• A chronic progressive transmural granulomatous inflammatory bowel disease • There are typically discontinuous (‘skip’) lesions with asymmetrical bowel wall involvement • It can affect any part of the GI tract – however it almost always affects the terminal ileum (in 95% of cases) • Inflammatory polyps (pseudopolyps): small, discrete round filling defects • Thickened valvulae conniventes: they can also be distorted, blunted or flattened (they are due to hyperplasia of the lymphoid tissue which causes an obstructive lymphoedema) • Fistulae formation: this can involve adjacent loops of ileum, caecum or sigmoid colon • Bowel wall sacculation: this is secondary to fibrosis within healing eccentric ulcers – NECT: the stratified appearance is due to a thickened muscularis mucosae and submucosal fatty infiltration – CECT: the stratified appearance is due to acute inflammation with submucosal oedema and enhancement of the mucosa and muscularis propria • Although any part of the GI tract can be involved, the ileum is the commonest involved site (esp. the terminal ileum and ileocaecal junction) • Discrete transverse and circumferential ulcers, mucosal fold thickening and strictures are the main radiological features • Ulcerative, hypertrophic or fibrotic forms are described: • Fleischner sign: a thickened patulous ileocaecal valve seen in conjunction with a narrowed terminal ileum • Stierlin’s sign: this is due to rapid emptying of contrast through a gaping incompetent ileocaecal valve and into a conically contracted caecum • A submucosal mesenchymal (non-epithelial) tumour appearing to arise from the muscularis propria • The commonest gastrointestinal mesenchymal tumour (< 1% of all GI tract tumours) • Location: stomach (40–70%) > small intestine (20–50%) > large intestine and rectum (5%) • 90% of tumours will express KIT (CD 117) which is a tyrosine kinase growth factor receptor • Increased prevalence of GIST with NF-1 • Unfavourable prognostic signs: tumour size >5cm • Carney’s triad: a genetic syndrome of young women
Small bowel
CROHN’S DISEASE (CD)
CROHN’S DISEASE
DEFINITION
RADIOLOGICAL FEATURES
Barium studies
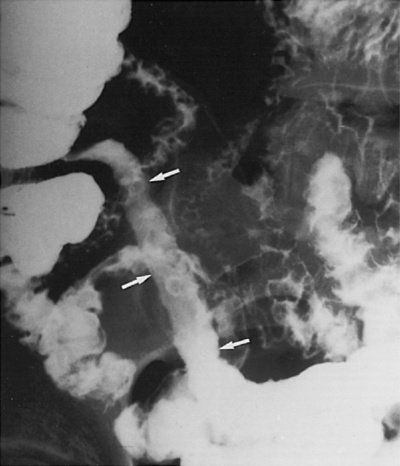
 Aphthoid ulcers: characteristic superficial ulcers that do not penetrate the muscularis mucosa
Aphthoid ulcers: characteristic superficial ulcers that do not penetrate the muscularis mucosa  they appear as small collections of barium with surrounding radiolucent oedematous margins
they appear as small collections of barium with surrounding radiolucent oedematous margins  en face they appear as a dense amorphous barium pool with a surrounding black halo
en face they appear as a dense amorphous barium pool with a surrounding black halo
 Fissuring ‘rose thorn’ ulcers: deep ulcers with penetrating thorn-like cuts into the thickened intestinal wall
Fissuring ‘rose thorn’ ulcers: deep ulcers with penetrating thorn-like cuts into the thickened intestinal wall  they may lead to abscess formation, sinuses or fistulae
they may lead to abscess formation, sinuses or fistulae
 Longitudinal ulcers: these run along the ileal mesenteric border
Longitudinal ulcers: these run along the ileal mesenteric border
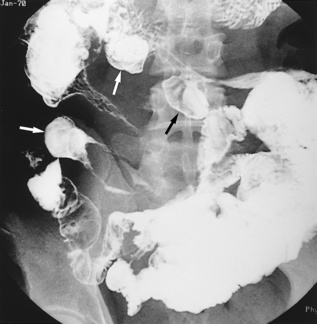
 ‘Cobblestone’ mucosa: a combination of longitudinal and transverse ulceration separating intact portions of mucosa
‘Cobblestone’ mucosa: a combination of longitudinal and transverse ulceration separating intact portions of mucosa
 these are not a frequent finding
these are not a frequent finding
 Thickened bowel wall segments will displace adjacent barium-filled loops
Thickened bowel wall segments will displace adjacent barium-filled loops
 Occasionally a smooth featureless outline will replace the normal mucosal pattern without a significant calibre change
Occasionally a smooth featureless outline will replace the normal mucosal pattern without a significant calibre change
 ‘Skip lesions’: discontinuous involvement of the bowel wall
‘Skip lesions’: discontinuous involvement of the bowel wall
 ‘Pseudodiverticula’: these are due to asymmetrical wall involvement and represent small patches of normal intestine in an otherwise severely involved segment
‘Pseudodiverticula’: these are due to asymmetrical wall involvement and represent small patches of normal intestine in an otherwise severely involved segment
 These may be short, long, single or multiple (the latter is virtually diagnostic of CD)
These may be short, long, single or multiple (the latter is virtually diagnostic of CD)  solitary strictures are common and may be accompanied by proximal (prestenotic) dilatation
solitary strictures are common and may be accompanied by proximal (prestenotic) dilatation
 ‘String sign’: tubular narrowing of the intestinal lumen secondary to oedema and spasm (± scarring)
‘String sign’: tubular narrowing of the intestinal lumen secondary to oedema and spasm (± scarring)
 Other sites: urinary bladder
Other sites: urinary bladder  perianal region (leading to a ‘watering can’ perineum)
perianal region (leading to a ‘watering can’ perineum)  occasionally the skin and vagina
occasionally the skin and vagina
 it can also be seen with ischaemic strictures or scleroderma (with wide ‘square’-shaped diverticulae)
it can also be seen with ischaemic strictures or scleroderma (with wide ‘square’-shaped diverticulae)
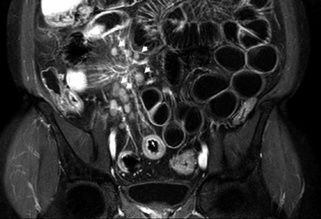
CT
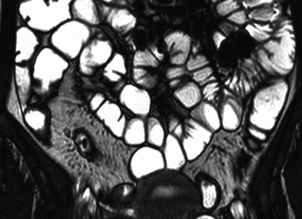
 The transmural disease leads to greater wall thickening than seen with UC
The transmural disease leads to greater wall thickening than seen with UC  mild reactive adenopathy (<1cm) can be present
mild reactive adenopathy (<1cm) can be present
 ‘Dirty fat’: transmural inflammation of the small bowel usually involves the adjacent mesentery
‘Dirty fat’: transmural inflammation of the small bowel usually involves the adjacent mesentery
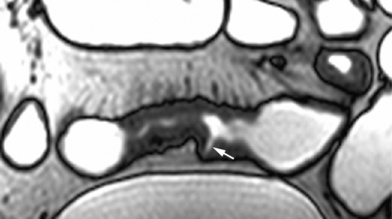
 ‘Target’ or ‘halo’ sign: a homogeneous or stratified appearance is seen on both NECT and CECT:
‘Target’ or ‘halo’ sign: a homogeneous or stratified appearance is seen on both NECT and CECT:
 Mesenteric fibrofatty proliferation: this results in increased CT attenuation
Mesenteric fibrofatty proliferation: this results in increased CT attenuation  it is the most common cause of bowel loop separation in CD
it is the most common cause of bowel loop separation in CD
 ‘Creeping fat’: fat accumulates on the serosal surfaces
‘Creeping fat’: fat accumulates on the serosal surfaces
 ‘Comb’ sign: mesenteric hypervascularity manifested as tortuosity, prominence and dilatation of the mesenteric arterial branches with a wide arrangement of the vasa recta
‘Comb’ sign: mesenteric hypervascularity manifested as tortuosity, prominence and dilatation of the mesenteric arterial branches with a wide arrangement of the vasa recta
 Advanced disease: intestinal perforation may lead to mesenteric phlegmon or interloop abscess formation
Advanced disease: intestinal perforation may lead to mesenteric phlegmon or interloop abscess formation  these may contain gas – this is usually due to enteric or cutaneous fistulae and sinus tracts rather than due to a gas-producing bacteria
these may contain gas – this is usually due to enteric or cutaneous fistulae and sinus tracts rather than due to a gas-producing bacteria
INFECTIONS/INFESTATIONS OF THE SMALL BOWEL
TUBERCULOSIS (TB)
Radiological features
 there are often multiple bowel lesions
there are often multiple bowel lesions
Barium follow through (ileocaecal tuberculosis)
 Ulcerative: there are discrete ulcers with a ‘shaggy’ edge – these tend to be large and circumferential
Ulcerative: there are discrete ulcers with a ‘shaggy’ edge – these tend to be large and circumferential
 Hypertrophic: this presents as an inflammatory mass with associated bowel stenosis
Hypertrophic: this presents as an inflammatory mass with associated bowel stenosis  it may be difficult to distinguish from lymphoma
it may be difficult to distinguish from lymphoma
GASTROINTESTINAL STROMAL TUMOURS (GISTs) AND CARCINOID TUMOURS
GASTROINTESTINAL STROMAL TUMOURS (GISTs)
Definition
 GISTs may arise from the interstitial cells of Cajal (these serve a gastric pacemaker function)
GISTs may arise from the interstitial cells of Cajal (these serve a gastric pacemaker function)
 leiomyomas and leiomyosarcomas are rare at these sites
leiomyomas and leiomyosarcomas are rare at these sites
Pearls
 this differentiates a GIST from other gastrointestinal mesenchymal tumours (e.g. leiomyoma or leiomyosarcoma)
this differentiates a GIST from other gastrointestinal mesenchymal tumours (e.g. leiomyoma or leiomyosarcoma)
 infiltration into adjacent organs
infiltration into adjacent organs  metastases
metastases  a high mitotic and proliferation index
a high mitotic and proliferation index
CARCINOID TUMOURS OF THE GASTROINTESTINAL TRACT
Clinical presentation


 ulceration
ulceration  cobblestoning
cobblestoning  a ‘target’ appearance
a ‘target’ appearance  fibrofatty proliferation
fibrofatty proliferation  vascular engorgement
vascular engorgement  adenopathy
adenopathy  luminal narrowing and stenosis
luminal narrowing and stenosis
 spondylitis
spondylitis  symmetrical sacroilitis
symmetrical sacroilitis  renal stones
renal stones  complications of steroid treatment (e.g. avascular necrosis)
complications of steroid treatment (e.g. avascular necrosis)  primary sclerosing cholangitis
primary sclerosing cholangitis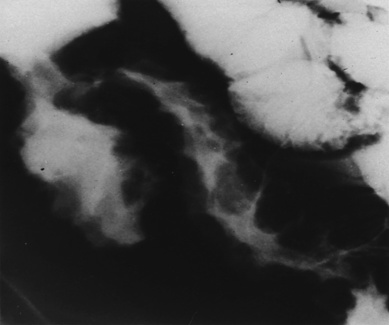



 it used to be secondary to pulmonary disease but is now more likely to be of primary bovine origin (from drinking unpasteurized milk)
it used to be secondary to pulmonary disease but is now more likely to be of primary bovine origin (from drinking unpasteurized milk) liver
liver  spleen
spleen  lymph nodes
lymph nodes  peritoneum
peritoneum  female genital tract
female genital tract fever
fever  weight loss
weight loss  diarrhoea
diarrhoea  intestinal obstruction
intestinal obstruction  bowel perforation (rare)
bowel perforation (rare) there may be enlarged rim enhancing low-density mesenteric nodes (due to caseous liquefaction)
there may be enlarged rim enhancing low-density mesenteric nodes (due to caseous liquefaction) acute inflammation of the terminal ileum is often indistinguishable clinically from an acute appendicitis
acute inflammation of the terminal ileum is often indistinguishable clinically from an acute appendicitis tortuous, thickened mucosal folds with small discrete nodular filling defects of lymphoid hyperplasia
tortuous, thickened mucosal folds with small discrete nodular filling defects of lymphoid hyperplasia  there can be mural thickening
there can be mural thickening the appendix is the most commonly affected site
the appendix is the most commonly affected site previous surgery
previous surgery  neoplasms
neoplasms  diabetes
diabetes  steroids
steroids  poor dental hygiene
poor dental hygiene it is contracted through contaminated drinking water
it is contracted through contaminated drinking water small well-defined nodular lymphoid hyperplasia in patients who also have dysgammaglobulinaemia
small well-defined nodular lymphoid hyperplasia in patients who also have dysgammaglobulinaemia thickened or absent valvulae conniventes within the duodenum and proximal jejunum
thickened or absent valvulae conniventes within the duodenum and proximal jejunum  severe cases may show a rigid ‘pipestem’ stenosis with irregular narrowing
severe cases may show a rigid ‘pipestem’ stenosis with irregular narrowing it may be indistinguishable from Crohn’s disease (although the mucosa remains intact)
it may be indistinguishable from Crohn’s disease (although the mucosa remains intact) it is very commonly seen in the tropics
it is very commonly seen in the tropics there can be associated oesophagitis, gastritis or colitis
there can be associated oesophagitis, gastritis or colitis thickened small bowel folds
thickened small bowel folds





 abdominal pain
abdominal pain  abdominal mass
abdominal mass  ileus
ileus  GI bleeding
GI bleeding  weight loss
weight loss the border of the smooth mucosal surface forms right or obtuse angles with the adjacent mucosa
the border of the smooth mucosal surface forms right or obtuse angles with the adjacent mucosa coarse mottled calcifications (25%)
coarse mottled calcifications (25%)  occasionally pedunculated (and may obstruct the pylorus or duodenum/act as a lead point for an intussusception)
occasionally pedunculated (and may obstruct the pylorus or duodenum/act as a lead point for an intussusception)  hypo- or hypervascular
hypo- or hypervascular T2WI: low to intermediate SI
T2WI: low to intermediate SI  T1WI + Gad: variable heterogeneous enhancement
T1WI + Gad: variable heterogeneous enhancement
 it is multiple in ⅓ of cases
it is multiple in ⅓ of cases it can present with abdominal pain, obstruction, or an abdominal mass
it can present with abdominal pain, obstruction, or an abdominal mass  GI haemorrhage is very rare
GI haemorrhage is very rare





