• Metastatic: the result of abnormal calcium metabolism • Calcinosis: occurring with a normal calcium metabolism • Dystrophic: related to tissue damage • Ossification: bony trabeculae are discernible (either ectopic or heterotropic) • The differential diagnosis is divided into: • Localized intratumoral calcification may occur within any soft tissue tumour due to haemorrhage or necrosis • Benign mineralizing tumours: soft tissue chondroma (punctuate or ‘ring and arc’ calcification) • Malignant mineralizing tumours: extraskeletal osteosarcoma • Developmental causes include fibrodysplasia ossificans progressiva, melorheostosis and progressive osseous heteroplasia • Post-surgical: this particularly occurs following a total hip arthroplasty (± pain and restricted movement) • Haemorrhage is followed by mineralization • Early biopsy should be avoided (as it can resemble a soft tissue osteosarcoma) • It is associated with burns and paraplegia This results from prolonged elevation of the serum calcium (or more importantly serum phosphate) • Primary hyperparathyroidism: calcification is typically seen involving arteries, cartilage (chondrocalcinosis) and periarticular tissues • Secondary hyperparathyroidism: soft tissue and vascular calcification is more common than in primary disease • Hypoparathyroidism: subcutaneous and basal ganglia calcification • Pseudohypoparathyroidism: there are similar features to hypoparathyroidism but it is associated with growth deformities (broad bones, cone epiphyses, short metacarpals and metatarsals – especially the 1st, 4th and 5th) • Pseudopseudohypoparathyroidism: XR features are identical to pseudohypoparathyrodism (but with a normal serum calcium and phosphate) • Hypervitaminosis D: smooth lobulated amorphous calcium hydroxyapatite masses within the periarticular regions, bursae, tendon sheaths and the joint capsule • Mönckeberg’s arteriosclerosis: finer ‘pipe-stem’ calcification seen with medial degeneration • Diabetes: calcification of the small vessels of the feet • Renal failure/hyperparathyroidism: a fine more generalized pattern of arterial calcification • Aneurysms: rounded, curvilinear and crescentic calcification
Soft tissue imaging
LOCALIZED CALCIFICATION AND OSSIFICATION
LOCALIZED CALCIFICATION AND OSSIFICATION
Definition
 calcium deposits tend to be more densely sclerotic than in normal bone
calcium deposits tend to be more densely sclerotic than in normal bone
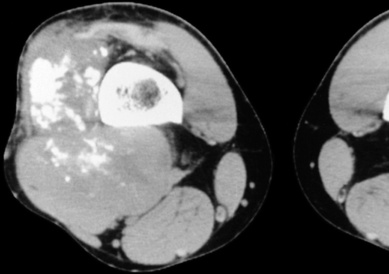
LOCALIZED CALCIFICATION – TUMOURS
Definition
 lipoma (ossification can occur, especially if it is parosteal)
lipoma (ossification can occur, especially if it is parosteal)  haemangiomas (phleboliths)
haemangiomas (phleboliths)
 extraskeletal chondrosarcoma
extraskeletal chondrosarcoma  synovial sarcoma (with a central rather than peripheral distribution)
synovial sarcoma (with a central rather than peripheral distribution)
HETEROTOPIC OSSIFICATION
Definition
 Pellegrini–Stieda lesion: ossification of the medial collateral knee ligament
Pellegrini–Stieda lesion: ossification of the medial collateral knee ligament
 Neurogenic heterotropic ossification: soft tissue ossification associated with CNS injuries (with prolonged unconsciousness and spinal trauma)
Neurogenic heterotropic ossification: soft tissue ossification associated with CNS injuries (with prolonged unconsciousness and spinal trauma)  there is a periarticular distribution (commonly affecting the hips)
there is a periarticular distribution (commonly affecting the hips)  surgery is associated with recurrence
surgery is associated with recurrence
 Avulsion of an ossification centre: in the skeletally immature an avulsed ossification centre may continue to grow
Avulsion of an ossification centre: in the skeletally immature an avulsed ossification centre may continue to grow  this may present later as a large ossified soft tissue mass (commonly affecting the pelvic and hamstring pelvic origins)
this may present later as a large ossified soft tissue mass (commonly affecting the pelvic and hamstring pelvic origins)
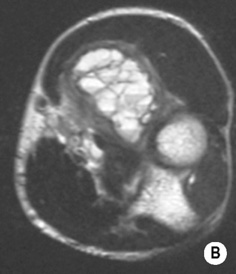
MYOSITIS OSSIFICANS
Definition
 this is first seen in the periphery with a gradual reduction in the size of the mass (which are both helpful in distinguishing from a mineralizing soft tissue sarcoma)
this is first seen in the periphery with a gradual reduction in the size of the mass (which are both helpful in distinguishing from a mineralizing soft tissue sarcoma)
 it is commonly seen around the elbow and in the thigh
it is commonly seen around the elbow and in the thigh
GENERALIZED SOFT TISSUE CALCIFICATION
METABOLIC DISORDERS
Definition
 chondrocalcinosis is infrequent
chondrocalcinosis is infrequent
 osteosclerosis
osteosclerosis  premature epiphyseal closure
premature epiphyseal closure  band-like paraspinal calcification (mimicking DISH)
band-like paraspinal calcification (mimicking DISH)
 dense metaphyseal bands and cortical thickening (± osteosclerosis in children)
dense metaphyseal bands and cortical thickening (± osteosclerosis in children)  osteoporosis in adults
osteoporosis in adults
ARTERIAL CALCIFICATION
Definition





 it is possibly due to haematoma ossification or displacement of periosteal elements into the soft tissues
it is possibly due to haematoma ossification or displacement of periosteal elements into the soft tissues






 it ranges from irregular plaques to extensive tramline calcification (predominantly affecting the aorta, pelvic and lower limb arteries)
it ranges from irregular plaques to extensive tramline calcification (predominantly affecting the aorta, pelvic and lower limb arteries) it is unrelated to myositis ossificans
it is unrelated to myositis ossificans






