries in cases of abuse (73–75).
Authors have reported diffuse sclerosis or chalkiness involving the long bones of abused children (12, 61, 76). Silverman suggested that the sclerosis is secondary to bone reaction caused by repetitive trauma (12). A variety of unusual long bone injuries occur that relate to the unique anatomic characteristics of the specific region involved. These are considered separately as individual anatomic regions in Chapters 3 and 4.
The CML
Background
For those physicians and other professionals dealing with cases of suspected physical child abuse, an important question inevitably arises: Regardless of history, in an otherwise normal patient, is there an injury that can be viewed as highly specific for inflicted trauma? The classically described metaphyseal lesions of the long bones satisfy this definition more closely than any other skeletal, central nervous system, or visceral abnormality occurring in cases of child abuse (35, 67, 77–80). These injuries are common in infants at high risk for abuse, but are rare in infants with skull fractures associated with falls and no other risk factors for abuse (80). In their retrospective study of a period of 10 years, Kleinman and others compared the prevalence of the CML on high-detail ACR-standardized SSs in infants at low and high risk for abuse (80). Low-risk infants met all of the following criteria: skull fracture without significant ICI on computed tomography (CT), history of a fall, and no other social risk factors for abuse. High-risk infants met all of the following criteria: significant ICI, retinal hemorrhages (RHs), and skeletal injuries (excluding CMLs and skull fractures). There were 42 low-risk infants (age range: 0.4–12 months; mean age: 4.4 months) and 18 high-risk infants (age range: 0.8–10.3 months; mean age: 4.6 months). At least one CML was identified in nine infants (50%) in the high-risk category and zero in the low-risk group; this difference was statistically significant (P < 0.0001; 95% CI, from 0–8% to 29–76%). These case control data add to the many case studies that support the strong association of CMLs with infant abuse (56).
Prevalence
In Barber et al.’s study of SSs in 567 infants, a total of 124 CMLs were identified in 50 patients (mean age: 4 months; range: 1 week to 10 months); 29 infants had two or more CMLs (mean: 2.5; range: 1–11). The distribution of the injuries is shown in Fig. 2.12 (57). Fifteen infants had bilateral symmetric involvement of the lower extremities; distal femur in 10 cases and proximal tibia in 7 cases. Four infants had both bilateral distal femoral and proximal tibia CMLs. This strong predilection for the lower extremities is in keeping with the findings noted in postmortem material (see Fig. 2.1) (45, 57).
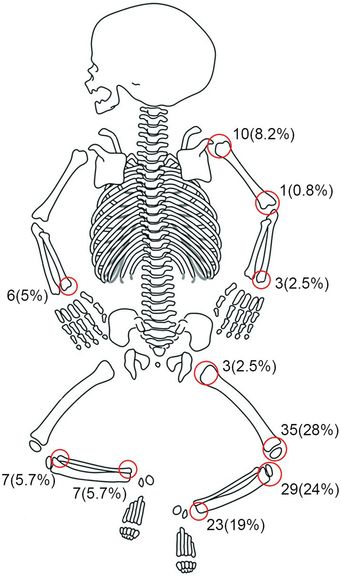
Figure 2.12 Distribution of 124 CMLs in 50 of 567 infants. (From Barber I, Perez-Rossello JM, Wilson C, Kleinman PK. The yield of high-detail radiographic skeletal surveys in suspected infant abuse. Pediatr Radiol. 2015;44(1) 69–80.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree