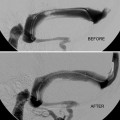
Fig. 1
(a) Patient affected by left posterolateral herniated disc at level C5–C6: scheme of anterolateral approach to foraminal space; (b) Fluoroscopic-guided needle placed into left foraminal at level C6–C7 with oblique tube orientation. (c) Fluoroscopic-guided needle placed into right foraminal at level L5–S1 in patient in prone position
For epidural injection, the needle is advanced into the epidural space by dorsal, oblique (20–30° caudal and lateral to the midline), and paramedian approach up to the superior margin of the spinal lamina, just subjacent to the interlaminar gap; then the needle can be pushed over the lamina, through the ligamentum flavum into the dorsal epidural space at the midline.
For foraminal injection, a lateral angle greater than that used for the interlaminar technique, generally 35–45° from the midline, is used.
The drug will be injected slowly to avoid reflux near the needle.
An injection of oxygen-ozone therapy (10 mL of 30 μg/mL at lumbar area and 3–4 mL at cervical area) can be performed after steroid injection to increase the anti-inflammatory and analgesic action.
At lumbar level, it is suggested to add a local anesthetic (just 1 cc of lidocaine 1 %), while this is never performed at the cervical level to prevent epidural diffusion with respiratory distress.
Patients do not require hospitalization and can be mobilized after the procedure without need of any other medical treatment.
Good outcome short-term results up to a rate of 40–65 % are achieved while the results at long-term follow-up are lower.
Epidural Injection
Epidural injection of corticosteroids with or without anesthetic drug is another therapy option commonly used in managing chronic spinal pain. Targets are patients suffering from back or neck pain with or without radiculopathy.
All patients must be studied by CT and/or MRI before the treatment to clearly evaluate the pathology.
The technique can be performed with the patient in the prone position by three different approaches:
The transforaminal approach is target specific and requires the smallest volume to reach the primary site of pathology, specifically, the anterolateral epidural space as well as the dorsal root ganglion (Fig. 1b–c).
The interlaminar entry can be directed more closely to the assumed site of pathology, requiring less volume than the caudal route (Fig. 2).
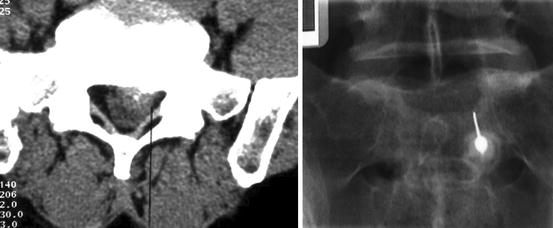
Fig. 2
CT scheme of translaminar approach; fluoroscopic-guided needle placed into right epidural space by translaminar approach at level L5–S1 in patient in prone position
The caudal entry is relatively easily achieved with minimal risk of inadvertent dural puncture, but requires a relatively high volume (10–20 mL) of injectate to reach the site of pathology.
The mechanism of action of epidurally administered steroid with or without local anesthetic injections is well understood. The achieved neural blockade alters or interrupts nociceptive input, reflex mechanisms of the afferent fibers, self-sustaining activity of the neurons, and the pattern of central neuronal activities. Conversely, the local anesthetic interrupts the pain-spasm cycle, and reverberating nociceptor transmission, the corticosteroids reduce inflammation by inhibiting either the synthesis or release of a number of pro-inflammatory mediators and by causing a reversible local anesthetic effect.
A radiopaque marker is used to identify the skin entry point and a sterile fashion is recommended.
For the epidural approach, with the patient in the prone position under fluoroscopic or CT guidance, a 22-gauge spinal needle is advanced into the epidural space via a dorsal, oblique paramedian approach. The puncture site is typically 2–4 cm from the midline and 2–3 cm caudal to the intended point of entry into the dorsal epidural space.
An 18-gauge venipuncture needle is placed from a puncture site 2–3 cm from the midline and without caudal offset over the desired interlaminar gap. An epidural needle with a blunt tip and side hole is then passed through the introducer needle to the midline dorsal epidural space. After the needle is placed, contrast material can be injected for epidurography, followed by therapeutic injection.
For transforaminal epidural injection, the patient is placed in the prone position on the fluoroscopy/CT table. The skin is marked with the C-arm/CT tube oriented posterolaterally approximately 308–458 and with craniocaudal angulation to profile the caudal undersurface of the pedicle above the target foramen. For sacral foramen (S1 or S2) injections, a dorsal approach from directly above the appropriate foramen is used, and the same injection technique is employed.
For caudal (sacral hiatus) epidural injection, the patient is place in the prone position, so the sacral hiatus can be palpated and visualized fluoroscopically. A fenestrated drape is placed and a 22-gauge spinal needle is advanced ventrally and rostrally at the midline to the sacral hiatus.
For cervical and thoracic epidural injection, the patient is always placed in the prone position and the skin is marked 1–2 cm from the midline, slightly caudal to the interlaminar gap. The C-arm fluoroscopic axis is angled 108–158 off midline and caudal for this alignment. After sterile preparation and draping, 1–3 mL of 1–2 % lidocaine is injected subcutaneously for local anesthesia. The skin is then punctured and an epidural needle is advanced to the dorsal midline epidural space and just 2–5 mL of steroid can be injected. Anesthetic agent is not injected into the cervical epidural space to avoid the risk of respiratory suppression resulting from high cervical anesthesia.
For lower thoracic injections (T7 to T8 or below), 3–5 mL of 1 % lidocaine can be injected after instillation of the steroid suspension.
Facet Joint Analgesic Injection
The facet joints [zygapophyseal or z-joints (FJ)] are paired synovial joints at the posterior aspect of the spinal column. Each joint consists of the articulation between adjacent superior and inferior articular processes arising from adjacent vertebrae. They make a tripod support for each spinal level with the intervertebral disc.
Approximately 30 % of patients affected by LBP, 55 % by NP, and 40 % with thoracic pain experience chronic spinal pain due to facet syndrome.
Causes of facet syndrome include trauma, arthritis, inflammatory, and especially degeneration.
FJ is manifested as axial low back or neck pain or headache; axial pain of thoracic level is less common.
Symptoms are nonspecific and overlap with other diseases (cerviogenic headache, shoulder, or scapular pain).
Clinical investigations include:
Pain aggravated by palpation of paraspinal muscles, standing, spinal extension, and facet joint loading with rotation with ameliorated by sitting and flexing the spine.
Morning pain and stiffness.
Occasional improvement with anti-inflammatory drugs.
Diagnosis is done by exclusion criteria ruling out other causes of LBP or NP like vertebral body fracture, herniated disc, spinal stenosis, spondylolisthesis, and nerve entrapment.
Imaging is not specific or sensitive. Degeneration and hypertrophy facet finding or accumulation of fluid in the joint capsule or MRI enhancement locally about facet joint can suggest FJ.
In acute pain, medical conservative therapy is suggested, but if it fails after 6–12 weeks, an FJ syndrome can be considered.
If there is pain relief after administration of local anesthetic directly into the joint capsule, a diagnosis of FJ syndrome can be made.
The technique consists of injection of steroid drugs (1 cc of Depo-Medrol 20–40 mq) plus 1 cc lidocaine 1 % directly into facet joint with antalgic long effect under CT or fluoroscopic guidance and the patient in the prone position with an 18–20- or 22-gauge Chiba needle.
A radiopaque marker is used to identify the skin entry point and a sterile fashion is recommended.
The orientation of the needle rides on the orientation of each joint. The cervical facet joints are typically oriented in an oblique coronal plane angled superior to inferior in a posterior direction. The thoracic facet joints are nearly vertical and coronal in orientation. The superior lumbar facet joints are oriented in a nearly sagittal plane.
CT guidance is easier than fluoroscopy to identify the correct orientation to approach to facet joint.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree