Skull Base and Cervical Spine
Eugen B. Hug
John E. Munzenrider
Chordomas arise from the remnants of the notochord. They comprise only 1% to 4% of primary bone tumors and arise within the axial skeleton, most commonly in the sacrococcygeal region (50% to 66%) and the skull base (˜35%).1 Chondrosarcomas develop in any bone preformed by cartilage. They arise de novo in normal bone or secondarily in diseased bone (Paget disease; irradiated bone) or in preexisting benign cartilaginous tumors. Common sites of origin are the pelvis and femur; only 5% of tumors develop in the head and neck region.1
Chordomas and chondrosarcomas located in the skull base and cervical spine are uncommon tumors and challenging to manage. Because of their location either in the clivus, petrous bone, or upper cervical vertebrae, adjacent to cranial nerves and major blood vessels, gross total surgical resections were historically rarely accomplished. Rapid advancements in microsurgical resection techniques have now allowed surgeons to perform macroscopically confirmed gross total resection in selected patients, even in areas in which resection until recently was considered inadvisable.2 However, even in the “best hands” and using the most sophisticated equipment, the ability to obtain a complete surgical resection remains elusive for many patients. Drs. L. Sekhar and D. Wright are some of the pioneers and leaders in skull base neurosurgery. Their recently published results indicate an overall 56% chance of complete or “near-”complete resection (near-complete = small residual disease radiographically) in 64 patients with chordomas or chondrosarcomas of the skull base.3 In other words, >50% of patients still had some degree of residual tumor after the most advanced neurosurgery and many patients presented with disease too extensive to permit gross total resection. One can only speculate about the chances of obtaining gross total resection in less specialized centers.
What are the chances for a patient to survive the diagnosis of chordoma? Before scrutinizing individualized risk prognosticators and evaluating different treatment modalities, it is useful to look at general benchmarks. According to the Surveillance, Epidemiology, and End Results (SEER) program of the US National Cancer Institute, the median survival was 6.29 years in 400 cases of microscopically confirmed chordoma diagnosed between 1973 and 1995;4 5- and 10-year survival rates were 67.6% and 39.9%, respectively.
Because of the “piecemeal” resection technique that is required for skull base surgery, even gross total resection often does not result in oncologically complete microscopic resection; that is, negative resection margins around the entire tumor specimen are rarely accomplished. Despite the possibly long period of stability following subtotal resection, ultimately most patients will experience recurrence and will die of their disease. Because the metastatic rate is relatively low (˜5% to 20%),5,6 local control of these aggressive tumors is of paramount importance. Accordingly, most physicians recommend adjuvant postoperative treatment.2 The results of chemotherapy have been discouraging thus far; therefore, RT remains the postoperative modality of choice.6
The skull base has an anatomically very complex shape, and tumors arising in the skull base generally have a highly irregular contour. With the immediate proximity of critical normal structures, such as brainstem, optic nerves, and temporal lobes, only moderate dose radiation could be delivered with conventional photon RT. Local control rates after doses <60 Gy were disappointing, and most patients
died of locally progressive disease. Recurrence rates as high as 70% to 100% even for small lesions have been reported after conventional megavoltage x-radiation therapy, and survival curves tended to follow a continuous downward slope.5,7,8 Rich et al.7 observed 13 local treatment failures in 18 patients receiving a photon dose of <60 Gy (local control 28%). Catton et al.,5 at Princess-Margaret Hospital reported a median overall survival time of 62 months in 45 patients. The median time to progression was 35 months and only approximately 20% of patients were progression-free at the actuarial 5-year point.
died of locally progressive disease. Recurrence rates as high as 70% to 100% even for small lesions have been reported after conventional megavoltage x-radiation therapy, and survival curves tended to follow a continuous downward slope.5,7,8 Rich et al.7 observed 13 local treatment failures in 18 patients receiving a photon dose of <60 Gy (local control 28%). Catton et al.,5 at Princess-Margaret Hospital reported a median overall survival time of 62 months in 45 patients. The median time to progression was 35 months and only approximately 20% of patients were progression-free at the actuarial 5-year point.
One could argue that the historically poor conventional external beam irradiation data were not only dose related, but also in part due to inadequacies at that time of the available diagnostic imaging to accurately identify the true extent of tumor. The recently published series of Hacettepe University in Ankara, Turkey, however, utilized modern imaging and radiation treatment techniques but at conventional doses.9 Five-year progression-free survival rates and overall survival rates of 23% and 35%, respectively, in 18 patients with clival chordomas following 50 to 64 Gy confirm the poor outcome with these doses and emphasize the importance of high target doses.
Skull base and paraspinal tumors early on became one of the main applications of proton radiotherapy (RT) at Massachusetts General Hospital, Boston, and the Harvard Cyclotron Laboratory, Cambridge, MA (MGH/HCL).10 The first patient with skull base chordoma was treated in 1974, within 1 year of initiation of large-field proton RT at MGH/HCL. Both anatomic location and tumor histology were considered an excellent opportunity to demonstrate the safety and efficacy of this novel, high-precision treatment modality. Following the first encouraging report by Austin-Seymour, Suit, and Goitein in 1985,11 and additional publications indicating its beneficial effects,10,12,13 all operational proton centers with sufficiently high proton energy have included skull base tumors in their clinical program. Despite the relative rarity of these tumors, >1,700 patients have been treated and reported worldwide. The proton RT results therefore constitute the single largest treatment modality experience ever reported for skull base and cervical spine chordomas and chondrosarcomas.13, 14, 15, 16, 17
LOCAL CONTROL AND SURVIVAL
Chondrosarcomas
Proton RT has convincingly established that low-grade chondrosarcoma of the skull base is a curable disease. The patient population treated at MGH with combined proton/photon RT constitutes the largest series on the treatment of chondrosarcomas of the skull base worldwide. This series continues patient accrual and follow-up; hence, the data will continue to mature and provide invaluable long-term outcome information for the foreseeable future. A clinicopathologic study of 200 cases revealed only 3 local failures after combined proton/photon irradiation to a median total dose of 72.1 Gy (RBE) with a follow-up period extending up to 18.5 years (median: 63 months).18
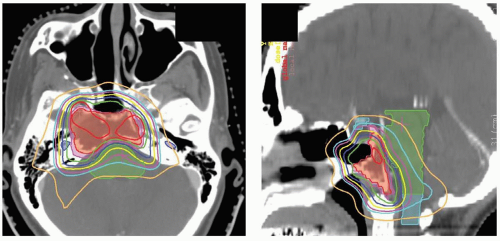
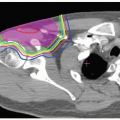
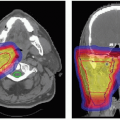
Munzenrider and Liebsch for the MGH/HCL group have reported results on 519 skull base patients, treated between 1975 and October 1, 1998. This included 229 chondrosarcoma patients (105 men and 124 women) who ranged in age from 10 to 80 years (median 39 years). Sixteen patients were ≤18 years of age. Local recurrence-free survival at 5 and 10 years was 98% and 94%, respectively. Five- and 10-year overall survival rates were 91% and 88%.17 A representative dose distribution for a patient treated for chondrosarcoma of the base of the skull at the MGH is shown in Figure 14.1.
Other institutions have reported local control rates for skull base chondrosarcomas exceeding 80% following proton RT: 91.6% actuarially at 3 years in 26 patients treated at the Centre de Protontherapie d’Orsay in Orsay, France;19 100% actuarially at 3 years in 11 patients using
spot-scanning proton delivery at the Paul Scherrer Institute (PSI) in Villigen, Switzerland,20 and 83.9% with a median follow-up of 53 months at Loma Linda University Medical Center (LLUMC) in Loma Linda, CA, resulting in a 5-year actuarial overall survival rate of 91.7%.21
spot-scanning proton delivery at the Paul Scherrer Institute (PSI) in Villigen, Switzerland,20 and 83.9% with a median follow-up of 53 months at Loma Linda University Medical Center (LLUMC) in Loma Linda, CA, resulting in a 5-year actuarial overall survival rate of 91.7%.21
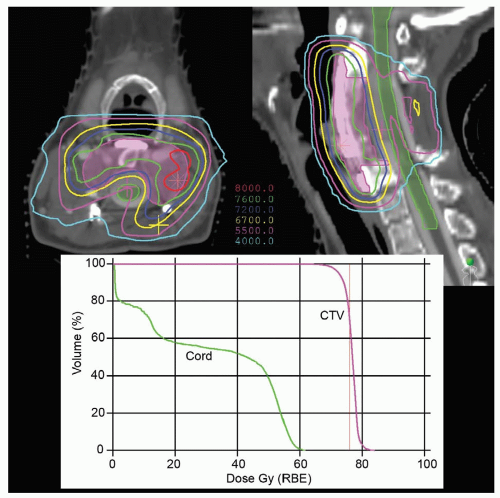
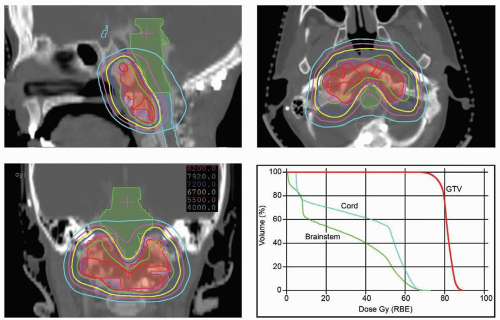 Figure 14.2 Dose distribution for a patient treated at Massachusetts General Hospital (MGH) for a chordoma of the skull base. The patient was treated with a combination of photons and protons to a total dose of 79.2 Gy (RBE) (18 Gy with photons). The normal tissue contraints were the same as those in Figure 14.1. GTV, gross tumor volume. |
It is difficult to establish prognostic indicators for risk of failure, because the overwhelming majority of patients will be cured after proton RT—seemingly regardless of age, gender, degree of gross disease, or primary versus recurrent disease.
This raises several management questions: How aggressive should surgery be? There is general consensus that a major tumor debulking is beneficial if there is critical normal tissue compression by tumor and surgery will improve tumor geometry with respect to critical normal structures to permit optimal target coverage by the prescription dose and to minimize the risks of adverse events. It is noteworthy that in the MGH/HCL series, few patients had complete surgical resection, that is, most patients underwent therapy with radiographically identifiable and quantifiable, gross disease. Hence, additional surgery with the sole intention to accomplish gross total resection does not seem to be justified for skull base chondrosarcomas based on outcome data after proton RT.
At present the average prescribed tumor dose for chondrosarcomas ranges from 66 to approximately 76 Gy (RBE) depending on the individual proton institution—averaging approximately 72 Gy (RBE) at 1.8/2.0 Gy (RBE) dose per fraction. The near future will reveal if the outstanding long-term MGH/HCL data will indeed be replicated by other institutions. In comparing the results of proton RT with alternative radiation treatment modalities, it is of paramount importance to separate the diagnosis of chondrosarcoma from chordoma in any analysis (vide infra).
Chordomas
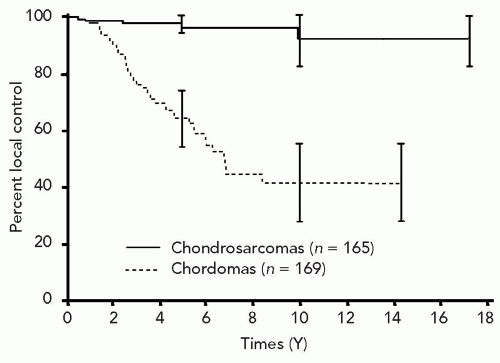
In the study cited in the preceding text, Munzenrider and Liebsch also reported results on 290 patients with chordomas (200 chondroid and 90 nonchondroid) of the skull base. One hundred and fity-nine patients were men and 131 were woman. Ages ranged from 1 to 80 years (median 39 years). Fifty-four were ≤18 years of age.17 Prescribed doses ranged up to 83 Gy (RBE), the dose given to female patients enrolled in a prospective randomized dosesearching clinical trial. Usually patients received four fractions of protons and one of megavoltage x-rays each week. Daily doses were 1.8 Gy with photons or 1.92 Gy (RBE) with protons. The median follow-up period was 41 months, and the maximum follow-up interval was 22 years. At 5 and 10 years, local recurrence-free survival (LRFS) rates for chordomas were 73% and 54%, respectively. Overall survival was 80% and 54%, respectively. LRFS was significantly better for male than for female patients at both 5 and 10 years: 81% versus 65% (ρ = 0.035) and 65% versus 42% (ρ = 0.007), respectively. Further analysis indicated that most male patients would achieve long-term tumor control and cure (˜60% at 10 years with plateau of the survival curve). In contrast, female patients continued even at 10 years to suffer tumor recurrence and death (42% local control at 10 years with continued decline of the survival curve). These data demonstrated for the first time that a subgroup of patients with chordomas (in this case male patients), might indeed be curable by high-dose irradiation. Dose distributions for selected patients with skull base and cervical chordomas are shown in Figures 14.2 and 14.3.
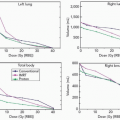
An earlier analysis of 334 patients with adult skull base chordomas and chondrosarcomas, with median follow-up approaching 5 years, showed that LRFS was significantly better for chondrosarcomas than for chordomas at both
5 years and 10 years: 97% versus 64% and 92% versus 42%, respectively as shown in Figure 14.4.
5 years and 10 years: 97% versus 64% and 92% versus 42%, respectively as shown in Figure 14.4.
In general, the MGH/HCL data have been confirmed at LLUMC. Hug et al. reported early outcomes for the LLUMC group on 33 patients with chordomas of the skull base and cervical spine treated almost exclusively by protons to doses between 64.8 and 79.2 Gy (RBE), mean 70.7 Gy (RBE), using five fractions per week.15 Followed for a mean period of 33 months, the crude local control rate was 76% and 3-year actuarial local control rate was 67%. A more recent update of the LLUMC data was presented in 2002 at the North American Skull Base Society’s Annual Meeting. W. Johnson reported on 78 patients with chordomas followed for a mean period of 53.1 months.21 The crude local tumor control rate for chordomas was 63.5% which translated into an actuarial overall survival rate at 5 years of 77.4%. Gross tumor size (≥25 mL) at time of proton RT continued to be an independent, statistically significant risk variable.
The team at PSI in Switzerland recently reported their initial results on 18 patients with chordomas of the skull base treated with spot-scanned proton RT between 1998 and 2003.20 Patient population data, tumor volumes, and prescription target doses were comparable to patients treated at other proton centers. The median follow-up time was 29 months (range 6 to 68 months). The authors reported one patient with “radiologic progression, not requiring additional treatment” and two other chordoma patients with “clinical tumor progression requiring treatment” resulting in a 3-year actuarial progression-free survival rate of 87.5%—thereby comparing favorably with early reports from the proton centers using passive scattering.
The Centre de Protontherapie d’Orsay in Orsay, France, reported on treatment of 64 chordomas of the skull base and cervical spine: At a median follow-up of 34 months, the local control rate at 3 years after a median total dose of 67 Gy (RBE) was 69.2%. A previous publication from the same group reported an actuarial overall survival rate for this patient population of 75% at 3 years.19,22
ADVERSE EFFECTS
Acute and late effects depend on tumor location of the primary site within the skull base or upper spine. Irradiation of the anterior skull base will expose the optic structures, hypothalamus, pituitary gland, frontal lobes, and temporal lobes to a higher risk of radiation injury. In contrast, these structures might not receive significant radiation doses with lesions involving the occipitocervical junction, where acute dysphagia and long-term risks of hearing loss, or injury to brainstem, cerebellum, and upper spinal cord need to be considered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree