Fig. 8.1
Osteomyelitis after polytrauma
8.5 SPECT/CT in Spine and Hip Conditions
8.5.1 Degenerative Changes of the Spine
Osteoarthrosis of the spine is one of the most frequent articular afflictions. It is caused by a variety of different processes and predominantly affects elderly people. In the vertebral column, the major types of degenerative disease include cartilaginous, uncovertebral, synovial, and fibrous joints. Each of these is characterized by morphological abnormalities that allow for their differentiation from other types of disease such as malignancies. Disk space narrowing, vacuum phenomena, well-defined sclerotic vertebral margins, osteophytosis, eburnation, and perivertebral calcifications all represent radiographic signs of spine degeneration.
Although anatomical imaging may readily define sites of degenerative and facet joint disease, 99mTc-MDP bone scintigraphy may localize metabolically active sites of disease [49, 50]. Increased tracer uptake is typical for intervertebral osteochondrosis and osteoarthritis but is found less often in spondylosis deformans. Occasionally, extreme spinal osteophytosis may be seen on radiographs while the bone scan is normal.
It is well known that abnormal radionuclide uptake in the spine is most often related to degenerative disease; however, it is difficult to differentiate from other skeletal abnormalities. SPECT/CT may be useful to confirm that a focal bone reaction is related to degenerative process and to rule out other causes of an increased uptake (Fig. 8.2), most notably bone metastases [21] and even bone infiltration from soft tissue tumors (Fig. 8.3). Furthermore, it is possible with SPECT/CT to differentiate costovertebral joint osteoarthritis from facet joint involvement and guide therapeutic intervention [50–52].
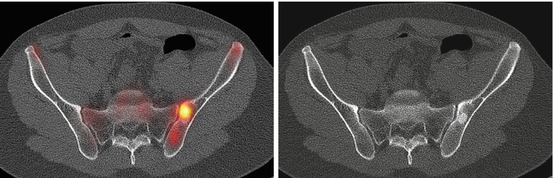
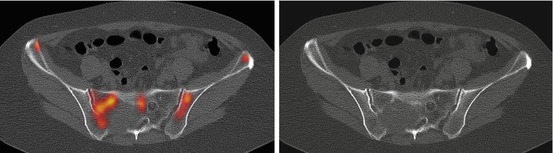
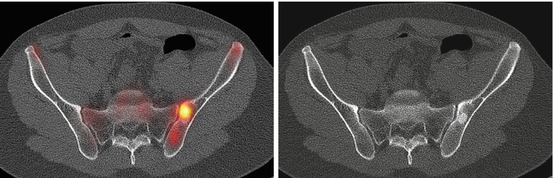
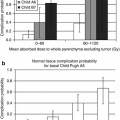
Fig. 8.2
Focally increased tracer uptake in the osteoblastic lesion of the left os ilium in a patient with chronic pain referred with suspected sacroiliitis
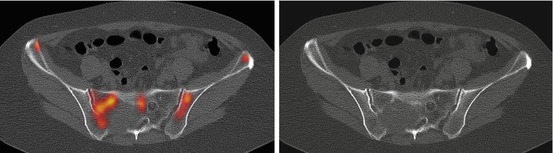
Fig. 8.3
Infiltration of right of sacral bone by soft tissue tumor
8.5.2 Compression Fractures of the Spine
Osteoporosis is the most common cause of compression fractures in the spine. The age and accurate localization of the fracture are critical for the therapy planning including vertebroplasty and kyphoplasty [53]. Scintigraphy can confirm and establish the age of vertebral fracture [54, 55]. One of the major utilities of bone scintigraphy is in deciding if a fracture is of long-standing and has no potential for healing, or it is metabolically active and has capability for healing [6]. A study that examined surgical outcomes for spondylolysis based on preoperative SPECT clearly showed that patients with positive studies had a better outcome than those with negative SPECT [56].
Scintigraphic appearances are loss of vertebral height and contour with intense linear uptake. However, the greatest challenge is the presence of other abnormalities near to the fracture accumulating the tracer. MRI is often used for anatomic localization, but is not always discriminative. In such cases, SPECT/CT may be of a great benefit especially for a better therapy planning. Applying SPECT/CT, compression fractures can also be distinguished from severe degenerative disease, both of which can cause intense activity across the spine on either planar or SPECT imaging. In patients with osteoporotic vertebral collapse and chronic back pain [57, 58], 99mTc-MDP bone SPECT/CT may often detect abnormal facet joint activity adjacent to a collapsed vertebra and can identify the patients who might benefit from specific treatment to this joint [58].
8.5.3 Spinal Fusion
Patients with intractable low back pain or those with significant neurologic deficit may undergo spinal fusion to stabilize the spine, restricting motion to prevent symptoms. However, a significant number of patients will have either residual or recurrent pain and further treatment depends on distinguishing among several possible causes [59]. Localizing activity in patients who have had spinal fusion can provide tremendous insight into the causes of therapeutic failures. There may be failure of the surgical hardware, which usually is associated with fracture of the bone graft and formation of a pseudarthrosis. In this setting, CT scanning often shows a lucent area surrounding the pedicle screws, and a bone scan will be positive in a pattern seen in other forms of hardware loosening. There may also be facet joint arthritis or disk space degenerative disease at adjacent levels, which is due to the transmission of forces, either above or below the area of rigidity created by the surgery (Fig. 8.4). Finally, there may be unrelated findings, such as sacroiliitis, or pathology associated with bone graft donor sites in the pelvis. CT imaging makes it possible to view these areas with a minimum of beam hardening artifact and, therefore, makes it possible for SPECT/CT to help find the cause of residual or recurrent symptoms.
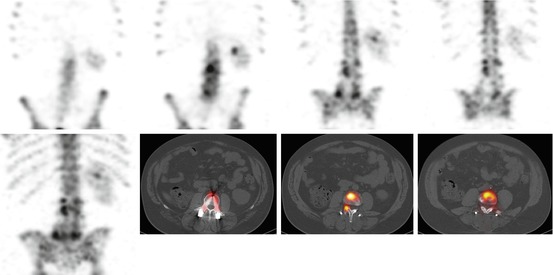
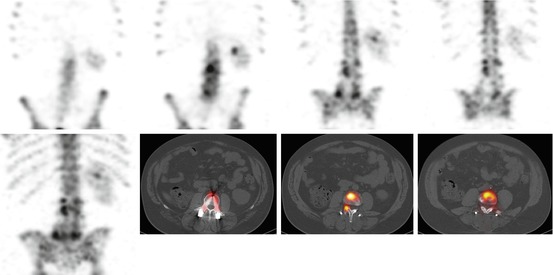
Fig. 8.4
Degenerative changes below the screws in a patient with suspected hardware loosening
8.5.4 Back Pain in Young Adults
Many injuries in this age group are the result of muscle strain, and physical therapy is often prescribed. In patients with fractures of the pars interarticularis, however, physical therapy should be avoided, and back braces are often used to limit motion during the healing phase. Stress fractures of the pars interarticularis have an incidence of 6 % in the general population and account for 15 % of pediatric stress fractures. These fractures may not be suspected clinically because the patients often present with relatively sudden pain but no clear traumatic injury. Scintigraphic imaging is important because 15 % of evolving fractures may not be evident on CT scanning [60]. Although bone scan is sensitive to the presence of fractures of the pars interarticularis, planar imaging may fail to demonstrate a large number of these lesions and, therefore, SPECT imaging is required [61–64]. SPECT/CT may distinct the fractures of the pars and other focal areas of increased activity including facet joint arthritis [65].
The use of SPECT/CT may also detect causes of unexplained hip pain, such as femoral acetabular impingement syndrome [66, 67]. This is characterized by groin pain in young adults and may lead to early osteoarthritis of the hip [68, 69]. The identification of femoral acetabular impingement as a cause of osteoarthritis allows appropriate therapy early and thus delays or prevents end-stage arthritis.
8.6 SPECT/CT in Extremities
The bony extremities, particularly the wrist, foot, and ankle, consist of a complex group of bony articulations, making accurate localization of tracer uptake on planar imaging challenging. Several conventional radiological and radionuclide techniques, such as ultrasonography, 99mTc-MDP bone scan, CT, and MRI, are used in the evaluation of extremities. All of which have several advantages and limitations with varied sensitivity and specificity. SPECT/CT provides, apart from the general conditions such as degenerative disease, more specific diagnoses, such as impingement syndromes, osteochondral defects, and trauma. Gnanasegaran and O’Doherty [70] reported additional diagnostic information of SPECT/CT of the ankles/feet in 81 % (25/31) of an unselected group of patients which resulted in a potential change in management of 62 % of patients.
8.7 Upper Extremities
Although there is only very limited experience concerning the use of SPECT/CT in the evaluation of upper extremities joints, the reported results are encouraging. In a study on 51 patients with persisting wrist pain, SPECT/CT detected considerably more lesions (20 %) than planar bone scan and had significant impact on the therapy in 37 % of patients [71]. In a prospective study on patients with clinical signs of fracture but normal radiographs, SPECT/CT detected more occult carpal fractures than MRI [72]. SPECT/CT has also proved more specific in the evaluation of causative pathologies in patients with nonspecific pain of the hand and wrist, whereas MRI was more sensitive in this setting [73]. In another study, SPECT/CT was valuable in diagnosing scaphoid lesions compared to plain radiography and planar scintigraphy [74]. SPECT/CT could also facilitate the establishment of diagnosis in patients with pain after shoulder arthroplasty [75].
8.8 Lower Extremities
8.8.1 Painful Knee
Knee SPECT has been reported to be useful in the evaluation of meniscal tears and cruciate and collateral ligament injury [76–79]. However, it is difficult to characterize the abnormalities or localize the site without anatomical or structural correlation, and SPECT/CT may be useful in localizing and characterizing the lesions, such as osteoid osteoma, osteochondral defects, bone remodeling at the site of an anterior cruciate ligament repair, patella maltracking/subluxation, as well as loosening of a total knee replacement. Total knee arthroplasty is the treatment of choice for patients with disabling primary osteoarthritis of the knee joint which leads to satisfactory long-term results. However, failure does occur in a considerable number of patients resulting in persistent or recurrent knee pain [80, 81]. The most common causes are considered to be infection, loosening, instability, prosthetic malposition, arthrofibrosis, and patellofemoral disorders [81, 82]. Clinically it can be difficult to differentiate between causes which necessitate surgical treatment from those which could be treated nonsurgically [82]. Hence, identifying the underlying cause of the pain is of paramount importance for guidance of optimal patient management.
Radiographs are considered to be the primary standard imaging technique in patients with knee pain after arthroplasty [80, 82]. However, these are only helpful in detecting gross prosthetic malposition, radiolucencies, and fractures. Plain radiographs are less sensitive in detecting more common but subtle abnormalities such as early loosening or minor implant malposition [80]. Radiographs are also subject to measurement inaccuracy due to variability in reproducible patient positioning [83, 84]. CT has its value in identifying malposition and may reveal the extent and size of periprosthetic lucencies not apparent on plain radiographs [85, 86]. Although planar bone scintigraphy and SPECT give important information on the osseous metabolism and joint homeostasis, their clinical value is limited due to the poor accuracy in localizing the increased tracer uptake [87–89]. Hybrid SPECT/CT may be useful in patients with postsurgical knee pain particularly when other radiographic imaging provides insufficient or ambiguous information [83, 84]. SPECT/CT imaging significantly changes the diagnosis and treatment proposed, independently of previous intention to revise or treat the patient nonsurgically (Fig. 8.5). With SPECT/CT changes within the patellofemoral joint, which may be due to progression of patellofemoral osteoarthritis, can be distinguished from other knee compartments, which may be due to mechanical loosening of the tibial or femoral prosthetic components (Fig. 8.6).
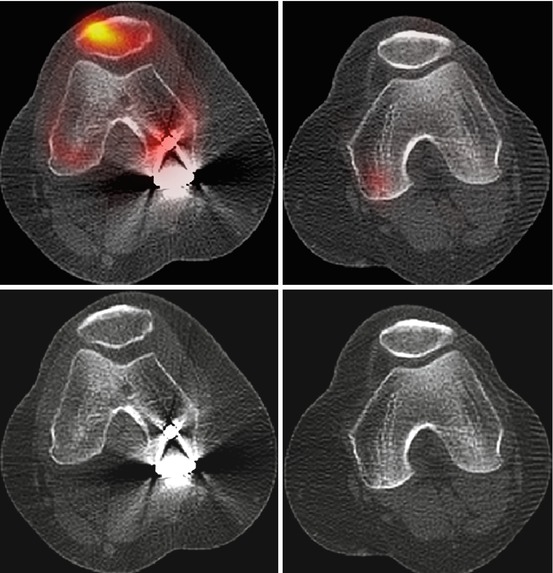
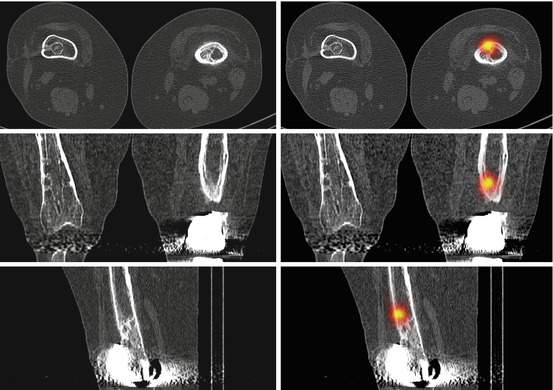
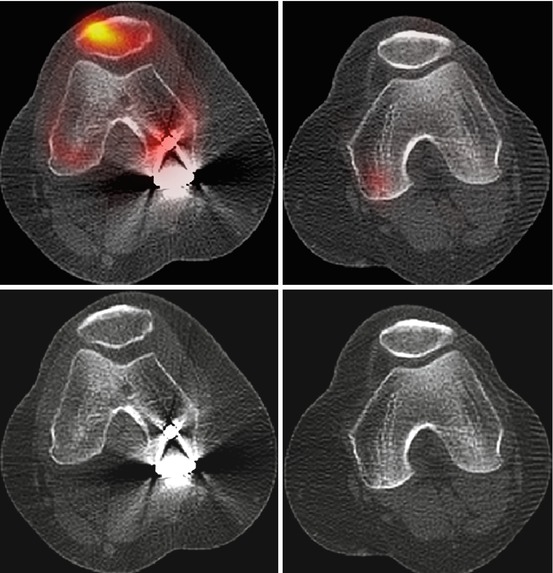
Fig. 8.5
Femoropatellar arthrosis in a patient with suspected loosening of knee prosthesis
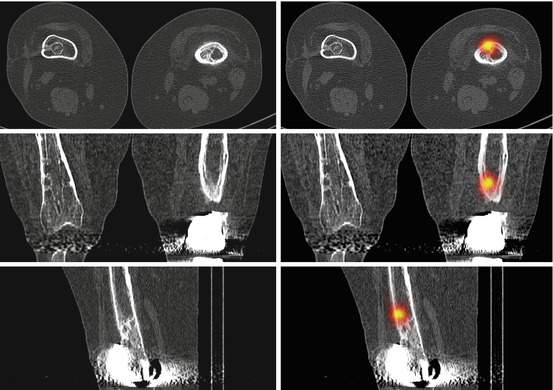
Fig. 8.6
Osteoid osteoma in patient with knee pain after knee replacement
Another problem in the interpretation of SPECT tracer uptake is the presence of increased tracer uptake in almost 20 % of patients up to 1 year after total knee replacement even in asymptomatic knees with perfect prosthetic alignment [88, 90]. A diffusely intense uptake around the prosthesis is suspicious for loosening, infection, mechanical malalignment, or progression of OA [90], while the absence of tracer uptake makes these causes highly unlikely. Patients with femoral mechanical loosening may present with increased tracer activity around the femoral tray which extended more frequently to the bone-prosthesis interface [91, 92]. In contrary changes below the tibial tray are considered to be less specific [91]. Malposition of prosthetic components, including the malrotation of the femoral or tibial component, is one of the most important factors leading to failure of total knee arthroplasty [93, 94]. SPECT/CT enables the correlation of component position with tracer uptake in each anatomical area for patients (Fig. 8.7).
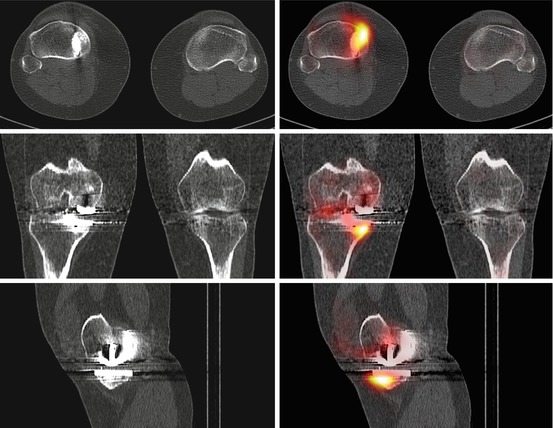
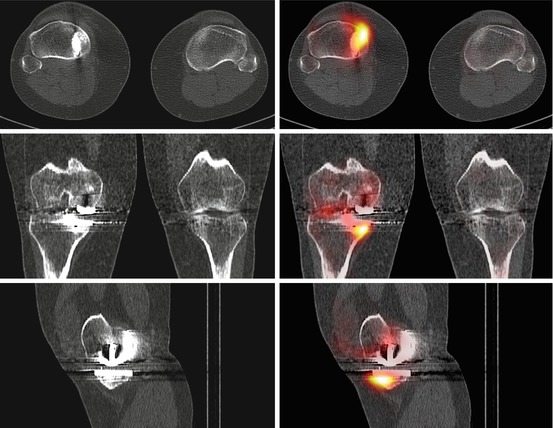
Fig. 8.7
Mechanical loosening of the tibial components 12 months after knee replacement
8.8.2 Foot and Ankle
Disorders of the ankle and foot are common, and the complex anatomy and function of the foot may hinder the diagnosis. It is only with SPECT/CT that details of complicated combinations of old and new injuries can be sorted out (Fig. 8.8).
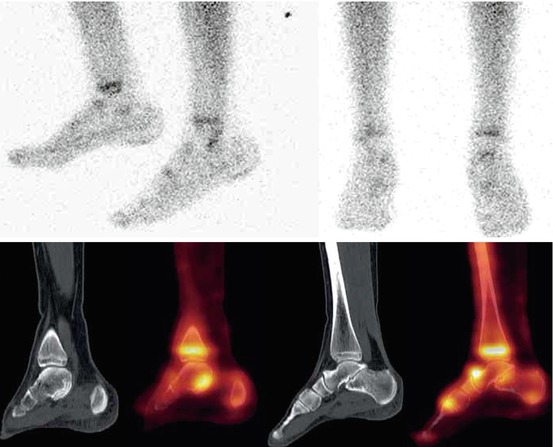
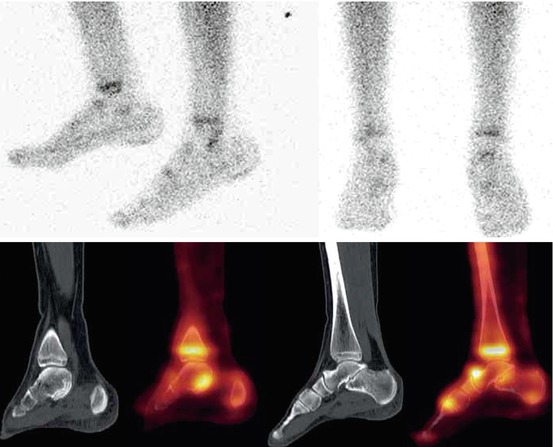
Fig. 8.8
Talocalcaneal coalition in a young patient with chronic heel pain
8.8.2.1 Chronic Ankle and Heel Pain
Obscure pain around the foot and ankle can be notoriously difficult to localize. Posterolateral ankle pain from chronic overuse may be due to the posterior impingement syndrome, impingement of the os trigonum, or peroneal tendonitis [95]. The scintigraphic appearance is of intense uptake in the posterior talus [96]. Anterior ankle pain following overuse is, on the other hand, due to the anterior impingement syndrome, and an increased tracer uptake is seen in the anterior aspect of the ankle [72].
Plantar fasciitis is one of the most common causes of heel pain [97]. Other causes of heel pain that may be elucidated by scintigraphy include Achilles tendonitis and bursitis, retrocalcaneal bursitis apophysitis of the calcaneum, and calcaneal stress fracture. Knowledge of anatomy is crucial in determining an accurate diagnosis because differences in the pattern of uptake can be subtle.
8.8.2.2 Osteochondral Defect (OCD)
OCD is a repetitive stress injury seen in young athletes [98]. Overuse of a joint leads to disruption in the blood supply to the adjacent bone. Bone and cartilage fragments often separate because of devitalization of the subarticular region, and these fragments may cause severe pain in the joint. The cystic degeneration that occurs in these patients is confined to the talar dome. Bilateral lesions may occur in approximately 10 % of cases, although medial lesions are more common. Surgery is often recommended in patient with persistent pain to smooth the articular surface and to remove fragments of bone and cartilage that may be interfering with motion. However, an osteochondral lesion of the talar dome is often subtle and missed on plain films. Bone scan is a sensitive screening test used in the diagnosis of talar OCD [99–102]. Increased blood flow and blood pool at the talar region associated with focally increased activity at the talar dome is suggestive of an osteochondral lesion. Abnormal focal activity at the talar dome was found to have 94 % sensitivity and 76 % specificity for osteochondral lesions [101].
8.8.2.3 Tarsal Coalition
Tarsal coalition is the congenital fusion of two of the tarsal bones with either a bony or fibrous bridge [103]. Three types of coalition exist: fibrous (syndesmosis), cartilaginous (synchondrosis), and osseous (synostosis) fusion. Calcaneonavicular and talocalcaneal coalition are the most common sites. The resulting stress on the hindfoot causes pain, which usually begins in the early adulthood. Surgery is required to separate the bones in those patients who do not respond to conservative treatment. Oblique anteroposterior radiography of the foot may at times identify calcaneonavicular coalition, whereas talocalcaneal coalition is often overlooked on plain radiographs because of overlapping structures. Diagnosis of talocalcaneal coalition on X-ray may be deduced by the presence secondary signs such as talar breaking [103], flattening and broadening of the lateral talar process, positive C sign [104–106], absent middle facet sign [107], and narrowing of the posterior talocalcaneal joint. Although CT and MRI are not the imaging studies of choice for tarsal coalition, CT of the subtalar joint is often diagnostic [108]. SPECT/CT may be an improved alternative to CT alone with addition of supplementary functional information from the bone scan (Fig. 8.9). The area of uptake on the SPECT study may also help guide intra-articular injections.
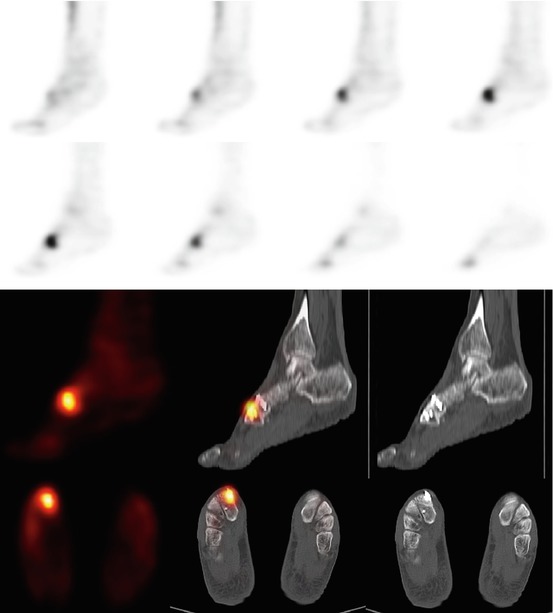
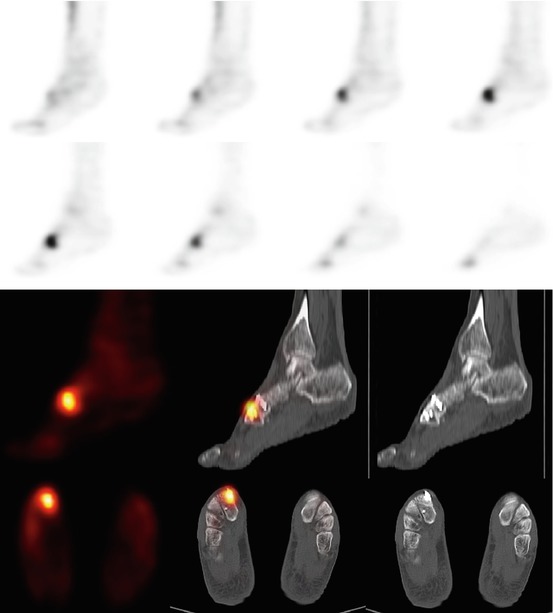
Fig. 8.9
Delayed union 10 months after cuneonavicular joint fusion
8.8.2.4 Osteoid Osteoma
Osteoid osteomas are benign tumors of bone seen often in teenagers [109]. They classically produce nocturnal pain that responds dramatically to salicylates. The pain responds to surgical removal of the nidus. A focus of intense activity is almost always seen on bone scan, and a lucent nidus can usually be identified on CT.
8.8.2.5 Planning of Joint Fusion
Selective fusion of painful osteoarthritic joints in the foot and ankle is crucial for the effective treatment of pain with minimal loss of function. Exact localization of active degenerative disease may require extensive assessment using several modalities of radiological imaging. Robinson et al. proposed the use of “coregistration imaging,” which superimposed the biological information derived from bone scan images on the morphological assessment of plain radiographs [110]. The morphological changes in radiological imaging correlate poorly with symptoms and with the progression of degenerative joint disease [111, 112]. However, scintigraphic activity correlates with the symptoms of degenerative joint disease and serves as a strong negative predictive value for the progression of joint degeneration [113]. Hence, in the evaluation of degenerative joint disease in the foot and ankle with pain of uncertain origin, evaluation by both a CT and a bone scan is usually required to determine the localization of active joint degeneration. The use of SPECT/CT images significantly increases the intraobserver and interobserver agreement. Its importance may be most pronounced in small complicated anatomical especially in the regions of naviculocuneiform and tarsometatarsal joints.
8.8.2.6 Postoperative Evaluation of Joint Fusion
Joint arthrodesis is used for the treatment of painful malalignment or arthritis of the hindfoot [114, 115]. Successful osseous union after joint arthrodesis is usually expected to occur within 6 months of the procedure and is confirmed if no joint motion is detected on clinical examination and there is evidence of trabeculation across the arthrodesis site as observed on plain film radiographs [116, 117]. Delayed union is defined as a successful fusion 6–9 months after surgery. In patients who continue to experience pain after arthrodesis, nonunion is suspected. Other complications that result in persistent pain after arthrodesis include overload of the adjacent joints, with development of arthritis in about 30 % in the medium term [118]. Postoperative assessment of the success of fusion has been routinely evaluated using X-ray and CT techniques [119]. Computed tomography scanning has gained use in identifying nonunion sites associated with pain but may provide limited information if metal implants are retained because of scatter effects. Retained metal implants may be removed before CT scanning to improve diagnostic accuracy that may be beneficial anyway as the hardware can be the source of discomfort (Fig. 8.10). SPECT/CT may provide a valuable technique for the evaluation of continuing pain in the context of arthrodesis with in situ hardware. This may improve the accuracy of identifying nonunion (Fig. 8.11) or malunion or subjacent arthritis (Figs. 8.12 and 8.13) as the cause for continuing pain.
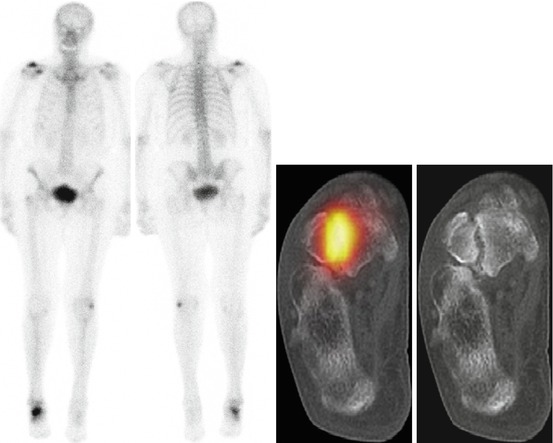
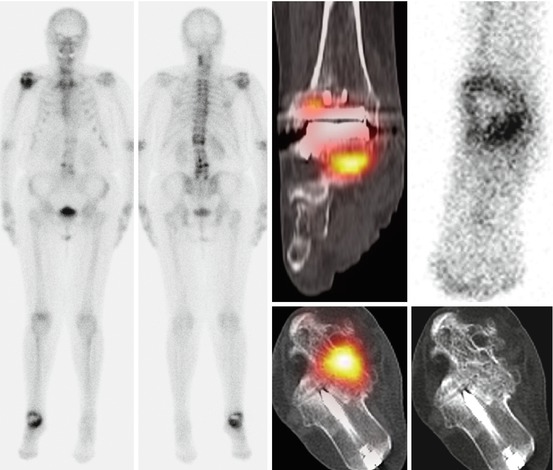
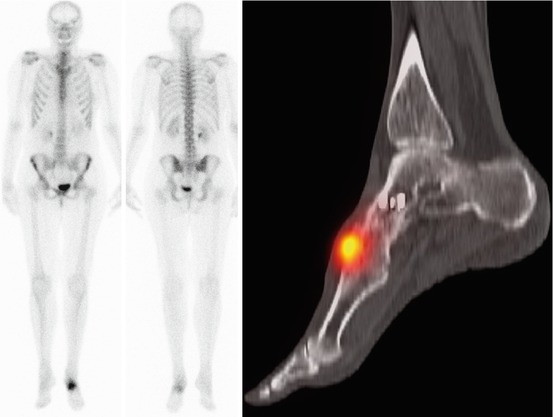
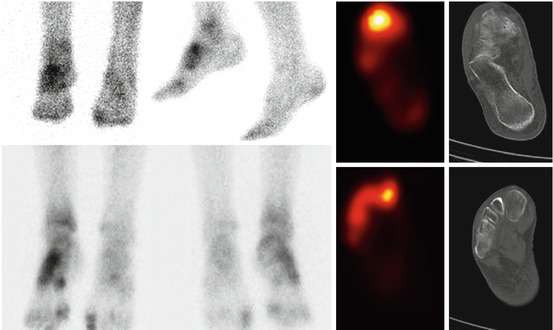
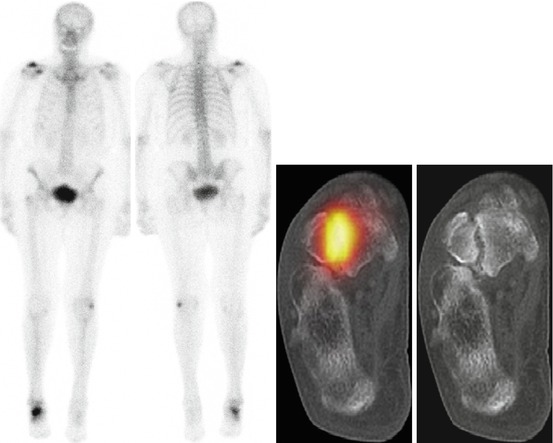
Fig. 8.10
Talar fracture in a patient with chronic ankle pain and history of trauma 5 months earlier
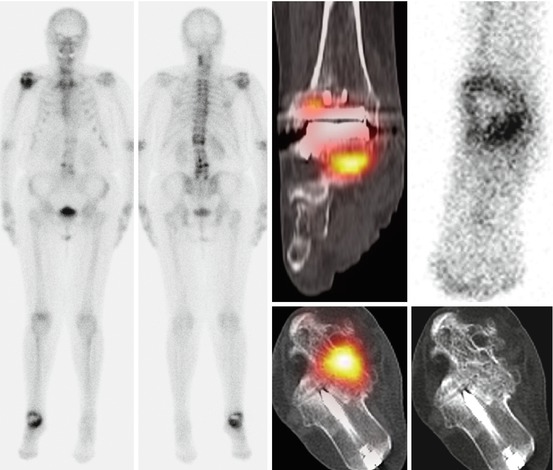
Fig. 8.11
Subjacent arthritis of talonavicular joint in a patient with chronic ankle pain who underwent the fusion 12 months earlier
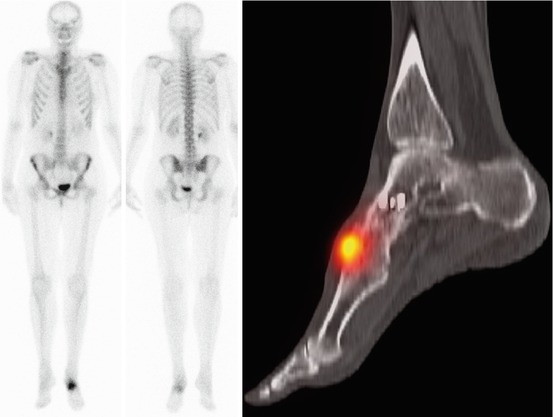
Fig. 8.12
Subjacent arthritis of cuneonavicular joint 18 months after talonavicular joint fusion
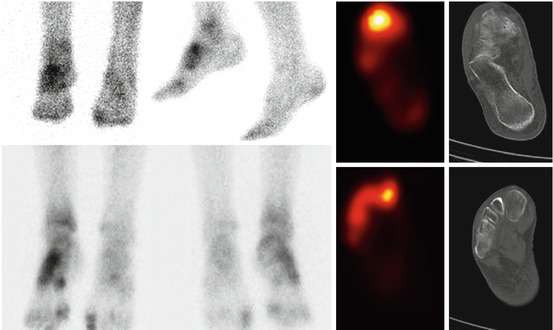
Fig. 8.13
Osteomyelitis of the hindfoot
8.8.2.7 Assessment of Postarthrodesis Infection
Despite strict aseptic measures and prophylactic antibiotic usage, superficial wound infections have been reported in as many as 3 % of patients undergoing midfoot and rearfoot fusions [120]. Elderly patients have been seen to experience a significantly higher infection rate with rearfoot fusions reported at 11 % [121, 122], but advanced age is not necessarily a contraindication for performing a midfoot or rearfoot fusion. Deep infections place the extremity at risk, and in such instances, appropriate and aggressive surgical debridement of all infected and devitalized bone, as well as implants should be undertaken. SPECT/CT bone scan may provide an excellent tool in assessing the presence and extent of infection, with the SPECT study delineating the extent of bony involvement and the CT study demonstrating the associated soft tissue changes (Fig. 8.14). This would be preferred to MRI given the problems posed by postsurgical scarring and micrometallic artifacts and also for diabetic patients in whom there is the additional risk of nephrogenic fibrosis associated with gadolinium contrast. A SPECT/CT white cell study would be useful in confirming bone and soft tissue infection and also in monitoring response to treatment.
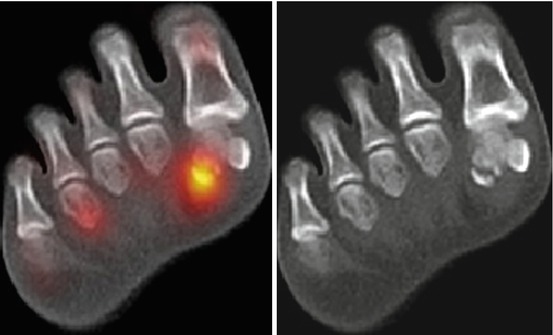
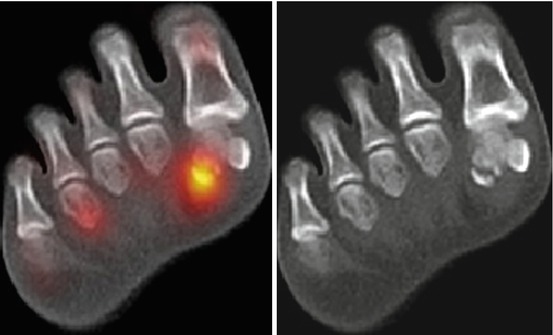
Fig. 8.14
Fracture of sesamoid bone in a patient with chronic pain in forefoot
8.8.2.8 Plantar Fasciitis and Achilles Tendonitis
Plantar fasciitis is a common enthesopathy causing heel pain. It may occur at any age but is common in patients aged 40–60 years [123]. Typically, plain radiography is not helpful, but is always done to rule out other conditions. Radiography may reveal a plantar calcaneal spur, but as this type of spur is commonly observed in asymptomatic adults, it is not specific. Bone scanning and MRI have been shown to be helpful in determining a diagnosis [124]. SPECT/CT can provide information about local alterations of metabolic activity in addition to providing excellent anatomical resolution of the plantar fascia.
Achilles tendonitis is essentially an overuse, degenerative condition [125]. Although MRI and ultrasonography remain the main modalities for the evaluation of the Achilles tendon, SPECT/CT may provide useful coincidental imaging information for the clinician. The SPECT study would demonstrate the metabolic abnormalities associated with the calcaneus, while CT would be useful in demonstrating the associated soft tissue abnormalities.
8.8.2.9 Painful Accessory Bones
Accessory bones have been described with chronic foot pain [126, 127]. The accessory tarsal navicular is situated adjacent to the medial and posterior margins of the tarsal navicular and has a prevalence of 4–14 % [126]. Os trigonum is located adjacent to the posterior margin of the talus and has a prevalence of 14–25 % [126]. The mechanism of pain in the presence of an accessory tarsal bone has been attributed to traumatic or degenerative changes at the synchondrosis or to soft tissue inflammation. Symptomatic accessory tarsal navicular bones have been studied with bone scanning and MRI. Symptomatic lesions are reported to show increased radiotracer uptake or marrow edema across the synchondrosis. SPECT/CT provides an excellent technique for the evaluation of the cause of chronic pain in this situation (Fig. 8.14).
8.9 SPECT/CT and Infection/Inflammation
Plain radiographs remain the first-line investigation in diagnosis of osteomyelitis but are usually unremarkable in early stages of infection. MRI and 2/3-phase bone scintigraphy are the modalities of choice in this setting. MRI may assess the presence of osteomyelitis and associated soft tissue complications, and CT is useful to determine cortical destruction, sequestration, and involucra. Both of these modalities provide high-quality morphological data but are often nondiagnostic because structural changes underlying the infectious process are nonspecific or become detectable only in the subacute or late stages of the disease. Radionuclide imaging plays a significant role in the evaluation of patients with suspected infection, especially because of its potential for detecting metabolic alterations which precede morphological changes.
The major drawbacks of bone scintigraphy are the anatomical localization of the infection and nonspecific tracer uptake, both of which may be overcome by using SPECT/CT. Bar-Shalom et al. [128] investigated 89 patients with different conditions, such as fever of unknown origin, vascular graft infection, suspected osteomyelitis, and suspected soft tissue infection. Planar, SPECT, and SPECT/CT results were concordant for the diagnosis and location of infection in 50 % (41/82), and SPECT/CT could determine the precise anatomical location of infection in 85 % (35/41) of discordant studies. Hybrid imaging can distinguish blood pool activity from infectious foci, with significant advantages for assessment of suspected vascular graft infection as well as in patients with fever of unknown origin. WBC SPECT/CT was found to be more accurate than 67Ga SPECT/CT, probably because of its higher specificity and target to background ratio [128]. In this regard, 99m




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree