Skull, Ventricles, and Developmental Abnormalities
Hisham M. Dahmoush
Shyam Sabat
Sathish Kumar Dundamadappa
Prachi Dubey
QUESTIONS
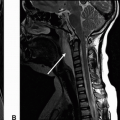
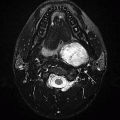
1 A 40-year-old male presents with acute-onset headache and altered mental status shortly after minor blunt trauma to the head. Key images are provided below.
|
1a What is the most likely diagnosis?
A. Intraventricular rupture of a colloid cyst
B. Intraventricular rupture of a dermoid cyst
C. Pneumoventricle
D. Subacute intraventricular hematoma
1b What is the most likely explanation of T1 hyperintensity within this lesion on precontrast images, as shown in Image A?
A. Fat
B. Sebaceous proteinaceous contents
C. Hemorrhagic contents
D. Calcification
View Answer
1b Answer A. Fat. Protein, calcification, and hemorrhage will show varying degree of hyperattenuation on CT unlike this case.
|
Imaging Findings: Lobulated T1 hyperintense intraventricular mass (A), which is hypointense on fat saturation T2 (B) and hypoattenuating on CT, most compatible with fat. Note a fat fluid level is seen anteriorly in the frontal horn of the left lateral ventricle. These features are most compatible with intraventricular rupture of a fatty lesion, such as dermoid cyst.
Discussion: Ruptured dermoid with intraventricular fat fluid level. Dermoid cysts are rare congenital inclusion cysts, resulting from inclusion of embryonic ectoderm into neural tube during 3rd to 5th weeks of embryonic life. They tend to occur in the midline, commonly sellar region, frontonasal region, and in the posterior fossa. The cyst wall is characterized by a stratified squamous epithelium capsule that contains dermal elements including sebaceous glands, sweat glands, and hair follicles. The contents of cyst include desquamated epithelium, sebaceous gland secretions, fat, and hair. Calcification and rarely teeth can be seen.
Unruptured lesions are mostly asymptomatic; the symptoms depend on location and size and mostly related to the mass effect. The dermoid cysts can grow, related to increase of internal contents by desquamation of epithelium and secretion of adnexal glands. Rupture of dermoid is rare, but well documented. The rupture is usually spontaneous but has also been reported after closed head trauma. It is hypothesized that increases in glandular secretions, possibly related to age-related hormonal changes mainly lead to rapid enlargement and subsequent rupture. On rupture, patients present with various symptoms including headache, seizures, focal neurologic deficits, aseptic meningitis, hydrocephalus, vasospasm, and cerebral ischemia. Aseptic meningeal inflammation by ruptured contents and aqueductal occlusion are felt to be the etiology for these symptoms.
On imaging, these are mostly fatty lesions, secondary to liquid cholesterol. On CT scans, the lesions show fat density. On MRI, the lesions are hyperintense on T1-weighted images and shows variable intensity in T2-weighted images. They can be heterogeneous, related to the calcification. They show no enhancement following contrast administration. On rupture, fat density/intensity droplets will be seen in subarachnoid spaces and also within the ventricular system. Pial enhancement can be seen from chemical meningitis in cases of rupture.
Differential diagnosis:
Epidermoid cyst: This is another inclusion cyst and shows a near CSF signal and not fat signal.
Lipoma: Homogenous fat attenuation.
References: Koh YC, Choi JW, Moon WJ, et al. Intracranial dermoid cyst ruptured into the membranous labyrinth causing sudden sensorineural hearing loss: CT and MR imaging findings. Am J Neuroradiol 2012;33(5):E69-E71. doi: 10.3174/ajnr.A2627. Liu JK, Gottfried ON, Salzman KL, et al. Ruptured intracranial dermoid cysts: clinical, radiographic, and surgical features. Neurosurgery 2008;62(2):377-384; discussion 384. doi: 10.1227/01.neu.0000316004.88517.29.
Osborn AG, Preece MT. Intracranial cysts: radiologic-pathologic correlation and imaging approach. Radiology 2006;239(3):650-664. doi: 10.1148/radiol.2393050823.
2 A 40-year-old male presents with chronic headaches and recently worsening nausea and vomiting. Key images from initial workup are shown below.
|
2a Based on the above images, what is the most likely diagnosis?
A. Intraventricular meningioma
B. Colloid cyst
C. Subependymal giant cell astrocytoma
D. Central neurocytoma
|
2b What is the most likely explanation for the periventricular white matter hyperintensity on FLAIR image shown above?
A. Periventricular leukomalacia (PVL)
B. Ependymitis granularis
C. Transependymal CSF flow
D. Chronic microangiopathic change
View Answer
2b Answer C. Transependymal CSF flow. This is the most likely explanation given the confluent periventricular FLAIR hyperintensity in the setting of hydrocephalus due to a large colloid cyst obstructing the foramen of Monro. Ependymitis granularis is a normal variant, smaller triangular foci of FLAIR hyperintense signal seen abutting the frontal horns of lateral ventricles. Chronic microangiopathic change is unlikely given no other deep or subcortical white matter changes are seen. PVL is seen in children because of prematurity-related white matter injury resulting in necrosis and cyst formation, unlike this case.
Imaging Findings: Figure 1. There is a rounded hypointense structure on T2w sequence at the foramen of Monro (A), that is, hyperdense on CT (B) and isointense to white matter on Sag T1w (C).
Figure 2. There is periventricular FLAIR hyperintensity in the setting of obstructive hydrocephalus due to a colloid cyst obstructing the foramen of Monro.
Discussion: Colloid cysts are rare anterior third ventricular lesions, typically draped by fornices. Location other than anterior third ventricle (other ventricles or even outside the ventricular system) has been reported, but very rare. These are spherical smooth-walled cysts and vary in size from a few millimeters to several centimeters.
The cyst is lined by simple to pseudostratified epithelial lining with interspersed goblet cells and ciliated cells. The cyst content is likely derived from secretions and breakdown products from the epithelium.
They are typically seen in adults in third to fifth decade of life with headache being the most common presenting symptom. On CT, about two-thirds of the lesions are hyperdense and about one-third isodense and rarely hypodense. The appearance on MRI is more variable. On T1 images, 50% of lesions are hyperintense and the rest hypointense or isointense. On T2-weighted images, most are hypointense. Hemorrhage and fluid-fluid levels can occasionally be seen. Following contrast administration, the lesions either do not enhance or only show thin peripheral enhancement. The smaller lesions are often better seen on CT and can occasionally be not apparent on MRI because of their signal characteristics and also related to thicker slices. Biventricular hydrocephalus is the dreaded complication of colloid cysts, secondary to obstruction at the foramen of Monro. They may have pendulous attachment to third ventricular roof and can cause intermittent hydrocephalus. Acute hydrocephalus and sudden death are known to occur with these lesions. But in our clinical experience, these are rare with smaller lesions. These are generally surgically treated. Hypodense appearance on CT and iso- to hyperintensity on T2 images suggest less viscous and more fluid-like content and may correlate with easier stereotactic aspiration. Recurrence rate is about 10% with incomplete resection of the wall.
References: Armao D, Castillo M, Chen H, et al. Colloid cyst of the third ventricle: imaging-pathologic correlation. Am J Neuroradiol 2000;21(8):1470-1477.
Marshman LA, Chawda SJ, David KM. Change in CT radiodensity of a colloid cyst of the third ventricle: case report and literature review. Neuroradiology 2004;46(12):984-987. doi: 10.1007/s00234-004-1303-2.
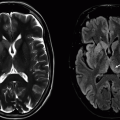
3 A 70-year-old male with progressive cognitive decline and gait abnormality presents for further assessment of symptoms. Key images from MRI are provided below.
|
3a Based on the above images and clinical features, what is the most likely diagnosis?
A. Aqueductal stenosis
B. Tectal glioma
C. Idiopathic normal pressure hydrocephalus (iNPH)
D. Age-related white matter atrophy
View Answer
3a Answer C. Idiopathic normal pressure hydrocephalus (iNPH). This is most likely given the clinical features of cognitive dysfunction and gait abnormality in the setting of profound ventriculomegaly out of proportion to sulcal enlargement is seen. Image A shows prominent flow through the aqueduct on the phase contrast CSF flow study and Image B shows wide patency of the aqueduct, arguing against the diagnosis of aqueductal stenosis. Tectal glioma also causes obstruction at the aqueductal level, not seen in this case. The lack of sulcal enlargement is atypical for age-related atrophy.
3b Which other diagnostic tests can be performed to aid in the diagnosis of idiopathic normal pressure hydrocephalus?
A. High-volume lumbar puncture
B. CT myelogram
C. Transcranial Doppler US
D. Florbetapir amyloid imaging
View Answer
3b Answer A. High-volume lumbar puncture. Pre-LP and post-LP functional testing can be performed with withdrawal of 30 to 40 mL of CSF as an additional diagnostic tool for idiopathic NPH. The other choices are not appropriate tools for assessment of iNPH.
|
Imaging Findings: Sagittal phase contrast CSF flow MRI showing hyperdynamic flow through the cerebral aqueduct (A). Sagittal 3D CISS showing a patent cerebral aqueduct with prominent dilation of lateral, third, and fourth ventricle (B). Axial T2w image showing dilated lateral ventricles out of proportion to sulcal enlargement. There is no evidence of periventricular transependymal CSF flow (C). These features in the current clinical setting are most compatible with normal pressure hydrocephalus.
Discussion: Idiopathic normal pressure hydrocephalus (iNPH) is a syndrome of ventricular enlargement associated with the clinical Hakim-Adams triad of urinary incontinence, dementia, and gait abnormalities without an obstructive cause.
It is thought to be related to nonobstructive impairment of CSF reabsorption. Ventriculosulcal disproportion is present in the form of widening of the ventricles and sylvian fissure with narrowing of suprasylvian and medial hemispheric subarachnoid spaces.
Evans index is used as an estimate of ventricular enlargement, measured as a ratio between the maximal diameter of the frontal horns and the inner diameter of the skull, with a ratio of >0.3 considered abnormal. Recent study shows, however, that more than one-fifth of the population-based sample had an EI > 0.3 and an EI ≥ 0.3 was average for men 80 years or older in age. This suggests that diagnosis of iNPH cannot be made based on EI alone, and clinical features as well as data from other diagnostic test should be factored into consideration.
A phase contrast MRI with measurement of aqueductal CSF stroke volume, high-volume LP (drainage of 30 to 40 cc of CSF, with pre-LP and post-LP functional status assessment), and nuclear cisternogram are other diagnostic test that can be utilized for iNPH diagnosis.
Management can be conservative or surgical using VP shunting or recently endoscopic third ventriculostomy. Hyperdynamic CSF flow through the aqueduct has been associated with good response to shunting. Phase contrast MRI can be used to quantify the aqueductal stroke volume, with iNPH patients who have twice the aqueductal stroke volume compared to age-matched controls, being most responsive to shunting.
References: Bradley WG Jr. Magnetic resonance imaging of normal pressure hydrocephalus. Semin Ultrasound CT MR 2016;37(2):120-128.
Jaraj D, Rabiei K, Marlow T, et al. Estimated ventricle size using Evans index: reference values from a population-based sample. Eur J Neurol 2017;24(3):468-474.
Tudor KI, Tudor M, McCleery J, et al. Endoscopic third ventriculostomy (ETV) for idiopathic normal pressure hydrocephalus (iNPH). Cochrane Database Syst Rev 2015;(7):CD010033.
4 Below are key images from a neonatal MRI performed for a congenital abnormality.
|
Based on the above images, what is the most appropriate diagnosis?
A. Microform holoprosencephaly
B. Semilobar holoprosencephaly
C. Alobar holoprosencephaly
D. Lobar holoprosencephaly
View Answer
4 Answer B. Semilobar holoprosencephaly. The interhemispheric fissure is seen posteriorly with partial fusion of the thalami. The septum pellucidum is absent and >50% of frontal lobes are not separated.
|
Imaging Findings: A large ventricle with absent septum pellucidum (A), presence of partially fused thalami (arrow B), and posteriorly seen interhemispheric fissure (A and C) are present. Findings are suggestive of semilobar holoprosencephaly.
Discussion: Holoprosencephaly (HPE) is the most common developmental malformation of the CNS. It has a multifactorial etiology with chromosomal/genetic causes, syndromic associations, exposure to teratogens, maternal diabetes, alcohol, and smoking. It can vary from minimal or microform subtypes with no to minimal anatomic defects on MRI to alobar, the most severe and lethal variant. Primary morphologic subtypes of HPE are as follows:
Alobar HPE: complete lack of hemispheric cleavage, characterized by a primitive monoventricle, fused thalami.
Semilobar HPE: partial cleavage with presence of falx or interhemispheric fissure posteriorly, >50% fusion of the frontal lobes and partial fusion of thalami. Anterior mantle of continuous brain parenchyma may be seen.
Lobar HPE: The interhemispheric fissure is nearly completely present with complete or near-complete cleavage of the thalami. The third ventricle and splenium/posterior body corpus callosum may also be present. Septum pellucidum is absent, and inferior frontal lobes may be fused.
Middle interhemispheric HPE: lack of cleavage of posterior frontal and parietal regions, characteristic of vertically oriented sylvian fissures
A dorsal cyst is commonly seen with the alobar form. Differentiation between semilobar and lobar forms may often be difficult, and presence of a rudimentary frontal horn and third ventricle may point toward the latter. Prognosis with this condition is poor. The severity along the spectrum of HPE determines survival with most severe forms being lethal in early childhood/infancy, and milder forms can survive longer, however, with significant developmental delays and morbidity.
Differential Diagnosis: Differential diagnosis is severe hydrocephalus and hydranencephaly. Evaluation of thalamic and hemispheric separation and presence of septum pellucidum can help distinguish from HPE.
Reference: Winter TC, Kennedy AM, Woodward PJ. Holoprosencephaly: a survey of the entity, with embryology and fetal imaging. Radiographics 2015;35(1):275-290.
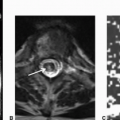
5 Severe ventricular enlargement was noted on CT. MRI was performed for better assessment. Key images are shown below.
|
Based on the above images, what is the most likely diagnosis?
A. Idiopathic normal pressure hydrocephalus
B. Aqueductal stenosis
C. Communicating hydrocephalus
D. Corpus callosal dysgenesis
View Answer
5 Answer B. Aqueductal stenosis. Marked hydrocephalus most severely involving the lateral ventricle with relative sparing of the fourth ventricle is seen. Based on the lack of flow through the cerebral aqueduct on Image A and anatomic obstruction seen within the aqueduct on B, the most appropriate diagnosis is aqueductal stenosis.
|
Imaging Findings: Sagittal phase contrast CSF flow study shows lack of flow through the aqueduct (A) in the setting of prominent enlargement of the third and lateral ventricles (B). There is a soft tissue focus within the aqueduct seen on the sagittal 3D CISS (B).
Discussion: Aqueductal stenosis (AS) is one of the causes of noncommunicating hydrocephalus. It is a triventricular hydrocephalus with dilation of lateral and third ventricle with relative sparing of the fourth ventricle. It can be caused by congenital or acquired obstruction at the level of aqueduct of Sylvius.
Congenital causes:
Aqueductal stenosis: Narrowing is generally focal and can be proximal or distal, more commonly proximal at the level of superior colliculi or intercollicular sulcus. Diffuse narrowing can also be seen (aqueduct atresia). In many cases of narrowing, the aqueduct can be divided into ventral and dorsal columns with several ductules within the dorsal column, known as “forking.”
Aqueductal web/membrane
Aqueductal gliosis: postinflammatory, secondary to perinatal hemorrhage or infection
Acquired causes:
Intrinsic obstruction: adhesion due to hemorrhage, meningitis, ventriculitis
Extrinsic compression: tectal plate glioma, pineal tumor
Imaging features include triventricular dilatation—dilatation of lateral and third ventricles and relatively small/normal-sized fourth ventricle. Relatively small/occluded aqueduct seen on thin/3D fluid-sensitive sequences. Sagittal 3D steady state sequence (FIESTA/CISS) is commonly used for this purpose. There is visible CSF obstruction in the aqueduct (lack of CSF flow-related artifact on T2-weighted images). Cardiac-gated phase contrast CSF flow studies are helpful. Periaqueductal mass may also be seen on MRI, because CT can be insensitive to tectal masses. Periventricular edema is variable, generally present in symptomatic patients.
Differential Diagnosis: Differential diagnosis includes normal pressure hydrocephalus, because it is not uncommon for the fourth ventricle to be smaller in size in NPH. CSF flow studies are helpful in demonstrating presence of flow across the aqueduct in difficult cases.
Endoscopic third ventriculostomy and VP shunting are the treatment options for the hydrocephalus.
References: Aqueduct Stenosis | Radiology Reference Article | Radiopaedia.org. Available at http://radiopaedia.org/articles/aqueduct-stenosis. Accessed on June 10, 2016.
Barkovich AJ, Raybaud C. Pediatric neuroimaging, 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2011.
Harrison MJ, Robert CM, Uttley D. Benign aqueduct stenosis in adults. J Neurol Neurosurg Psychiatry 1974;37(12):1322-1328.
Rumboldt Z, ed. Brain imaging with MRI and CT: an image pattern approach. Cambridge, UK: Cambridge University Press, 2012.
Stoquart-El Sankari S, Lehmann P, Gondry-Jouet C, et al. Phase-contrast MR imaging support for the diagnosis of aqueductal stenosis. AJNR Am J Neuroradiol 2009;30(1):209-214. doi: 10.3174/ajnr.A1308.
6 An infant presents with recurrent apneic spells thought to be seizures. Further workup reveals abnormal brain MRI. Key images are shown below.
|
6a What is the most likely diagnosis?
A. Lissencephaly
B. Hemimegalencephaly
C. Schizencephaly
D. Dyke-Davidoff-Masson syndrome
View Answer
6a Answer B. Hemimegalencephaly. There is enlargement of the right cerebral hemisphere with a dysmorphic right lateral ventricle and areas of abnormal cortical thickening and gyral pattern.
6b What is the characteristic abnormality in the above disorder?
A. Cerebral hemiatrophy
B. Hamartomatous overgrowth
C. Absence of cortical gyration
D. Small ipsilateral ventricle
View Answer
6b Answer B. Hamartomatous overgrowth. Hamartomatous overgrowth of one hemisphere or part of it with associated neuronal migration anomalies are characteristic abnormalities seen with this disorder. Cerebral hemiatrophy is seen with Dyke-Davidoff-Masson syndrome. Absence of cortical gyration is seen with lissencephaly (smooth cortical surface). This disorder can have enlargement of ipsilateral ventricle; however, some cases may show smaller ipsilateral ventricle.
|
Imaging Findings: There is enlargement of the right cerebral hemisphere with dysmorphic appearance of the right lateral ventricle. Broadening of gyri with thickened cortical mantle is also noted in the right frontal and parietooccipital cortices (arrows B). These findings are most consistent with hemimegalencephaly.
Discussion: Hemimegalencephaly is a congenital developmental condition characterized by hamartomatous overgrowth of one or part of a hemisphere with associated neuronal migrational anomalies as is evident in the form of pachygyria-polymicrogyria along with unilateral hemispheric enlargement.
There is no gender predilection. The disease can be isolated or part of a syndrome such as tuberous sclerosis, or NF type 1. Typically hemispheric, rarely, total hemimegalencephaly can involve unilateral hemisphere, with ipsilateral brainstem and cerebellum. There may be characteristic enlargement of the frontal horn of the lateral ventricle although the ipsilateral ventricle enlargement is less pronounced compared to the rest of the involved hemisphere. Some patients may even have smaller ipsilateral ventricle. Agyria, pachygyria, and polymicrogyria may be associated with this condition.
Clinically, patients have severe developmental delay, refractory seizures, and hemiplegia/hemianopia. Prognosis is poor because of significant neurologic dysfunction. Primary goal of management is seizure control for which antiepilepsy drugs are used. In patients with refractory epilepsy anatomic or functional hemispherectomy can be performed.
Reference: Broumandi DD, Hayward UM, Benzian JM, et al. Best cases from the AFIP: hemimegalencephaly. Radiographics 2004;24(3):843-848.
7 An MRI was performed for characterization of a congenital abnormality. Key image is shown below.
|
7a The congenital abnormality in the above image is a result of which of the following embryologic malformations?
A. Aplasia or hypoplasia of the cerebellar vermis
B. Partial fusion of the cerebellar hemispheres
C. Formation of a cerebellar cleft
D. Formation of a retrocerebellar cyst
View Answer
7a Answer A. Aplasia or hypoplasia of the cerebellar vermis. This image shows wide opening of the fourth ventricle and absence of a cerebellar vermis. This appearance is characteristic of Dandy-Walker malformation.
7b Which of the following clinical features is highly prevalent with this condition?
A. Micrognathia
B. Microcephaly
C. Craniofacial anomalies
D. Macrocephaly
View Answer
7b Answer D. Macrocephaly. Macrocephaly is the most common clinical feature associated with Dandy-Walker malformation present in >90% of infants with this condition.
|
Imaging Findings: Wide opening of the fourth ventricle seen along the posterior edge continuous with a posterior fossa cystic space. No vermis is identified. The cerebellar hemispheres are maintained without evidence of hypoplasia or fusion. This appearance is characteristic of Dandy-Walker malformation.
Discussion: Dandy-Walker malformation shown here is characterized by abnormal vermian development. The vermis is either absent or profoundly hypoplastic. There is associated dilation of the fourth ventricle with a large opening into a cystic posterior fossa space as shown here. The tentorium may be elevated because of a large posterior fossa. These patients may have associated hydrocephalus that can benefit from early shunting. Developmental delay, seizures, mental retardation, and macrocephaly are common clinical manifestations. Macrocephaly is the most common clinical manifestation association with this condition and can be seen early in infancy.
Reference: Abdel Razek AA, Castillo M. Magnetic resonance imaging of malformations of midbrain-hindbrain. J Comput Assist Tomogr 2016;40(1):14-25.
8 Key images from an MRI performed for evaluation of refractory seizures are shown.
|
What is the most striking abnormality on MRI in this patient who also had an abnormal EEG?
A. Subependymal nodular heterotopia
B. Subcortical dysmyelination
C. Subcortical band heterotopia
D. Bifrontal focal cortical dysplasia
View Answer
8 Answer C. Subcortical band heterotopia.
|
Imaging Findings: There is curvilinear subcortical band of abnormal signal that is isointense to gray matter on all sequences, most compatible with subcortical laminar heterotopia.
Discussion: Subcortical band heterotopia (SBH), also referred to as “double cortex,” is a congenital neuronal migration disorder associated with abnormal gray matter settling underneath the cortex separated from the cortex by a thin layer of white matter. The thickness of the abnormal subcortical gray matter can vary from thin curvilinear to a thick band of tissue. Subcortical band heterotopia (SBH) is classified with lissencephaly complex (agyria-pachygyria) and not with the other heterotopias. SBH may result from less severe mutations of DSX or LIS1 gene, in addition, a genetic defect on X chromosome in the gene that codes for doublecortin is implicated in some of the cases. Based on the extent of abnormality on the spectrum, the patient can be asymptomatic or have seizures and intellectual impairment.
The most common form of heterotopias is subependymal or periventricular heterotopia, typically the nodular form. These heterotopias due to abnormal neuronal migration can be classified as follows:
Subependymal (periventricular) heterotopia
Subcortical nodular heterotopia (not the band type; note that SBH is classified with lissencephaly as a part of the classic lissencephaly spectrum)
Marginal glioneuronal heterotopia (or sometimes referred to as leptomeningeal heterotopias). This is a rare entity, with glioneuronal proliferations overlying the cortex and protruding into the subarachnoid spaces.
References: Barkovich AJ, Kuzniecky RI, Jackson GD, et al. Classification system for malformations of cortical development: update 2001. Neurology 2001;57(12):2168-2178.
Guerrini R, Parrini E. Neuronal migration disorders. Neurobiol Dis 2010;38:154-166.
Nalbantoglu M, Erturk-Cetin O, Gozubatik-Celik G, et al. The diagnosis of band heterotopia. Pediatr Neurol 2014;51(1):178-180.
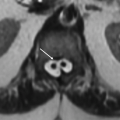
9 Based on the following image, what is the most likely diagnosis?
|
9a What is the most likely diagnosis?
A. Porencephalic cyst
B. Open-lip schizencephaly
C. Closed-lip schizencephaly
D. Cystic encephalomalacia
9b Which of the following is a key feature of this diagnosis?
A. Cleft lined by gray matter
B. Cleft lined by white matter
C. Cleft without ependymal communication
D. Presence of a cyst wall
View Answer
9b Answer A. Cleft lined by gray matter. It is a key feature for diagnosis.
|
Imaging Findings: A large open cleft-like defect that communicates with the ventricle (arrow) and pial surface and is lined by gray matter. This is most compatible with open-lip schizencephaly. If the loss of brain tissue is minimal and the cleft walls are apposed, it is termed as closed-lip schizencephaly.
Discussion: Schizencephaly is a disorder of cortical malformation characterized by a gray matter-lined cleft that communicates with pial and ependymal lining. Depending on the amount of loss of neural tissue, the cleft can be wide as in this case, referred to as open-lip schizencephaly or minimal with apposed walls, namely, closed-lip schizencephaly. In the latter, the demonstration of ependymal communication may be challenging, and usually, an outward dimple is noted in the ventricle wall. This can be associated with subependymal heterotopia usually adjacent to the ependymal continuation and juxtaposed dysplastic cortical gyri. These are usually unilateral; however, one-third of the cases are bilateral. These are most common in the frontal or frontoparietal lobes. This is a rare abnormality and often found in conjunction with polymicrogyria. Depending on the severity of defect, the patients may be neurologically intact to profound neurologic defects, mental retardation, and developmental delay. Nearly all patients have epilepsy.
References: Barkovich AJ, Guerrini R, Kuzniecky RI, et al. A developmental and genetic classification for malformations of cortical development: update 2012. Brain 2012;135(Pt 5):1348-1369. doi: 10.1093/brain/aws019.
Barkovich AJ, Raybaud CA. Neuroimaging in disorders of cortical development. Neuroimaging Clin N Am 2004;14(2):231-254.
Hayashi N, Tsutsumi Y, Barkovich AJ. Morphological features and associated anomalies of schizencephaly in the clinical population: detailed analysis of MR images. Neuroradiology 2002;44(5):418-427.
10
|
10a What is the key finding seen on this image that distinguishes this entity from other morphologically similar conditions?
A. Peripheral cortical location
B. Contact with the pial surface
C. White matter lining the cyst wall
D. Scalloping of the calvarium
View Answer
10a Answer C. White matter lining the cyst wall. The white matter lining is typically seen with porencephalic cyst as in this case, distinguishing it from schizencephaly.
10b What is the most likely diagnosis?
A. Porencephalic cyst
B. Open-lip schizencephaly
C. Closed-lip schizencephaly
D. Hydranencephaly
View Answer
10b Answer A. Porencephalic cyst. The lack of gray matter lining the cyst wall differentiates this from schizencephaly. Hydranencephaly on the other hand is much more severe with profound loss of brain tissue and a large fluid-filled cavity.
|
Imaging Findings: Right parietal parasagittal cystic cavity without any septations or internal complexity. It is lined by nongliotic white matter (arrow) with thinning of the overlying cortex.
Discussion: Porencephaly refers to CSF-containing cavity that replaces normal brain parenchyma.
Porencephaly, multicystic encephalomalacia, and hydranencephaly are related entities, with differences in age of the patient at the time of insult and also the degree of insult. Rarely, a familial form is seen because of COL4A1 mutation encoding type IV collagen, basement membrane component, resulting in porencephalic cyst, intracranial hemorrhages, and aneurysms.
The typical porencephalic cyst, also known as an encephaloclastic porencephaly or type I porencephaly, results from insult after late second trimester. These are smooth-walled cavities with no or only minimal surrounding gliosis.
Hydranencephaly refers to an extreme form of bilateral porencephaly and is due to disruption of the fetal anterior circulation and destruction of the developing cerebral hemispheres. Each cerebral hemisphere is replaced by a large fluid-filled sac covered by thin meninges.
When the insult occurs late in gestation or at/after birth, there is generally more pronounced astroglial reaction and CSF-filled cavities are multiple with shaggy walls and septations. This is referred to as multicystic encephalomalacia.
The porencephalic cyst typically results from vascular insult or is infectious in etiology. Acquired cysts can also happen from injury late in life and are usually secondary to trauma, surgery, ischemia, or infarction. Most common etiology is felt to be periventricular hemorrhagic infarction, either arterial or venous. The location of the lesion varies with the nature of the insult. If it is secondary to vascular insult, the lesion is seen in vascular distribution. Injury resulting from mild to moderate hypotension tends to be in watershed areas. With severe hypotension, only the immediate periventricular white matter may be spared. If hypoglycemia is the inciting event, lesions tend to be in parietal and occipital lobes. With infection, the site is nonspecific, reflecting the region of brain involvement by infection.
On imaging, cystic degeneration develops 7 to 30 days after the insult. The cavities can be unilateral or bilateral and cortical or subcortical and usually, although not invariably, communicate directly with the ventricular system. The wall is smooth with no or only minimal surrounding gliosis. The content of cyst is isointense to CSF on all MR sequences. Wallerian degeneration can be evident in distant white matter tracts.
Differential Diagnosis: Differential diagnosis includes arachnoid cyst (extra-axial in location; no changes in the adjacent brain parenchyma), ependymal cyst (intraventricular; no changes in the adjacent brain parenchyma), and neuroglial cyst (intra-axial; typically, no changes in the adjacent brain parenchyma, no evidence for distant wallerian degeneration, and does not communicate with the ventricular system). Occasionally, it may be difficult to differentiate a small porencephalic cyst from this entity.
References: Barkovich AJ, Raybaud C. Pediatric neuroimaging, 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2011.
Durrani-Kolarik S, Manickam K, Chen B. COL4A1 mutation in a neonate with intrauterine stroke and anterior segment dysgenesis. Pediatr Neurol 2017;66:100-103.
Naidich TP, ed. Imaging of the brain. Expert radiology series. Philadelphia, PA: Saunders/Elsevier, 2013.
Osborn AG, Preece MT. Intracranial cysts: radiologic-pathologic correlation and imaging approach. Radiology 2006;239(3):650-664. doi: 10.1148/radiol.2393050823.
11 A 35-year-old female presented with post-LP headache and photophobia. Key images from an MRI are shown below.
|
11a What is the most likely diagnosis in the current clinical setting?
A. Meningoencephalitis
B. Bifrontal subdural empyema
C. Chiari 1 malformation
D. Intracranial hypotension
View Answer
11a Answer D. Intracranial hypotension. Diffuse pachymeningeal enhancement is seen throughout the brain and partially imaged upper cervical cord. Note bilateral L>R subdural effusions and presence of mild downward displacement of the cerebellar tonsils, depression of the floor of third ventricle, and narrowed appearance of the fourth ventricle. In the provided clinical setting, these findings are compatible with intracranial hypotension.
11b What is the most likely explanation for the pachymeningeal enhancement seen with this entity?
A. Congenital developmental anomaly
B. Dural venous engorgement
C. Infection related to nonsterile puncture technique
D. Reactive because of chronic subdural hematoma
View Answer
11b Answer B. Dural venous engorgement. The dural enhancement seen in these patients is thought to have resulted from venous engorgement and not infection, trauma, or any congenital abnormality.
|
Imaging Findings: Diffuse pachymeningeal enhancement is seen (arrows A) on axial postcontrast T1w image. On sagittal T1w, there is depression of the floor of third ventricle (dotted arrow, B) and mild tonsillar descent (arrow B). Bilateral L>R, subdural effusions are also seen on T2w axial image (C). These findings in the current clinical setting are consistent with intracranial hypotension.
Discussion: Intracranial hypotension (ICH) can be spontaneous or acquired, the common causes being a lumbar puncture, surgery, and trauma. It typically presents as orthostatic headache, although nonpositional and exertional headaches have been reported. In addition to headaches, symptoms include neck stiffness, tinnitus, hyperacusis, photophobia, and nausea, as well as a wide variety of cranial nerve symptoms. Rarely, symptoms can be severe, even resulting in coma.
The etiology for spontaneous ICH is commonly CSF leak in the spine, cervicothoracic spine being the most common location. Perineural cyst/dural diverticula are the common sites of the leak. Connective tissue disorders can also predispose to spontaneous CSF leak.
CSF opening pressure of <6 cm of water is considered low pressure. However, opening pressures are not always obtained and are not completely reliable in patients with intracranial hypotension. Given the lack of baseline, pressures can also be within the normal range in patients. Imaging is the mainstay for diagnosis.
Many of the imaging features can be explained by the Monro-Kelly hypothesis, which states that the volume in intracranial compartment is constant and a fall in CSF volume results in compensatory enlargement of venous and arterial structures and formation of subdural collections. Each of the various imaging features by themselves is nonspecific and can be seen in other intracranial pathologies. However, a combination of findings is reliable for the diagnosis of intracranial hypotension. Imaging may be negative in a small percentage.
Findings on the unenhanced CT scan can be subtle, with subdural fluid collections being the most prominent feature, and effacement of basal cisterns, small sulci, and ventricles can be seen.
MRI is the investigation of choice for the diagnosis of ICH. Diffuse pachymeningeal thickening with intense enhancement is the most common feature, seen in over 80% of patients. This is secondary to venous engorgement in the dura. Engorged vertebral venous plexus in the cervical spinal canal is also a common finding. Subdural fluid collections (commonly hygromas, rarely hematomas) can be seen and are commonly bilateral. Distended dural venous sinuses and pituitary engorgement are commonly present. In more severe cases, sagging brainstem is seen, with midbrain displaced below the level of the dorsum sella, reduced pontomamillary distance, and flattening of the pons against the clivus. Tonsillar displacement can also be seen, which can mimic the appearance of Chiari malformation. Optic chiasm and hypothalamus can be seen stretched and draped over the sella.
Additional imaging to identify the actual site of leak can be undertaken, especially in patients not improving on conservative treatment (fluid replacement, bed rest, epidural blood patch). Contrast-enhanced MRI of the entire spine and dynamic CT myelogram are the commonly performed tests for this purpose.
References: Cauley KA, Fulwadhva U, Dundmadappa SK. Apparent diffusion coefficient measurements to support a diagnosis of intracranial hypotension. Br J Radiol 2014;87(1040):20140131. doi: 10.1259/bjr.20140131.
Osborn AG. Osborn’s brain: imaging, pathology, and anatomy, 1st ed. Salt Lake City, UT: Amirsys Pub, 2013.
Rumboldt Z, ed. Brain imaging with MRI and CT: an image pattern approach. Cambridge, UK: Cambridge University Press, 2012.
12 Key images from an MRI of a child with cerebral palsy born preterm with congenital heart disease are provided below.
|
12a What is the most likely diagnosis?
A. No abnormality is noted.
B. Periventricular leukomalacia
C. Colpocephaly
D. Tuberous sclerosis
12b What is the most likely etiologic factor for this appearance in the provided clinical setting?
A. Hypoxic-ischemic white matter injury
B. Congenital neuronal migration abnormality
C. Antenatal CMV exposure
D. Gestational diabetes
View Answer
12b Answer A. Hypoxic-ischemic white matter injury.
|
Imaging Findings: There is periventricular white matter volume loss and signal changes on FLAIR and T1 suggestive of gliosis with wavy margin of the lateral margin. Findings are compatible with periventricular leukomalacia in the current clinical setting.
Discussion: Periventricular leukomalacia refers to a pattern of white matter injury as a result of mild to moderate hypoxic-ischemic injury usually in the premature brain.
This is thought to be because of increased vulnerability of the oligodendrocyte precursor cells to oxidative stress from hypoxic-ischemic injury. Low cerebral vascularity has been shown in the affected periventricular regions. Motor and visual impairment are typical clinical manifestations.
Early in the course of disease, there is periventricular restricted diffusion, followed later in disease by T2 hyperintensity and subsequently by cavitation, necrosis, and cyst formation and ultimately by volume loss. There is also ventricular enlargement, with wavy contours of the lateral ventricle. These changes are most commonly present abutting the lateral ventricle in the peritrigonal region and in the region of the foramen of Monro. This causes an overlap with terminal zone of myelination (TZM); however, TZM T2 hyperintensity is separated from the ependymal margin by a thin band of T2 low signal unlike PVL that extends up to the ventricular ependymal.
On US, four stages of PVL are seen (stage 1, globular areas of increased echogenicity within 48 hours followed by transient normalization seen between 2nd and 4th weeks). Periventricular cyst formation occurs at 3 to 6 months and finally end stage with resolution of cysts, periventricular volume loss, and ventricular enlargement.
MRI shows periventricular white matter foci T1 hyperintensity surrounded by T2 hyperintensity at 3 to 4 days. Subsequently, there is T2 hypointensity with some cases showing foci of hemorrhage. End-stage PVL shows volume loss in the periventricular white matter and centrum semiovale and dilation of the trigones with an irregular ventricular outline. Thinning of corpus callosum posterior body and splenium may also be present.
References: Back SA. Perinatal white matter injury: the changing spectrum of pathology and emerging insights into pathogenetic mechanisms. Ment Retard Dev Disabil Res Rev 2006;12(2):129-140.
Chao CP, Zaleski CG, Patton AC. Neonatal hypoxic-ischemic encephalopathy: multimodality imaging findings. Radiographics 2006;26(Suppl 1):S159-S172.
de Vries LS, Benders MJ, Groenendaal F. Progress in neonatal neurology with a focus on neuroimaging in the preterm infant. Neuropediatrics 2015;46(4):234-241.
Huang BY, Castillo M. Hypoxic-ischemic brain injury: imaging findings from birth to adulthood. Radiographics 2008;28(2):417-439.
Varghese B, Xavier R, Manoj VC, et al. Magnetic resonance imaging spectrum of perinatal hypoxic-ischemic brain injury. Indian J Radiol Imaging 2016;26(3):316-327.
A. Polymicrogyria
B. Ependymoma
C. Focal cortical dysplasia
D. Gray matter heterotopia
View Answer
13a Answer C. Focal cortical dysplasia. The images demonstrate findings most consistent with focal cortical dysplasia (FCD) type IIB.
13b Which of the following is a characteristic imaging feature for this entity?
A. Blurring of the gray-white matter junction
B. Gray matter signal intensity on all pulse sequences
C. Mass effect and vasogenic edema
D. Cortical thinning
View Answer




13b Answer A. Blurring of the gray-white matter junction. Blurring of gray and white matter junction is seen with this entity.
|
Imaging Findings: Axial (A) and coronal (B) FLAIR images and coronal T1-weighted image (C) are shown. FLAIR images demonstrate focal high-signal abnormality in the cortex and subjacent white matter of the right parietal lobe with a funnel-shaped configuration toward the ventricular margin. T1-weighted image highlights the focal loss of sharp gray-white matter junction in the right parietal lobe with blurring of this junction.
Discussion: Focal cortical dysplasias (FCD) are a heterogeneous group of abnormalities related to neuronal disorganization. The etiology is multifactorial and likely a result of in utero insults involving the fifth layer of the cerebral cortex. Patients typically present with intractable seizures with onset in childhood or early adulthood. Histologically, there may be heterotopic neurons in the white matter, deranged cortical lamination, giant and dysmorphic neurons, and balloon cells (large cells containing a large cytoplasm).
A classification is proposed by the Diagnostic Method Commission of the International League against Epilepsy (ILAE). FCD type I is characterized by abnormal cortical lamination, whereas FCD type II is characterized by dysmorphic neurons without (IIA) or with (IIB) balloon cells. FCD type III is associated with a principal lesion such as hippocampal sclerosis (IIIA), glial or glioneuronal tumor (IIIB), vascular malformation (IIIC), or sequela of trauma, ischemia, and infection (IIID).
Imaging studies of affected patients with FCD with balloon cells (FCD IIB) are characteristic. The region involved is usually small. The key findings are focal cortical thickening, T2 signal increase in the cortex, focal loss of the gyral architecture, excessive depth of a sulcus as compared with its contralateral homolog, blurring of the cortical-white matter junction, and T2 prolongation of the underlying white matter. In many patients, a linear, curvilinear, or funnel-shaped focus of abnormal signal intensity can be identified extending from the cortical-white matter junction to the superolateral margin of the lateral ventricular surface (“transmantle dysplasia”), which is practically pathognomonic of FCD type IIB.
The transmantle dysplasia characteristic of type IIB FCD is never found in FCD type I. The brain may appear normal in 20% to 25% of FCD type I and FCD type IIA; therefore, it is important to recognize that a normal brain MRI does not exclude an FCD. Other imaging studies, such as interictal and ictal single photon emission computed tomography (SPECT), positron emission tomography (PET), or magnetoencephalography (MEG), may be helpful in detecting the seizure focus when MRI is negative.
Differential Diagnosis: Differential diagnosis includes polymicrogyria, a disorder of cortical organization characterized by irregular cortical contour; shallow anomalous sulci; normal or apparent thickening of the cortex that is isointense to normal cortex; and irregular nodular gray-white matter junction. Slowly growing indolent cortically based neoplasms such as gangliomas and dysembryoplastic neuroepithelial tumors (DNET) also present with seizures and can appear similar to or can be associated with FCD. Gray matter heterotopias are collections of gray matter nodules outside the cortex and deep gray matter structures, are associated with seizures, and are isointense to gray matter on all pulse sequences.
References: Blümcke I, et al. The clinicopathologic spectrum of focal cortical dysplasias: a consensus classification proposed by an ad hoc Task Force of the ILAE Diagnostic Methods Commission. Epilepsia 2011;52(1):158-174.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree