Agatston score
Calcium score categories
Probability of significant CAD
Cardiovascular risk
Recommendations
0
Absent
Very unlikely (<5 %)
Very low
Reassure patient. General guidelines for primary prevention of CV diseases
1–10
Minimal
Very unlikely (<10 %)
Low
General guidelines for primary prevention of CV diseases
11–100
Mild
Mild or minimal coronary stenosis likely
Moderate
Counsel about risk factors modification, strict adherence with primary prevention goals. Daily ASA
101–400
Moderate
Nonobstructive CAD, highly likely, obstructive CAD possible
Moderately high
Institute risk factor modification and secondary prevention goals. Consider exercise testing
>400
Extensive
High likelihood of significant coronary stenosis (>90 %)
High
Institute very aggressive risk factor modification. Consider exercise of pharmacological nuclear stress testing for the detection of inducible ischemia
On the other hand, a very low or negative CAC cannot completely exclude obstructive CAD. This is mainly due for patients with noncalcified plaques, which are typically present in younger patients or young smokers [27, 28]. Furthermore, even despite the known correlation between increased calcium burden, atherosclerosis, and obstructive CAD, a modest only relationship between calcified plaque burden and obstructive CAD could be found [35–37]. Nevertheless, information about CAC improves the pre-coronary computed tomographic angiography (CCTA) probability of obstructive CAD and can help in the interpretation of CCTA since the non-contrast scan used for CAC determination may be able to better demonstrate calcifications than the contrast study used for CCTA [27].
9.3.2 Coronary Computed Tomographic Angiography
CCTA has advanced over the past years as the most accurate tool for noninvasive coronary angiography. Current multi-slice devices coupled with improved acquisition protocols allow robust and reproducible assessment of coronary morphology with high temporal and spatial resolution at rather low-radiation exposure [38–40]. CCTA was shown to obtain high-quality images of the coronary arteries with an average sensitivity for detecting at least one coronary artery with >50 % stenosis of 94 % (range: 75–100 %). On the other hand, specificity falls off compared to the sensitivity with an average value of 77 % (range: 49–100 %) [4, 41]. The corresponding average positive predictive value (PPV) and NPV are 84 % (range: 50–100 %) and 87 % (range: 35–100 %), respectively, and the overall diagnostic accuracy is 89 % (range: 68–100 %) [4, 41].
The robustness of 64-row CCTA for complete visualization of the coronary tree was recently confirmed by two multicenter, single-vendor trials [18, 42].
In the 2008 published Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography (ACCURACY) trial, 230 chest pain patients without known CAD were included and underwent both CCTA and invasive coronary angiography (ICA). On a patient-based model, the sensitivity, specificity, PPV, and NPV to detect ≥50 % or ≥70 % coronary stenosis were 95, 83, 64, and 99 %, respectively, and 94, 83, 48, and 99 %, respectively. However, the specificity was found to be significantly reduced in case of calcium scores ≥400 [18]. The authors concluded that 64-row CCTA possesses a high diagnostic accuracy for the detection of obstructive coronary stenosis at both thresholds of 50 and 70 % stenosis. Furthermore, based on the 99 % NPV, CCTA might be established as an effective noninvasive alternative to ICA to rule out obstructive coronary artery stenosis.
The Coronary Artery Evaluation Using 64-Row Multidetector Computed Tomography Angiography (CORE-64) trial enrolled 291 patients with a prevalence of obstructive CAD of 56 % and CAC scores ≤600. As with in the ACCURACY trial, all patients underwent CCTA and ICA. However, the CORE-64 trial provides additional evidence that is somewhat discordant to the ACCURACY trial and to initial results from single-center studies [42, 43]. On a per-patient basis, a sensitivity for detecting at least 1 coronary artery with ≥50 % stenosis of 85 % was found, which is considerably lower than in single-center studies and in the ACCURACY trial using similar technology [18, 42, 43]. In contrast, the specificity was 90 %, higher than what was previously reported. The corresponding average PPV and NPV were 91 and 83 %, respectively, surprisingly different from those in most previous studies [42, 43]. This relatively high PPV and low NPV might be explained by the high prevalence of obstructive CAD in the patients studied.
However, another prospective, multicenter, multi-vendor study with 64-row MDCT CCTA involving 360 symptomatic patients with acute and stable angina and an even higher prevalence of CAD (68 %) reported values of sensitivity, specificity, PPV, and NPV for detecting ≥50 % stenoses, on a patient-based model, of 99, 64, 86, and 97 %, respectively [44]. No patients or segments were excluded because of impaired image quality attributable to either coronary motion or calcifications, which may lead to the low specificity reported in this trial [44].
Except for the CORE 64 trial study, these and other single-center studies consistently reported that CCTA has a particularly high NPV and allows the identification of CAD at an early stage, before emergence of ischemia [27]. From a clinical perspective, a normal CCTA is therefore helpful, as it effectively excludes the presence of obstructive CAD and the need for further testing [4]. Furthermore, CCTA with no detectable plaque defines a low clinical risk with an excellent prognosis with an annual event rate of 0.3 % and makes management decisions straightforward [45].
However, one has to keep in mind that the results are generally limited to relatively large vessel sizes (≥1.5 mm), excluding the results of smaller or uninterpretable vessels (generally distal vessels and side branches). The inclusion of these “difficult” vessels would lower the sensitivity. Furthermore, based on the anatomical-related nature of this imaging technique, CCTA does not provide information on myocardial perfusion or metabolism. This is mainly critical as it was shown that percent narrowing or absolute stenosis lumen area on ICA correlates poorly with the degree of impaired coronary flow reserve [46]. Accordingly, only half of the lesions considered significant on CCTA are linked with abnormal perfusion [15, 47–49]. All of these data clearly indicate that luminal obstruction of the coronaries seen on CCTA does not necessarily indicate the presence of ischemia. Importantly, although a normal CCTA practically excludes relevant hemodynamic CAD, the inverse is frequently not true [27]. Obviously, there seem to be many factors that might influence the relation between anatomical findings and functional, i.e., hemodynamically, consequences, which cannot in total be clarified by anatomical imaging alone [50].
9.4 Integration of Nuclear MPI and CT
Whereas the superiority of applying dual-modality imaging for improved detection and staging of cancer has been proven over years by the results of hybrid positron emission tomography (PET) and CT (PET/CT) imaging, that concept still needs to be proven to be beneficial in the cardiovascular setting as well. This is mainly due for the relatively new hybrid SPECT/CT technique. The aim of hybrid imaging is to provide an accurate spatial alignment between separate anatomical (CT) and functional (MPI) data sets into one fused image. CT scanners are nowadays able to image cardiac and coronary anatomy with high spatial resolution. On the other hand, nuclear imaging in general and MPI in particular can sensitively and reliably identify functional abnormalities. This information together with imaging of the morphology by means of CT might be able to provide information beyond that achievable with either stand-alone or side-by-side interpretation of the respective data sets [4, 27]. It is obvious that in hybrid imaging, both data sets contribute equally to the image information, which helps to reduce the number of equivocal results [51].
Furthermore, it was shown that hybrid MPI and CCTA can accurately allocate the culprit lesion in multivessel CAD, which is particularly important because in more than half of the cases, the proposed “standard” distribution of myocardial perfusion territories does not correspond with the individual coronary anatomy [52, 53]. MPI information helps to overcome the drawback of a reduced sensitivity of CCTA in distal coronary segments and side branches as mentioned above. In contrast, one of the main pitfalls of semiquantitative MPI, the diagnosis of multivessel CAD, can be improved by adding CCTA information [27]. Additionally, assessing regional myocardial perfusion with MPI together with information about the coronary artery tree as provided by CCTA eliminates uncertainties in the relationship of perfusion defects, scar regions, and diseased coronary arteries in watershed regions, mainly in patients with multiple perfusion abnormalities and multivessel CAD [27].
9.5 Integration of CT with MPI for Attenuation Correction
One of the drawbacks of MPI is the nonhomogeneous photon attenuation in the thorax which may reduce both specificity and sensitivity of MPI. Whereas nonuniform regional perfusion defects may be misinterpreted as a perfusion defect and therefore may impact specificity of MPI, sensitivity may be reduced due to improperly scaling of images to regions suppressed by attenuation, potentially masking true perfusion defects [27]. Correcting for these attenuation artifacts in cardiac imaging remains being a challenge because of cardiac and respiratory motion [54, 55]. CT as part of hybrid SPECT/CT imaging technique seems to have the potential to overcome these problems as using the CT component for attenuation correction improved the specificity of SPECT MPI to 80–90 % [56]. However, one needs to take into account, that despite the fact, that SPECT/CT studies have shown that low-dose CT acquisition is feasible for attenuation correction in cardiac imaging, a potential misalignment between emission and transmission data might cause incomplete correction and, consequently, artificial perfusion defects [27]. Therefore, careful quality control to avoid reconstruction artifacts is mandatory. It was recently shown that the frequency of these misalignments is quite high with significant clinical consequences in case they are not corrected [57, 58]. Notably, mainly because of the lower spatial resolution of SPECT, the effect of misalignments is less severe for cardiac SPECT/CT compared to cardiac PET/CT [59]. Usually, the alignment of emission and transmission data is currently performed manually, which may lead to a relevant variability. However, steps towards automated methods for quality control have already been made and might offer a solution to overcome this drawback in the future [27, 60, 61].
9.6 MPI and CAC
Detection of CAC was shown to provide incremental value to MPI [62–64]. Recent reports suggest that CAC may have the potential to improve the diagnostic and prognostic value of MPI. Mainly in case of a normal MPI, CAC was shown to potentially enhance the diagnosis of CAD, which was particularly due in severe multivessel CAD [64, 65]. There is growing evidence that CAC scores are generally predictive of a higher likelihood of ischemia on MPI, and the available data support the concept of a threshold phenomenon governing this relationship [4]. Indeed, it was seen that myocardial ischemia was significantly more frequently diagnosed with increasing CAC scores. This was especially the fact among patients with CAC > 400 [64, 66, 67].
The approach of combining CAC with MPI is promoted by the relative ease to obtain CAC images for which no contrast injection is needed and which is associated with a low overall radiation exposure. Furthermore, an increasing availability of hybrid scanners integrating low- or high-end CT devices with SPECT camera systems is seen and further supportive of implementing combined MPI and CAC imaging into clinical routine [39].
In a study by Schepis et al., a CAC score >709 was found to provide the optimal cutoff to detect patients with obstructive CAD despite normal perfusion in SPECT MPI [65]. In this situation, the normal SPECT imaging most likely reflects balanced ischemia. Using this threshold, the addition of the CAC score to the SPECT MPI data was reported to improve the sensitivity for identifying patients with obstructive CAD over the results of SPECT MPI alone, without a significant decrease in specificity. In contrast, CAC scores >400, especially in symptomatic patients with intermediate likelihood of CAD, may be less effective in excluding CAD. This is mainly the case in young subjects and women [65].
Regarding the added prognostic value of combining CAC with MPI, higher MACE rates are reported for patients with higher CAC scores, even in case of a normal stress MPI [68]. This is mainly due for patients with known CAD or with greater comorbidities [68]. Therefore, CAC as a direct marker of coronary atherosclerosis is helpful in identifying patients requiring a more intensive management of risk factors or follow-up protocol [27]. Furthermore, data suggest that incremental risk stratification can be obtained by incorporating information about the anatomical extent of atherosclerosis as provided by CAC to conventional MPI without CT [4].
9.7 MPI and CCTA
The first clinical results of hybrid MPI and CCTA appear encouraging, as they support that this approach offers superior diagnostic information with regard to identification of the culprit vessels (Fig. 9.1) [4, 47, 69, 70]. This is mainly due to the fact that MPI provides valuable clinical information regarding the pathophysiological significance of coronary stenosis, especially when the sensitivity of CCTA is substantially reduced, which is the case in more distal segments of the coronary arteries and side branches [4, 41]. Previously published studies indicate that this benefit of combining CCTA with MPI becomes evident both in low-risk CAD populations as well as in patients with multivessel CAD [69, 71, 72]. In 2009, van Werkhoven et al. published their results about the incremental prognostic value over SPECT MPI alone in patients with suspected CAD [45]. In 541 patients referred for further cardiac evaluation, both multi-slice CCTA and MPI were performed. Both scans were performed with stand-alone CT and SPECT within a time frame of 3 months and therefore not using a “true” hybrid SPECT/CT approach. MACE were recorded over a median follow-up time of 672 days. The median hard event rate in patients with none or mild CAD by CCTA was 1.8 % versus 4.8 % in patients with significant CAD by CCTA. Accordingly, a normal MPI and abnormal MPI were associated with an annualized hard event rate of 1.1 and 3.8 %, respectively. After adjustment for clinical risk factors, obstructive plaque detected by CCTA and an abnormal MPI was independently predictive for late events. This prediction significantly improved when combining the two modalities compared with either modality alone. Concordantly normal CCTA and MPI were associated with an annual event rate of 1 %, whereas this rate increased to 9 % in case of concordantly abnormal CCTA and MPI results. Importantly, the presence of noncalcified plaques provided incremental prognostic information over baseline clinical variables, MPI, and significant CAD on CCTA [45].
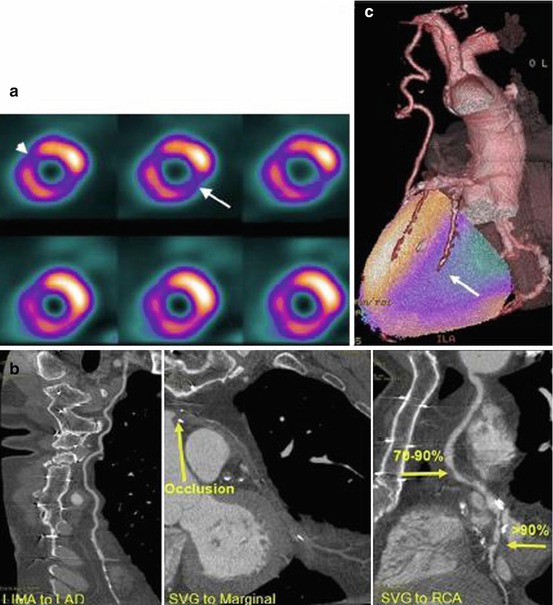
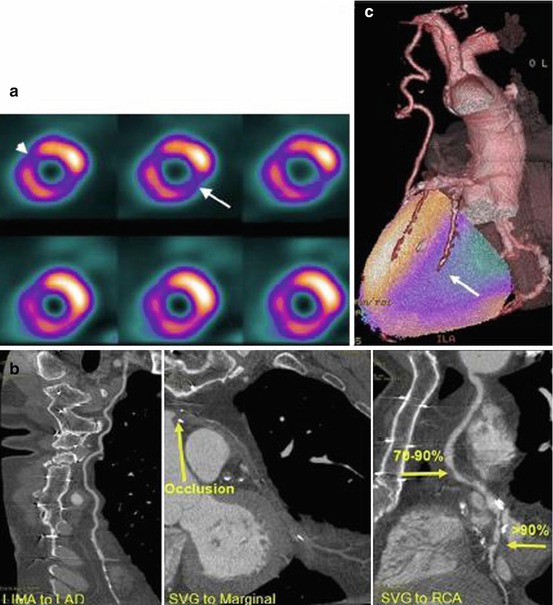
Fig. 9.1
(a) A 61-year-old man with NSTE-MI and a history of stent insertion and coronary artery bypass grafting. SPECT short-axis slices (upper row stress, lower row rest) demonstrate a reversible perfusion defect at the inferolateral wall indicating ischemia (arrow) and an anteroseptal fixed defect consistent with scar tissue (arrowhead). (b) CCTA demonstrates the presence of three-vessel coronary artery disease with an occluded SVG to the marginal artery (middle image, arrow) and two areas of severe stenosis in the SVG to the RCA (right image, arrows). The LIMA to LAD is normal (left image) (LAD left anterior descending coronary artery, LIMA left internal mammary artery, RCA right coronary artery, SVG saphenous vein graft). (c) SPECT/CCTA fused data relate the inferolateral myocardial ischemia to the territory of the RCA (arrow) (With permission from Rispler et al. [73])
In a study by Rispler et al., published in 2007, 56 patients with angina pectoris underwent single-session SPECT MPI and CCTA with a hybrid SPECT/16-row CT device and coronary angiography within 4 weeks [47]. The ability of fused SPECT/CCTA images to diagnose physiologically significant lesions showing >50 % stenosis and reversible perfusion defects in the same territory was determined and compared with CCTA stand-alone. They found a total of 224 coronary segments in the 56 patients included; 12 patients and 54 segments (23 %) were excluded from further analysis of CCTA. Therefore, a total of 170 coronary segments were evaluated. The sensitivity, specificity, PPV, and NPV of CCTA were 96, 63, 31, and 99 %, respectively, as compared with 96, 95, 77, and 99 %, respectively, for combined SPECT/CCTA. Based on these results, it becomes quite obvious that hybrid SPECT/CCTA imaging mainly results in improved specificity and PPV to detect hemodynamically significant coronary lesions in patients with chest pain [47].
Several other studies underscored the incremental diagnostic accuracy or co-registration and fusion of stand-alone acquired MPI and CCTA over side-by-side interpretation (Table 9.2) [4, 69, 74, 75]. To further strengthen these findings, Rispler et al. found added diagnostic information provided by fused analysis not obtained on side-by-side analysis in almost one-third of patients [47].
Table 9.2
Diagnostic value of SPECT/CT or PET/CT software image fusion compared by side-by-side analysis
Technology | N | Benefit by hybrid imaging | Reference |
|---|---|---|---|
SPECT/64-row MDCT and 3-D image fusion | 38 patients with ≥1 SPECT defects | Among equivocal lesions, haemodynamic significance is confirmed in 35 % and excluded in 25 % | [69] |
16- and 64-row MDCT and MPI (SPECT or 82Rb PET) | 50 patients suspected of CAD | Modification of the initial interpretation in 28 % of the cases | [74] |
Trend to increase in 17 % the sensitivity in patients with multivessel disease | |||
Automated SPECT/64-row MDCT registration software | 35 patients suspected of CAD | Improved diagnostic performance in the RCA and LCx, not in LAD | [75] |
In another, well-designed and recently published study by Schaap et al., the diagnostic performance of hybrid SPECT/CCTA versus stand-alone SPECT and CCTA for the diagnosis of significant CAD was evaluated [76]. Ninety-eight patients with stable angina complaints and a median pretest likelihood of 87 % were prospectively included in their study. Hybrid SPECT/CCTA was performed prior to conventional coronary angiography. Hybrid analysis was performed by combined interpretation of SPECT and CCTA images. The diagnostic performance was calculated for hybrid SPECT/CCTA and stand-alone SPECT and CCTA on per-patient level. Fractional flow reserve measurements <0.80 served as a reference for significant CAD and was seen in 57.9 % of the patients included. Non-conclusive SPECT or CCTA results were found in 32.7 % of the patients. Stand-alone SPECT and CCTA had a sensitivity of 93 %, specificity 79 %, PPV 85 %, and NPV 89 % and a sensitivity of 98 %, specificity 62 %, PPV 77 %, and NPV 96 %, respectively. Hybrid analysis of SPECT and CCTA led to an improved overall performance with a sensitivity, specificity, PPV, and NPV for the presence of significant CAD of 96, 95, 96, and 95 %, respectively [76]. Based on the results of the study, two highly interesting conclusions can be drawn. First of all, in >40 % of the patients with a high pretest likelihood, no significant CAD was demonstrated. This clearly emphasizes the value of accurate pretreatment cardiovascular imaging. Secondly, by combining SPECT and CCTA, significant CAD can be accurately diagnosed and excluded, surpassing the diagnostic performance of stand-alone myocardial SPECT and CCTA [76].
Whereas CCTA alone tends to overestimate coronary stenosis, the combination with MPI, and therefore with the information about the hemodynamic relevance of the observed stenosis, allows the identification of many false-positive CCTA findings [27]. Mainly in case of motion artifacts or severe coronary calcifications, the specificity and PPV of stand-alone CCTA becomes suboptimal [27]. In this context, it needs to be pointed out that non-evaluable, severely calcified vessels especially benefit from further testing due to the relatively high likelihood of obstructive disease, whereas non-evaluable vessels with motion artifacts do not usually have hemodynamic relevance. The latter is particularly the case in the right coronary artery (RCA) territory [27, 77]. However, hybrid imaging with CCTA and SPECT MPI is of particular value not only in the RCA but also in lesions of distal segments, diagonal branches, and the left circumflex artery (LCX) [69, 74]. On the other hand, CCTA improves the detection of multivessel CAD, which is one of the main pitfalls of MPI as already mentioned above, and increases the diagnostic confidence for categorizing intermediate lesions and equivocal perfusion defects [4, 47].
9.8 Radiation Exposure
Both SPECT and CT are diagnostic modalities that use ionizing radiation to generate images for the functional and morphological evaluation of the heart.
The radiation exposure related to MPI is lower for the nowadays most frequently used 99mTc (99mtechnetium)-labelled agents (like 99mTc-sestamibi, 99mTc-tetrofosmin) compared to the use of 201thallium (201Tl). Depending on the applied protocol (1- or 2-day protocol), the injected dose, and the used camera system, the radiation exposure of 99mTc-sestamibi or 99mTc-tetrofosmin may differ with an increasing dose by applying a 1-day protocol. The reported effective doses for 99mTc-sestamibi (rest) are 0.009 mSv/MBq (stress: 0.0079 mSv/MBq) and for 99mTc-tetrofosmin (rest) 0.0069 mSv/MBq (stress: 0.0069 mSv/MBq), respectively. For 201Tl, one has to consider an effective dose of 0.14 mSv/MBq, which will even increase with a reinjection of 201Tl [78–81]. However, nowadays, SPECT-related radiation exposure can be markedly reduced by the use of new iterative reconstruction methods in combination with dedicated detectors and collimators optimized specifically for MPI [82, 83]. Further emphasizing the necessity of reducing the radiation exposure to the patients in MPI, a statement document was published by Cerqueira et al. in 2010 regarding the best practice methods to further minimize the radiation exposure of MPI by obtaining the highest-quality diagnostic images [84].
The effective patient radiation dose from cardiac CT varies widely depending on the protocol, instrumentation, and patient size [27]. For a CAC scan, which can also be used to perform MPI attenuation correction, the radiation exposure of approximately 1 mSv is rather low [85]. However, the dose tends to be higher with lower slice thickness, as in this case, the radiation dosage needs to be increased to obtain the same signal to noise ratio [86]. In a 2009 published cross-sectional, international, multicenter study of 1,965 CCTA scans performed at 50 study sites, the estimated mean radiation dose was 12 mSv (interquartile range: 8–18 mSv) [87]. A reduction of the radiation exposure can be achieved by implementation of modern cardiac CT acquisition protocols. Prospective (step-and-shoot) ECG triggering, ECG-controlled current modulation (reduction of the tube current by 80 % during systole), and body mass-adapted tube voltage (reduction of the tube voltage to 100 kV in patients <90 kg of weight) allow reduction of the radiation dose from CCTA by 60–80 % [71, 88–90]. Along with this, application of the most recent high-pitch scanning protocols using dual-source CT scanners has even further lowered doses into the sub-millisievert range [38, 39].
9.9 Clinical Applications
It is well accepted that the clinical use of imaging should depend on the pretest likelihood of CAD [27]. In the 2011 joint position statement by the European Association of Nuclear Medicine (EANM), the European Society of Cardiac Radiology (ESCR), and the European Council of Nuclear Cardiology (ECNC),a proposed clinical algorithm for the use of imaging techniques, including hybrid imaging, in patients with chronic chest pain was published (Fig. 9.2). Furthermore, it was stated that for symptomatic patients without known CAD and low to moderate pretest (i.e., < 50 %) likelihood of disease, which is typically seen in young and middle-aged patients, CCTA would probably be essential to (virtually) exclude CAD [27]. Whereas in case of a normal result, further diagnostic tests are avoided, abnormal or equivocal findings need to be confirmed or rejected by MPI or ICA [27]. Especially in these patients, hybrid imaging would lead to a more rapid diagnosis. Today, when initial tests yield equivocal results and further assessment to exclude CAD with final certainty is needed, many of these patients are referred for ICA. Hybrid cardiac imaging offers a substantially improved diagnostic confidence, and the more frequent use of these techniques would therefore result in a reduction of the number of patients, which are currently unnecessarily exposed to ICA [27].
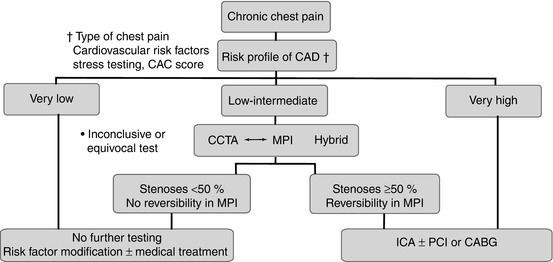
Fig. 9.2
Proposed clinical algorithm for the use of imaging techniques in patients with chronic chest pain. CABG coronary artery bypass grafting, CAD coronary artery disease, CCTA cardiac computed tomographic angiography, ICA invasive coronary angiography, MPI myocardial perfusion imaging (SPECT or PET), PCI percutaneous coronary intervention (With permission from Flotats et al. [27])
In patients with higher pretest likelihood of disease (i.e. >50 % likelihood), which are characteristically those with known CAD or older age, MPI might be a better first-line test compared to CCTA [27]. This group of patients is more likely to have extensive CAC and also includes patients with known or suspected microvascular endothelial dysfunction, e.g. diabetics [27, 77, 91]. In case of equivocal MPI findings, suggestive of artifacts, microvascular or multivessel disease, CCTA can be added. In these patients, the hybrid imaging approach would lead to an improved diagnostic accuracy and would also allow for a complete evaluation of the hemodynamic relevance of coronary stenosis and the assessment of the viability in myocardial territories supplied by occluded arteries [27]. The accurate co-registration of CCTA and MPI data would allow to gain information about coronary stenoses and perfusion defects and therefore would also improve the evaluation of hemodynamic properties of even fairly small coronary branches [27]. By confirming the hemodynamic relevance of given lesions, hybrid cardiac imaging might help to avoid potentially harmful revascularization attempts and also provides a platform for multidisciplinary coronary teams including an interventional cardiologist and a cardiac surgeon to discuss the most appropriate treatment strategy (medical conservative vs. percutaneous vs. surgical revascularization) [39]. In this context, Schaap et al. prospectively evaluated to what extent treatment decisions for patients with stable angina pectoris can be made based on hybrid MPI SPECT and CCTA as the question remains whether these imaging results lead to similar treatment decisions as compared to stand-alone SPECT and ICA [92




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree