Figure 3-9. Normal sheath distension. [A] Positioning of the probe. [B] Corresponding axial 12-5 MHz US image shows the LHBBT (t) and normal amount of fluid in the most dependent portion of the sheath (asterisks). The cross-sectional area of the distended sheath is normal and estimated at four times the cross-sectional area of the normal LHBBT. Lt= lesser tuberosity. Gt= greater tuberosity.
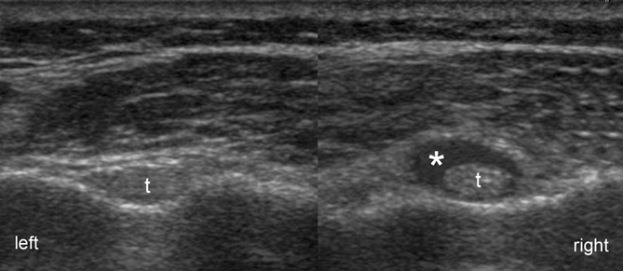
Figure 3-10. Normal sheath asymmetry in an asymptomatic healthy volunteer. Axial 12-5 MHz comparative image shows normal LHBBT (t) and slight asymmetric distribution of fluid in the most dependent portion of the sheath (asterisk). The small amount of fluid in the right side is considered normal and clinically irrelevant.
Simple fluid is usually anechoic, whereas complex fluid can be anechoic, hypoechoic, or hyperechoic (figure 3-11). Hypo- and hyperechoic fluid may resemble synovial proliferation on static images, but the findings of flow on Doppler US, poor compressibility, and lack of internal movements during graded compression suggest the latter rather than complex fluid. Meticulous technique is mandatory because excessive pressure with the probe can displace fluid and lead to a false-negative result for sheath distension (figure 3-12). It is also important to differentiate communicating joint effusion from tenosynovitis. Although pathological sheath distension accompanied by local pain during real time compression with the probe is commonly regarded as a manifestation of tenosynovitis, this association has not been sufficiently validated by controlled studies and its accuracy is uncertain. A more reliable strategy to differentiate communicating joint effusion from tenosynovitis is to carefully evaluate other glenohumeral joint recesses, because concomitant distension strongly suggests communicating joint effusion as the cause of sheath distension. Tenosynovitis, in turn, is suggested by coexistent hypoechoic swelling of the tendon (figure 3-13). Evaluation of tendon diameter and echogenicity is subjective and may require contralateral comparison (figure 3-14). Occasionally, tenosynovitis is depicted as isolated hypo-echoic swelling of the tendon (figure 3-15; video 3-4) or results in inflammatory erosion of the intertubercular groove (figure 3-16).23 The LHBBT sheath can also serve as a reservoir for loose bodies (figure 3-17).
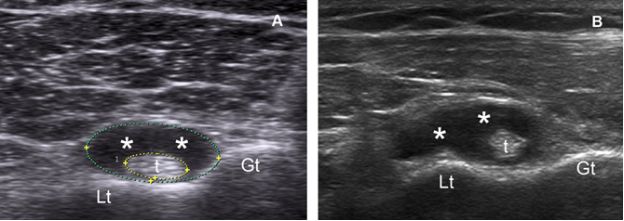
Figure 3-11. Tenosynovitis of the LHBBT. [A] Axial 12-5 MHz US image depicts fluid distension of the most dependent portion of the sheath (asterisks). The cross-sectional area of the distended sheath is estimated at six times the cross-sectional area of the normal LHBBT (t). [B] Axial 12-5 MHz US image obtained from another patient also depicts tenosynovitis of the LHBBT. Lt= lesser tuberosity. Gt= greater tuberosity.
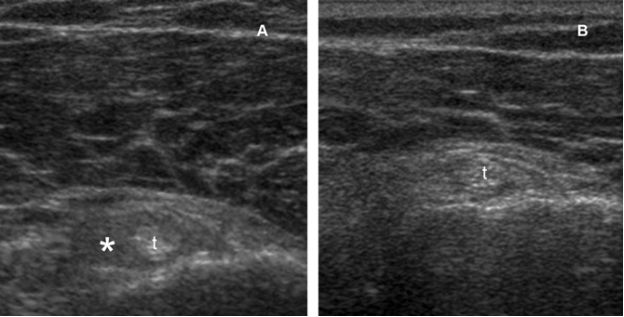
Figure 3-12. Pitfall. [A] Axial 12-5 MHz US image shows the LHBBT (t) and a small amount of echogenic fluid in the most dependent portion of the tendon sheath (asterisk). [B] Excessive compression with the probe squeezes the fluid away from the image plane and results in a false-positive study.
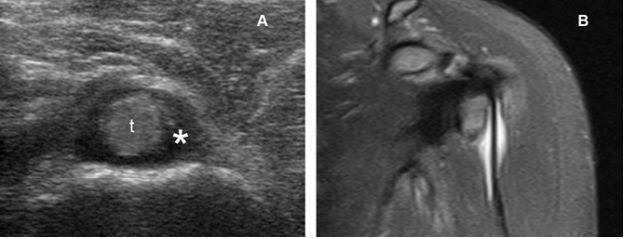
Figure 3-13. Tenosynovitis of the LHBBT. [A] Axial 12-5 MHz US image depicts hypoechoic swelling of the LHBBT (t) and fluid distension of the sheath (asterisk). [B] Corresponding coronal oblique STIR MRI confirms sonographic findings. Since MRI is obtained in decubitus, fluid within the LHBBT sheath does not accumulate distally.
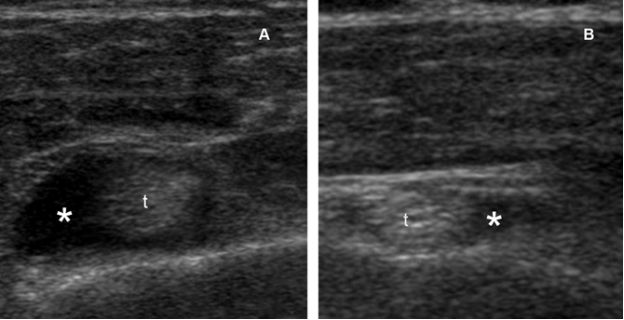
Figure 3-14. Tenosynovitis of the LHBBT. [A] Axial 12-5 MHz US image depicts hypoechoic swelling of the LHBBT (t) and increased fluid in the most dependent portion of the sheath (asterisk). [B] Contralateral comparison shows normal tendon and fluid.
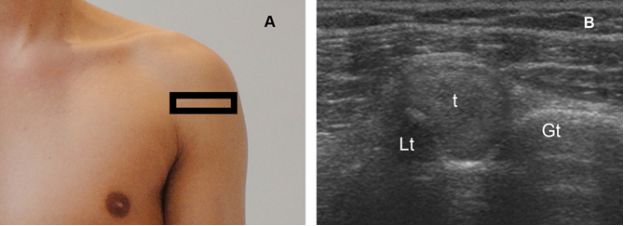
Figure 3-15. Tenosynovitis of the LHBBT. [A] Positioning of the probe. [B] Corresponding axial 12-5 MHz US image shows isolated hypoechoic swelling of the LHBBT (t). Lt= lesser tuberosity. Gt= greater tuberosity.
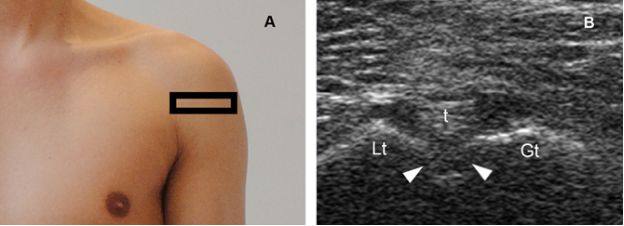
Figure 3-16. Inflammatory erosion of the intertubercular groove. [A] Positioning of the probe. [B] Corresponding axial 12-5 MHz US image shows normal LHBBT (t) and an inflammatory erosion of the intertubercular groove (arrowheads). Lt= lesser tuberosity. Gt= greater tuberosity.
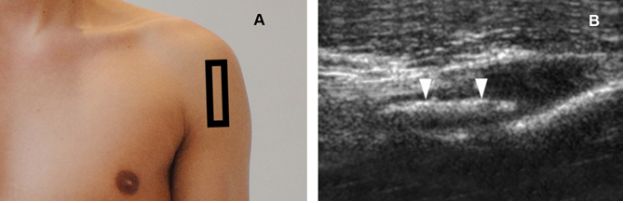
Figure 3-17. Osteochondral loose body. [A] Positioning of the probe. [B] Corresponding sagittal 12-5 MHz US image shows an echogenic loose body (arrowheads) with faint shadow inside the LHBBT sheath.
5.2. Partial Tears
Partial tears of the LHBBT are usually chronic and result from progression of tenosynovitis to a frank tear. Longitudinal fissures and splits are the most common types. These tears may either create an eccentric anechoic defect (figure 3-18) or split tendon into two symmetric (figure 3-19) or asymmetric cords (figure 3-20). Distal evaluation typically document reattachment of these lesions at the musculotendinous junction (video 3-5). Multiple axis views are necessary to differentiate split lesions from proliferating synovium because the latter may mimic two tendons on axial images (figure 3-21). Bifid tendon is an anatomical variant that may also simulate split tears. However, bifid tendon contains two individual mesotendons and this feature permits its differentiation from true tears (figure 3-22); another important feature in the differential diagnosis is that split tears generate two tendons that are half-diameter, while bifid tendon generates two full-diameter tendons (figure 3-23). A double tendon sheath containing bifid LHBBT and separated by a bony septum have also been described.24
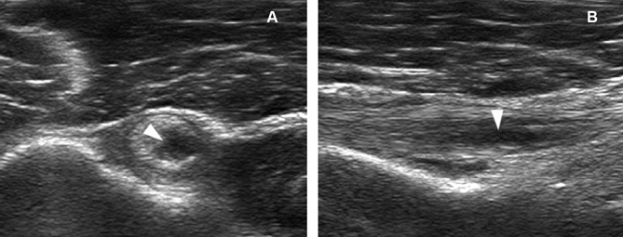
Figure 3-18. Partial tear of the LHBBT. [A] Axial 12-5 MHz US image shows an eccentric hypoechoic defect of the LHBBT (arrowhead). [B] Corresponding sagittal 12-5 MHz US image confirms a hypoechoic defect of the tendon (arrowhead).
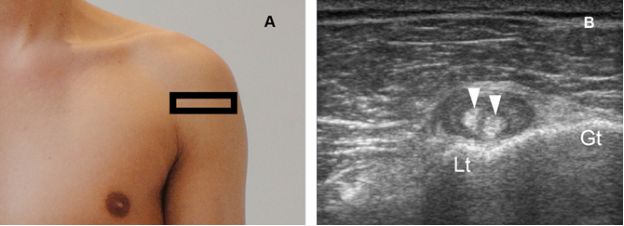
Figure 3-19. Partial tear of the LHBBT. [A] Positioning of the probe. [B] Corresponding axial 12-5 MHz US image shows longitudinal split of the LHBBT into two symmetric cords (arrowheads). Lt= lesser tuberosity. Gt= greater tuberosity.
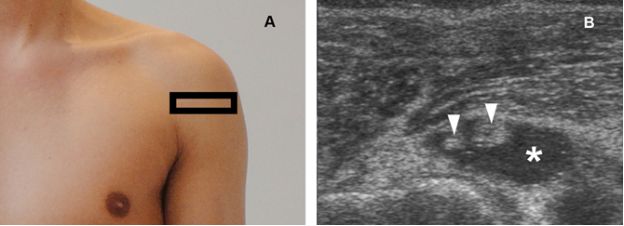
Figure 3-20. Partial tear of the LHBBT. [A] Positioning of the probe. [B] Corresponding axial 12-5 MHz US image shows longitudinal split of the LHBBT into two asymmetric cords (arrowheads) and fluid distension of the sheath (asterisk).
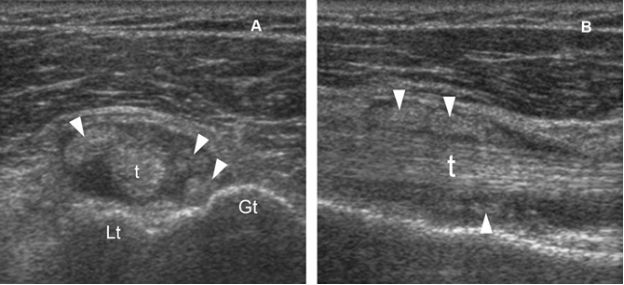
Figure 3-21. Pitfall. [A] Axial 12-5 MHz US image shows proliferating synovial tissue (arrowheads) mimicking a partial tear of the LHBBT (t). [B] Sagittal 12-5 MHz US image confirms proliferating synovial tissue (arrowheads) and no tendon tear. Lt= lesser tuberosity. Gt= greater tuberosity.
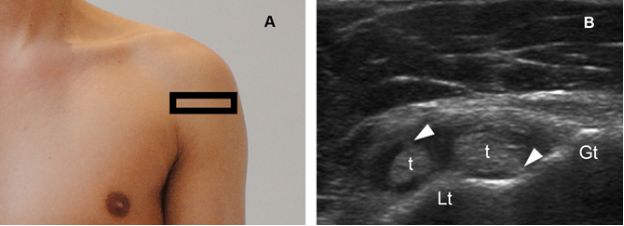
Figure 3-22. Bifid LHBBT. [A] Positioning of the probe. [B] Corresponding axial 12-5 MHz US image shows bifid LHBBT (t) and its mesotendons (arrowheads). Note also dislocation of the medial tendon over the lesser tuberosity (Lt). Gt= greater tuberosity.
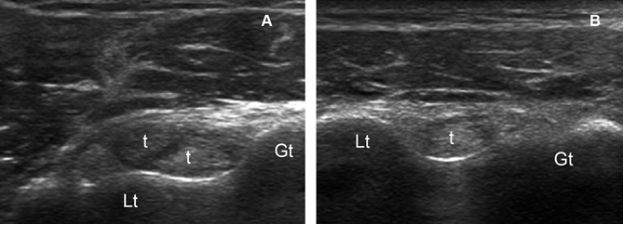
Figure 3-23. Bifid LHBBT. [A] Axial 12-5 MHz US image shows bifid LHBBT generating two full-diameter tendons (t). [B] Contralateral comparison shows normal LHBBT. Contralateral evaluation is useful to assess the size of the LHBBT and categorize the two tendons in the index shoulder as half-diameter or full-diameter. Lt= lesser tuberosity. Gt= greater tuberosity.
5.3. Complete Tears
Complete tears of the LHBBT usually occur in trauma setting and generate a soft-tissue mass in the anterior aspect of the arm, the so called Popeye sign, which paradoxically leads to a decreased strength during flexion and supination of the forearm. In the majority of cases, the clinical diagnosis is straightforward. US, however, may be useful when clinical findings are dubious. In recent complete tears, the gap left by the missing tendon is filled in by fluid (figure 3-24). Occasionally, bone spurs arising from the margins of the intertubercular groove may be depicted as a predisposing factor (figure 3-25). Ruptures at the musculotendinous junction can be missed if examination is restricted to proximal levels, since tendon retains its normal appearance at both rotator interval and intertubercular groove (figure 3-26). Careful evaluation distal to intertubercular groove is required to correctly diagnose these subtle injuries and typically reveals a bulbous biceps muscle as a result of retraction (video 3-6). In long-standing tears, the sonographic diagnosis is challenging because fluid is usually minimal or absent and the gap filled in by proliferating synovial tissue and collapsed tendon sheath that may mimic a heterogeneous but intact tendon, especially in older individuals. In such cases, refraction shadowing deep to the retracted tendon and contralateral comparison may be useful to provide a more intuitive diagnosis (figure 3-27).
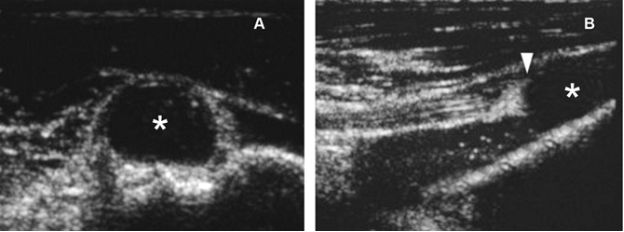
Figure 3-24. Complete tear of the LHBBT. [A] Axial 12-5 MHz US image at the distal level of the intertubercular groove demonstrates a fluid-filled empty sheath (asterisk). [B] Corresponding sagittal 12-5 MHz US image shows abrupt termination of the LHBBT (arrowhead) and a distal fluid-filled empty sheath (asterisk).
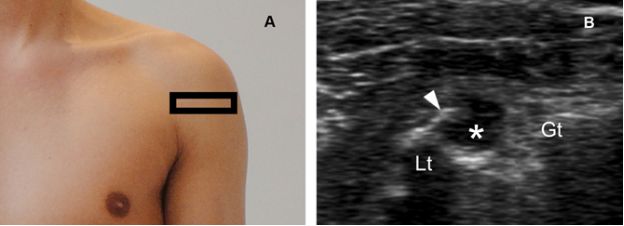
Figure 3-25. Complete tear of the LHBBT. [A] Positioning of the probe. [B] Corresponding axial 12-5 MHz US image shows a fluid-filled empty sheath (asterisk) secondary to a complete tear of the LHBBT. Note also a bone spur (arrowhead) arising from lesser tuberosity (Lt). Gt= greater tuberosity.
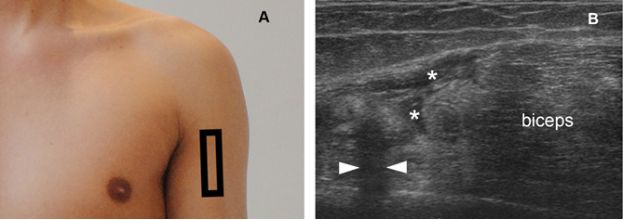
Figure 3-26. Complete tear of the LHBBT. [A] Positioning of the probe. [B] Corresponding sagittal 12-5 MHz US image shows a complete tear at the musculotendinous junction of the LHBBT surrounded by a thin layer of fluid (asterisks). Note also refraction shadowing deep to the retracted tendon (arrowheads) and distal muscle retraction (biceps).
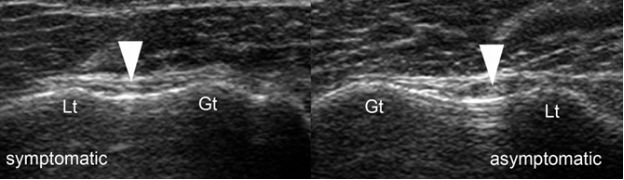
Figure 3-27. Complete chronic tear of the LHBBT. Comparative axial 12-5 MHz US image shows a complete chronic tear of the LHBBT in the symptomatic shoulder. The gap is filled in by collapsed tendon sheath that mimic a heterogeneous but intact tendon (arrowhead). Contralateral comparison shows normal tendon in the asymptomatic shoulder. Lt= lesser tuberosity. Gt= greater tuberosity.
When the LHBBT is not seen in the intertubercular groove, the differential diagnosis includes complete tears, tendon instability (see section 5.5) and prior surgery. Three popular surgical options for symptomatic LHBBT that can generate an empty intertubercular groove are tenotomy, tendon transfer, and tenodesis. Tenotomy consists of detaching the LHBBT from its labral origin. Transfer involves tenotomy plus suturing of the LHBBT to the conjoined tendon. Tenodesis involves tenotomy plus anchoring the LHBBT along its original course more distally.
Management of complete tears is conservative and surgery reserved for cosmetic reasons and patients who require full muscle strength for daily activities.
5.4. Ganglion
A ganglion is a common benign pseudocystic lesion filled with gelatinous material that is covered by multidirectional strata of collagen fibers and has no synovial lining.25-27 The distinction between ganglia and synovial cysts is microscopic and defined on the basis of the presence or absence of synovial lining, but these terms are loosely applied because imaging findings are similar and secondary changes in the capsule may make histologic differentiation difficult.28 Both ganglia and synovial cysts may communicate with the tendon sheath and this finding does not help in differentiating between these two lesions, but this information should always be reported to the referring physician because failure to resect such a communication invariably leads to recurrence.29-31 Also, both ganglia and synovial cysts frequently exhibit acoustic enhancement, although it may be difficult to demonstrate in small lesions close to the bone. On daily practice, we liberally use the term ganglion as a descriptive, not histopathological diagnosis.
Ganglia may occasionally arise from degeneration and rupture of the LHBBT sheath (figure 3-28). Ganglia may also occur within the LHBBT. Such lesions are rare and typically depicted as a central cavity (figure 3-29) or as multiple elongated cavities within the tendon (figure 3-30). Internal low-level echoes may represent artifact, hemorrhage, or the relative proportion of the constituents of mucin.32,33 The etiology of intratendinous ganglion is unclear but thought to involve mucoid degeneration of tendon tissue caused by overuse, chronic irritation, and/or chronic ischemia.34 Mucoid degeneration is associated with spontaneously ruptured tendons, and intratendinous ganglion may be a risk marker for tendon tears.35 Intratendinous ganglia can usually be distinguished from partial tears because the former creates a poorly compressible central cavity within the tendon, while the latter is typically depicted as a highly compressible eccentric defect (video 3-7). Differential diagnosis also includes giant cell tumor and xanthoma. However, these are solid masses that are usually easily differentiated from cysts at US.
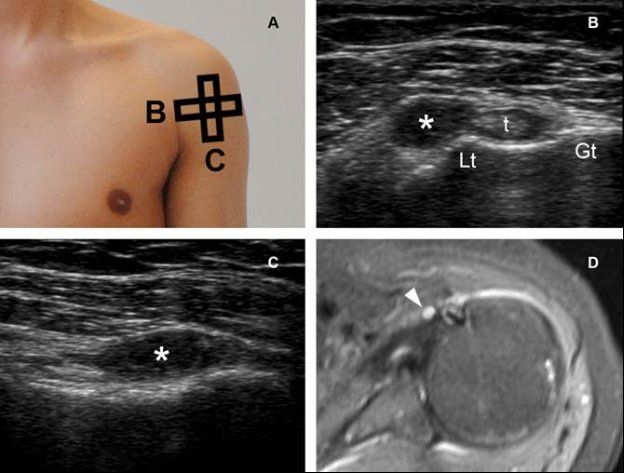
Figure 3-28. Ganglion originating from the LHBBT sheath. [A] Positioning of the probe. [B] Corresponding axial 12-5 MHz US image shows a well-defined pseudocystic lesion (asterisk) adjacent to the tendon (t). [C] Corresponding sagittal 12-5 MHz. [D] Corresponding axial STIR MRI confirms sonographic finding (arrowhead). Lt= lesser tuberosity. Gt= greater tuberosity.
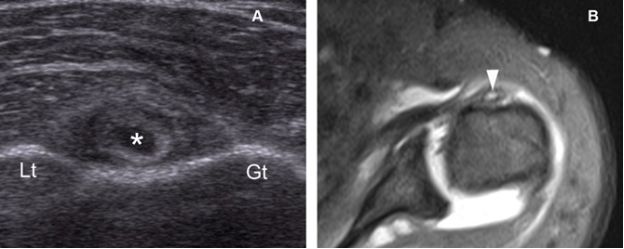
Figure 3-29. Intratendinous ganglion. [A] Axial 12-5 MHz US image shows a central cavity within the tendon (asterisk). [B] Corresponding axial STIR MRI shows the high signal intensity of the fluid-containing intratendinous ganglion (arrowhead). Lt= lesser tuberosity. Gt= greater tuberosity.
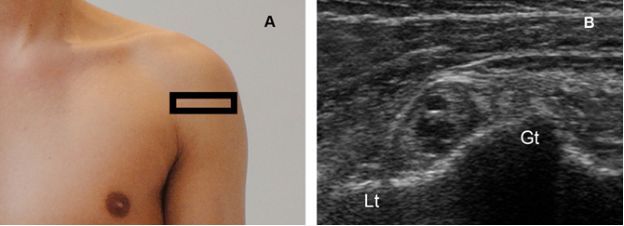
Figure 3-30. Intratendinous ganglion. [A] Positioning of the probe. [B] Corresponding axial 12-5 MHz US image shows multiple elongated cavities within the LHBBT. Lt= lesser tuberosity. Gt= greater tuberosity.
Studies on the natural history of untreated ganglia are lacking. Changes in ganglion size are common at follow-up and may reflect repeated cycles of rupture and expansion, which may explain multiple septations frequently seen in chronic lesions.33 It is important to describe the presence of septations in the sonographic report because this finding may preclude successful needle aspiration.
5.5. Tendon Instability
In general, LHBBT instability can be classified as dislocation and subluxation. Subluxation is defined as a tendon proximally fixed over the apex of the lesser tuberosity and distally recentered into the intertubercular groove (figure 3-31). It occurs at first cranially, at the rotator interval level, but a reliable diagnosis can be made only when the tendon overlies the lesser tuberosity (figure 3-32). Dislocation is defined as the total loss of contact between the tendon and the intertubercular groove (figure 3-33). Injury to the biceps reflection pulley is necessary for tendon dislocation to occur and may be secondary to acute trauma, repetitive chronic microtrauma, degenerative changes, or concomitant rotator cuff tear.36,37 Dislocations can be further classified depending on the subscapularis tendon status into intra-articular, intratendinous, and superficial subtypes (figure 3-34). Intra-articular subtype is the most common form of LHBBT dislocation (videos 3-8 and 3-9). In these cases, dislocated LHBBT is positioned deep to an associated complete tear of the subscapularis and adjacent to the humerus (figure 3-35). In the uncommon case of superficial dislocation, the LHBBT rests superficial to intact subscapularis (figure 3-36; video 3-10). Intratendinous dislocations are exceedingly rare and occur when LHBBT penetrates into a delimitative partial tear of the subscapularis. Once dislocated, the LHBBT tends to remain displaced. However, dynamic evaluation is always recommended because internal rotation relocates the tendon into the intertubercular groove and abnormal tendon position may only occur with maximal external rotation of the shoulder. Partial tears of the LHBBT, abnormalities in the supporting structures at the rotator interval (figure 3-37), and bone spurs may be associated findings (figure 3-38).
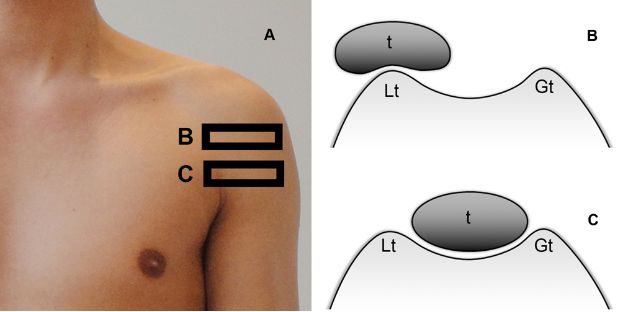
Figure 3-31. Medial subluxation of the LHBBT. [A] Imaging plane. [B] Corresponding schematic drawing demonstrates the LHBBT (t) located over the apex of the lesser tuberosity (Lt) at the proximal level of the intertubercular groove. [C] Corresponding schematic drawing shows the LHBBT recentered distally into the intertubercular groove. Gt= greater tuberosity.
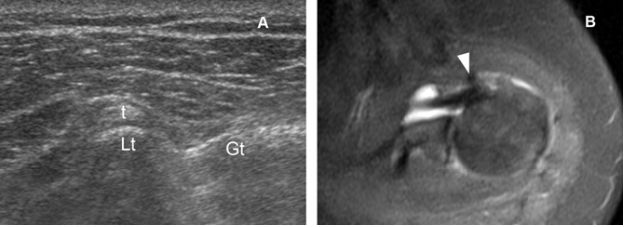
Figure 3-32. Medial subluxation of the LHBBT. [A] Axial 12-5 MHz US image shows the LHBBT (t) located over the apex of the lesser tuberosity (Lt) at the proximal level of the intertubercular groove. [B] Corresponding axial STIR MRI confirms sonographic finding (arrowhead). Gt= greater tuberosity.
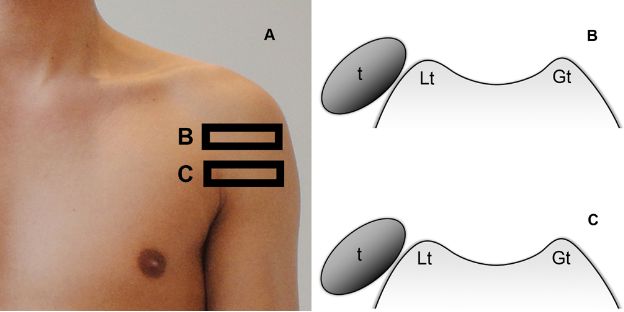
Figure 3-33. Medial dislocation of the LHBBT. [A] Imaging plane. [B,C] Corresponding schematic drawings demonstrate total loss of contact between the LHBBT (t) and the intertubercular groove. Lt= lesser tuberosity. Gt= greater tuberosity.
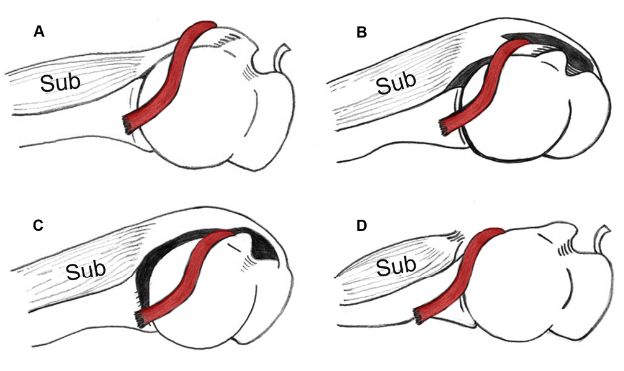
Figure 3-34. Types of LHBBT dislocation. Schematic drawing of an axial view of the right shoulder viewed from above. [A] Medial superficial dislocation. [B] Medial intratendinous dislocation. [C] Medial intra-articular dislocation. [D] Medial intra-articular dislocation. Red= LHBBT. Sub= subscapularis.
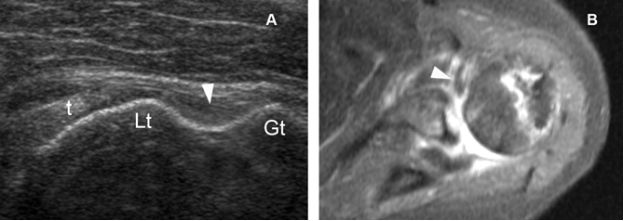
Figure 3-35. Medial intra-articular dislocation of the LHBBT. [A] Axial 12-5 MHz US image shows the LHBBT (t) located medial to the lesser tuberosity (Lt), adjacent to the bone cortex. Note also an empty intertubercular groove (arrowhead). Occasionally, the dislocated tendon may be difficult to identify because of its deep location. [B] Corresponding axial STIR MRI shows the dislocated LHBBT (arrowhead). Gt= greater tuberosity.
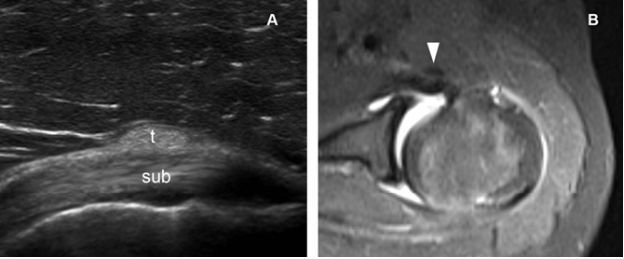
Figure 3-36. Medial superficial dislocation of the LHBBT. [A] Axial 12-5 MHz US image shows the LHBBT (t) located superficial to the normal subscapularis tendon (sub). [B] Corresponding axial STIR MRI shows the dislocated LHBBT (arrowhead).
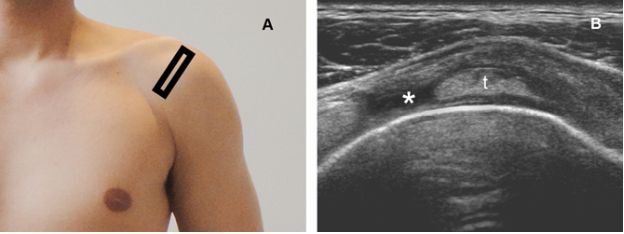
Figure 3-37. Tear of the superior glenohumeral ligament at the rotator interval. [A] Positioning of the probe. [B] Corresponding 12-5 MHz US image shows the normal LHBBT (t) and a tear of the superior glenohumeral ligament (asterisk) at the rotator interval.
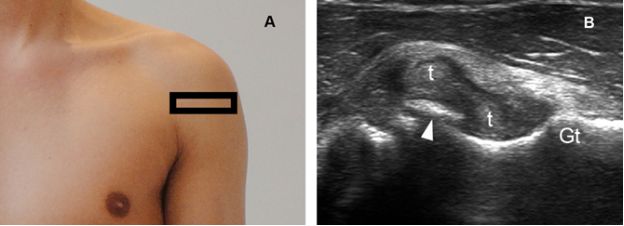
Figure 3-38. Concomitant partial tear and subluxation of the LHBBT. [A] Positioning of the probe. [B] Corresponding 12-5 MHz US image shows a longitudinal split of the LHBBT into two cords (t). Note also subluxation of the medial cord over a bone spur arising from lesser tuberosity (arrowhead). Gt= greater tuberosity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree