Soft Tissue Neck
Syed Adil Aftab
Daniel Thomas Ginat
QUESTIONS
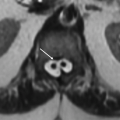
2 Identify the nodal level of the enlarged necrotic right neck lymph node shown on the following image:
|
A. Level III
B. Level IV
C. Level VA
D. Level VB
View Answer
2 Answer C. Level VA.
|
Imaging Findings: The axial CT image shows an abnormal lymph node located posterior to the posterior margin of the left sternocleidomastoid muscle (arrow), indicating that the node must be a level V lymph node. Although the cricoid cartilage is not visible on this image, the thyroid cartilage is evident, indicating that the node is above the level of the cricoid cartilage and therefore is a level VA lymph node.
Discussion: Level I lymph nodes include the submental (IA) and submandibular (IB) lymph node chains. Level IA nodes are between the anterior bellies of the digastric muscles. Level IB nodes are posterolateral to the anterior bellies of the digastric muscles. Level II lymph nodes constitute the internal jugular lymph node chain superior to the hyoid bone, which are anterior or immediately adjacent to the jugular vein (IIA) or posterior to the jugular vein deep to the sternocleidomastoid muscle (IIB). Level III lymph nodes involve the jugular chain between the hyoid and cricoid cartilage, and level IV lymph nodes involve the jugular chain below the cricoid cartilage. Level V is designated as all the lymph nodes of the posterior triangle of the neck (deep and posterior to the sternocleidomastoid muscle and above the clavicle). Level V nodes superior to the cricoid cartilage are designated as VA, whereas those inferior to the cricoid cartilage are designated VB. Level VI lymph nodes are in the space between the hyoid bone and manubrium anterior to the level III and IV nodal stations. Level VII nodes are in the superior mediastinum.
Reference: Forghani R, Yu E, Levental M, et al. Imaging evaluation of lymphadenopathy and patterns of lymph node spread in head and neck cancer. Expert Rev Anticancer Ther 2015;15(2):207-224.
A. Glossopharyngeal nerve
B. Vagus nerve
C. Spinal accessory nerve
D. Hypoglossal nerve
View Answer
3 Answer B. Vagus nerve.
|
Imaging Findings: The axial CT image shows medialization of the posterior left vocal cord margin and dilation of the ipsilateral laryngeal ventricle.
Discussion: Vocal cord paralysis can result from impairment of the recurrent laryngeal branch of the vagus nerve. The nerve loops around the aortic arch on the left side and around the subclavian artery on the right side and courses through the tracheoesophageal grooves bilaterally. Although vocal cord paralysis can be observed on imaging, manifesting as dilation of the piriform sinus and ventricle, as well as medial rotation of the arytenoid, aryepiglottic fold, and posterior vocal cord, the role of imaging is mainly to identify a potential cause of the paralysis, such as tumors, and the field of view should extend from the brainstem to the upper mediastinum.
The glossopharyngeal nerve supplies the stylopharyngeus muscle.
The spinal accessory nerve supplies the sternocleidomastoid muscle and the trapezius muscle.
The hypoglossal nerve supplied the intrinsic tongue muscles.
Reference: Kwong Y, Boddu S, Shah J. Radiology of vocal cord palsy. Clin Radiol 2012;67(11):1108-1114.
A. Masticator space
B. Parapharyngeal space
C. Carotid space
D. Parotid space
View Answer
4 Answer A. Masticator space.
|
Imaging Findings: The axial fat-suppressed T2-weighted MRI shows a mass arising from the left mandible (arrow), which proved to be Ewing sarcoma.
Discussion: The suprahyoid head and neck spaces are subdivided by layers of the deep cervical fascia into the pharyngeal mucosal, parapharyngeal, carotid, parotid, masticator, retropharyngeal, and perivertebral spaces.
The masticator space contains the masseter, lateral pterygoid, medial pterygoid, and temporalis muscles, posterior portion of the mandible and inferior alveolar nerve, and internal maxillary artery. Tumors arising from the masticator space tend to displace the parapharyngeal fat pad medially.
Differential Diagnosis: Differential diagnosis or lesions in this location include inflammatory lesions from odontogenic source, vascular lesions like hemangioma and neoplasms arising from the mandible, trigeminal nerve branches or the muscles of mastication.
Reference: Gamss C, Gupta A, Chazen JL, et al. Imaging evaluation of the suprahyoid neck. Radiol Clin North Am 2015;53(1):133-144.
Fernandes T, Lobo JC, Castro R, Oliveira MI, and Som PM. Anatomy and pathology of the masticator space. Insights Imaging 2013;4(5):605-616.
5 Which of the following statements is true in general about the condition depicted in the image below?
|
A. The abnormality can potentially extend into the mediastinum via the danger space.
B. The abnormality is more common in adults than in children.
C. The abnormality most commonly arises from penetrating trauma.
D. The presence of an enhancing wall does not differentiate this from an effusion.
View Answer
5 Answer A. The abnormality can potentially extend into the mediastinum via the danger space.
|
Imaging Findings: The sagittal contrast-enhanced CT of the neck demonstrates a rim-enhancing fluid collection posterior to the pharynx (arrow), consistent with a retropharyngeal abscess.
Discussion: The retropharyngeal space is located posterior to the pharynx and esophagus and constitutes the true retropharyngeal space, which extends inferiorly to the level of T1 to T6, and the “danger space,” which extends into the mediastinum, down to the level of the diaphragm, allowing abscess in this space to spread inferiorly. Other complications of retropharyngeal abscess include airway and vascular compromise. Retropharyngeal abscesses most commonly arise from rupture of suppurative retropharyngeal lymph nodes and less often from spread of infection from contiguous spaces or penetrating trauma. Because retropharyngeal lymph nodes are more prominent in children, retropharyngeal abscesses are more common in this age group than in adults. On imaging, retropharyngeal abscesses typically appear as convex rim-enhancing fluid collections, as opposed to effusions, which have a bow-tie configuration in cross section and no rim enhancement.
Reference: Hoang JK, Branstetter BF, Eastwood JD, et al. Multiplanar CT and MRI of collections in the retropharyngeal space: is it an abscess? AJR Am J Roentgenol 2011;196(4):W426-W432.
6 The patient presented with neck pain for several weeks. The following CT of the neck without contrast was obtained. What is the most appropriate next step?
|
A. Surgery
B. Treatment with antibiotics
C. MRI of the neck
D. Treatment with NSAIDs
View Answer
6 Answer D. Treatment with NSAIDs.
|
Imaging Findings: The axial CT depicts calcifications in the prevertebral space (encircled), along the bilateral longus colli tendons, related to calcific tendinitis.
Discussion: Calcific tendinitis of the longus colli muscle is an inflammatory reaction to deposition of calcium hydroxyapatite in the tendons of the longus colli muscle. Symptoms develop acutely and include neck pain, fever, dysphagia, odynophagia, and reduced neck range of movement. Inflammatory markers such as erythrocyte sedimentation rate can be elevated. The diagnosis is best made via CT depiction of calcification in the upper prevertebral space, but the degree of symptoms may be unrelated to the amount of calcification. MRI may demonstrate elevated T2 signal in the surrounding soft tissue due to edema. Antibiotics are not indicated for the treatment of calcific tendinitis of the longus colli muscle. Rather, this condition often responds well to conservative management with NSAIDs.
Reference: Eastwood JD, Hudgins PA, Malone D. Retropharyngeal effusion in acute calcific prevertebral tendinitis: diagnosis with CT and MR imaging. AJNR Am J Neuroradiol 1999;19(9):1789-1792.
7 The patient presented with persistent sore throat for several days and new-onset chest pain. Physical examination reveals an inflamed erythematous mucosa with purulent exudate in the tonsils. The following CT of the neck with contrast was obtained. Which of the following is the most appropriate next step?
|
A. Incision and drainage
B. MRI of the neck
C. CT of the chest
D. Treatment with oral antibiotics
View Answer
7 Answer C. CT of the chest.
|
Imaging Findings: The CT of the neck demonstrates thrombus within the left internal jugular vein (arrow) and left oropharyngeal mucosal space edema. A chest CT also showed multiple septic emboli:
|
Discussion: Lemierre syndrome consists of an oropharyngeal infection associated with thrombophlebitis of the adjacent internal jugular vein. Bacteremia and distal septic thromboembolism, most often involving the lung, is a common complication of the syndrome. An oropharyngeal abscess may or may not be present. Classically, Fusobacterium necrophorum is considered to be the most common causative organism, although various other organisms can be responsible. The patient in this scenario presented with chest pain, which should raise the suspicion for pulmonary emboli, prompting further evaluation with a CT of the chest. A neck MRI does not add more information once the findings in the neck have been made on the neck and chest CTs. The infection related to Lemierre syndrome typically requires prolonged therapy with parenteral antibiotics as opposed to oral antibiotics. Incision and drainage are not necessary if there is no neck abscess.
Reference: Nguyen-Dinh KV, Marsot-Dupuch K, Portier F, et al. Lemierre syndrome: usefulness of CT in detection of extensive occult thrombophlebitis. J Neuroradiol 2002;29(2):132-135.
A. Ranula
B. Branchial cleft cyst
C. Thyroglossal duct cyst
D. Laryngocele
View Answer
8 Answer C. Thyroglossal duct cyst.
|
Imaging Findings: The sagittal CT image shows a midline lobulated cystic lesion (arrow) that extends from the tongue base to the anterior neck soft tissues inferior to the hyoid bone.
Discussion: Thyroglossal duct cysts are congenital anomalies that represent segments of the thyroglossal duct that do not regress. They are the most common congenital neck cyst. The lesions can be found in the midline or near the midline from the base of the tongue to the suprasternal region, but occur most commonly just below the level of the hyoid bone. Most lesions are in midline with off midline locations seen more inferiorly.
Reference: Miller MB, Rao VM, Tom BM. Cystic masses of the head and neck: pitfalls in CT and MR interpretation. AJR Am J Roentgenol 1992;159(3):601-607.
9 The following images is from a contrast-enhanced neck CT. Which of the following is the most likely diagnosis?
|
A. Lymphatic malformation
B. Mycobacterial lymphadenitis
C. Papillary thyroid cancer
D. Lymphoma
View Answer
9 Answer C. Papillary thyroid cancer.
|
Imaging Findings: The coronal CT images shows cystic and solid left cervical lymph nodes (arrows) and a mass in the right lobe of the thyroid gland with calcification (encircled).
Discussion: Lymph node metastases from papillary thyroid carcinoma may be the initial manifestation of the cancer and are often cystic with walls that range from thin/imperceptible to thick enhancing nodular. The lesions may be hypervascular, contain septations and calcify. Imaging findings may mimic second branchial cleft cyst.
Reference: Wunderbaldinger P, Harisinghani MG, Hahn PF, et al. Cystic lymph node metastases in papillary thyroid carcinoma. AJR Am J Roentgenol 2002;178(3):693-697.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree