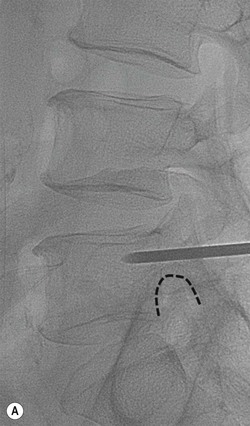
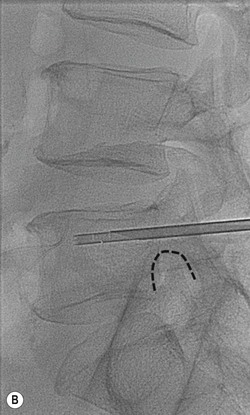
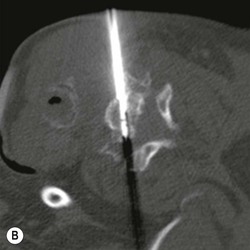
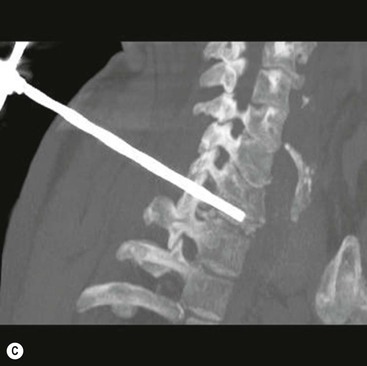
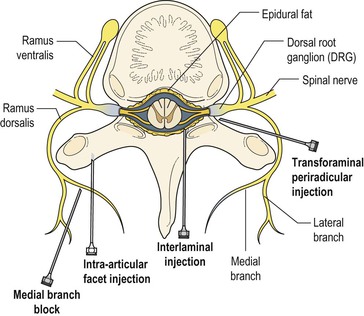
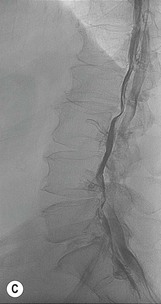
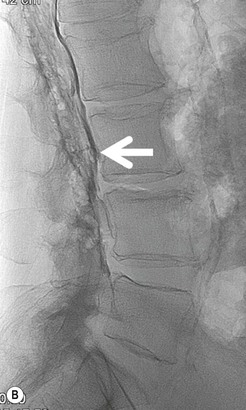
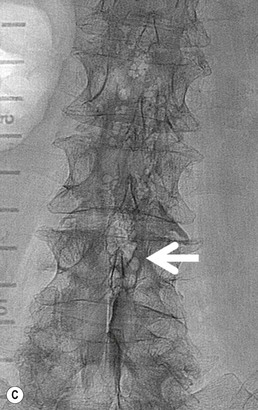
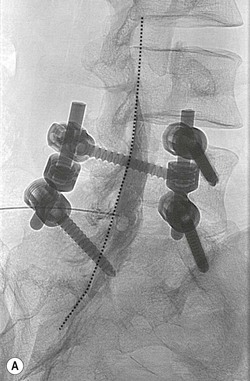
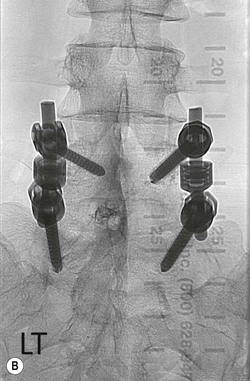
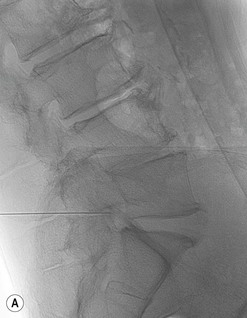
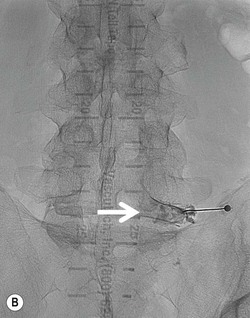
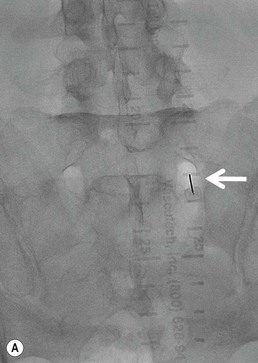
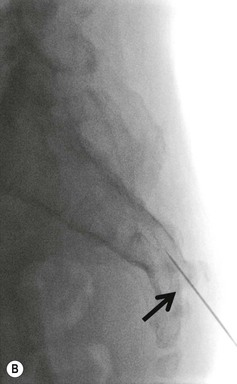
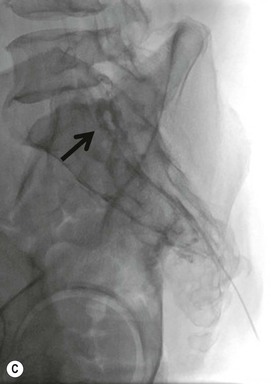
Konstantinos Katsanos, Tarun Sabharwal Spinal interventional procedures are used in the diagnosis and treatment of various spinal pathologies of benign or malignant origin. Procedures described in the present chapter are performed by interventional radiologists, who work within a wider multidisciplinary team of clinical specialists that may include neurosurgeons, orthopedic surgeons and oncologists. Interventional radiologists are appropriately trained to carry out spinal intervention with minimal risks, and can manage any relevant procedure-related complications. Vertebral bone biopsy is a minimally invasive percutaneous procedure with the advantages of low cost, low morbidity, high accuracy and repeatability and it has replaced open surgical biopsy in most cases. Fluoroscopy-guided bone biopsy was first described in the 1970s and image-guided bone biopsy is today a critical part of the management of musculoskeletal lesions, including primary tumours, bone metastases and bone infections. Spinal applications include image-guided biopsy of the vertebrae, the sacrum and the iliac bones. Disc aspiration for the investigation of spondylodiscitis is also widely practiced. Under X-ray guidance a biopsy needle can be used to access and sample small lesions in difficult anatomies, such as the vertebral body or intervertebral discs, without surgical exploration. Before considering an image-guided spinal biopsy all relevant medical history, laboratory tests and relevant imaging findings must be analysed thoroughly and discussed with the multidisciplinary team. The multidisciplinary team usually includes the spinal neurosurgeon, the musculoskeletal radiologist, the responsible oncologist and an experienced cytopathologist. Correlation with plain films and MRI is critical to avoid unnecessary procedures in certain benign lesions with typical imaging appearances (‘do not touch lesions’). Well-recognised and accepted indications and contraindications for spinal biopsies are outlined in Table 93-1. In general, spinal biopsy is indicated to identify tumour or infection. If bone metastasis is suspected, biopsy should be undertaken only if the result will influence oncologic management. Spinal biopsy may also be considered for tumour staging, or to compare histological characteristics in patients with synchronous or metachronous metastatic cancer. Primary musculoskeletal tumours require identification, grading and often cytogenetic analysis to determine appropriate treatment strategies and prognosis. Bleeding diathesis is the only absolute contraindication to spinal biopsy as it can cause severe haemorrhage or epidural haematoma that may compromise the spinal cord. Alternative options and the risk–benefit ratio should be considered in all patients with spinal lesions that are difficult to access percutaneously. TABLE 93-1 Image-Guided Vertebral Bone Biopsy: Indications and Contraindications Correction of coagulopathy, informed consent and consideration regarding conscious sedation or general anaesthesia constitute key elements of preoperative assessment for all spinal biopsy procedures. Anticoagulants like warfarin and heparin must be stopped prior to the procedure per local institutional policy and a platelet count below 50,000/mL must be corrected with adequate platelet transfusion. Bleeding diathesis with an international normalised ratio (INR) higher than 1.3–1.5 may be reversed with transfusions of fresh frozen plasma or cryoprecipitate as needed. Antiplatelet agents must be stopped in all cases of spinal interventions at least 5 days prior to the procedure to correct platelet dysfunction. Image guidance may be real-time plain fluoroscopy based on bony landmarks or computed tomography (CT), which offers higher soft tissue resolution, but is not real time. There are several different routes for performing an image-guided spinal biopsy depending on lesion anatomy and size. Typically, patients are placed in a prone or lateral decubitus position. The transpedicular or posterolateral approach is often used for lumbar vertebral body biopsy (Fig. 93-1). The intercostovertebral approach is usually indicated for the thoracic spine and an anterolateral approach with manual displacement of the large vessels is recommended for the cervical spine (Fig. 93-2). Fluoroscopic guidance is the modality of choice for the majority of spinal procedures and may be supplemented by CT for cervical lesions (Fig. 93-3). Biplane fluoroscopy or rotational flat panel angiography with cone beam CT capabilities are emerging modalities for enhanced image guidance during difficult spinal procedures. CT fluoroscopy is readily available in many institutions, but is generally avoided because of the increased radiation exposure. An oropharyngeal approach is indicated for biopsy of C1 or the dens. A posterior oblique CT-guided approach is usually chosen for biopsy of the pedicles and the other posterior spinal elements or the surrounding soft tissues. The access route will also depend on the image-guidance modalities available. Beware that certain musculoskeletal tumour lesions may be eligible for curative surgical resection; thus certain anatomical compartments, not involved by the tumour, must not be breached by the biopsy needle. This is especially true for soft tissue sarcomas and osteosarcomas to limit local recurrence after resection. Nevertheless, the risk of tract seeding following musculoskeletal fine needle aspiration is very low, estimated at 3–5/100,000 cases. Routine monitoring of vital signs is necessary during all spinal procedures. Percutaneous vertebral biopsy is a painful procedure because of osseous puncture and conscious sedation is necessary. Sedation is routinely administered using a combination of fentanyl and midazolam according to national and international guidelines. General anaesthesia may be necessary on a case-by-case basis. In patients with multiple spinal metastatic lesions, the largest and most easily accessible lesion should be chosen. The integrity of the underlying weight-bearing bone must also be considered, although the risk of post-biopsy iatrogenic vertebral fracture is very low. In patients with painful vertebral pathologic fractures, consideration of palliative cementoplasty following successful histologic analysis is worthwhile to improve quality of life. Bone sampling may be accompanied by sampling of adjacent soft tissues, and percutaneous disc biopsy may include biopsy of the neighbouring subchondral vertebral endplates to increase diagnostic yield. When planning a vertebral biopsy, mixed sclerotic-lytic or contrast-enhancing lesions are preferred as target lesions compared to hypodense or cystic areas that often contain necrotic components. Beware of certain spinal lesions, such as renal cell carcinoma metastases and haemangiomas, which may be highly vascular and can be associated with an increased risk of haemorrhagic complications. Different specimens must be sent for histology, cytopathology and microbiology. With regard to needle choice, the length of the needle (10–20 cm long) must be appropriate to the depth of the lesion. Spinal bone biopsies require use of 11–15G trephine needles that obtain an adequate core of bone marrow. Spinal trephine needles are inserted through a matching outer cannula that is hammered to penetrate the osseous cortex, as necessary. Routine 16–20G core biopsy cutting needles are used in patients with tumours that have a soft tissue component or extensive osteolysis. Fine needle aspiration with a 20–22G needle (Chiba needle) is usually enough for sampling intervertebral discs and aspiration of collections. Larger bore needles are preferred for percutaneous biopsy of the vertebrae because of their rigidity and ability to be hammered or drilled into the bone. Automated drilling biopsy guns have recently been made available for routine bone marrow biopsy and can be used in patients with bony lesions that have a thick overlying cortex. Depending on the indication, trephine core biopsy for histology may be combined with coaxial fine needle aspiration for cytology and microbiology. Reported diagnostic accuracy of spinal bone biopsies is above 95%, but there is always a small risk of a non-diagnostic outcome because of insufficient tissue sampling or sampling of necrotic or sclerotic areas. Diagnosis of spinal metastatic tumours is considered generally easier than primary bone tumours, but diagnostic yield also depends on lesion size and accessibility. In general, more than three needle passes are recommended to obtain an adequate volume of tissue and increase biopsy success. Multiple core biopsies are required for diagnosis of lymphoma, whereas fine needle aspiration may suffice for the diagnosis of metastasis and infection. Large core trephine biopsy is indicated for investigation of primary spinal tumours like osteoblastomas. The diagnostic accuracy of percutaneous disc biopsy for the investigation of infectious spondylodiscitis is around 50% and the rate of negative cultures may well exceed 60%, even when paravertebral or intervertebral disc fluid collections are aspirated. The most commonly isolated pathogen in infectious spondylodiscitis is blood-borne Staphylococcus aureus, and empirical antibiotic treatment may be initiated even without definite diagnosis. Antibiotics can be stopped 24–48 h prior to tissue sampling to increase diagnostic yield from fluid cultures. Lumbosacral radicular pain is defined as pain radiating to one or more lumbar or sacral dermatomes caused by nerve root compression producing irritation and inflammation. The pathology is also known as sciatica or nerve root pain. Radiculitis (only radicular pain) should be distinguished from radiculopathy that includes objective findings of sensory or motor disturbance. Lumbosacral radicular pain is the commonest form of neuropathic pain with an annual prevalence of 9.9–25% in the general population. Pain usually resolves spontaneously in two-thirds of patients within 12 weeks of onset. However, almost a third of patients continue to suffer from radicular pain after 3 months to 1 year. Before the age of 50 the most frequent cause is disc herniation, while after the age of 50 degenerative spine changes are more prevalent. Radiating pain may be sharp, stabbing, throbbing or burning and diagnosis is based on medical history and medical examination. Dermatomal distribution, pain that increases while bending forward or coughing, and a positive Laségue or crossed Laségue test are the usual clinical findings. Disc herniation most commonly occurs in the L4–L5 (around 30%) and L5–S1 (around 50%) intervertebral segments and the L4, L5 and S1 roots are the ones most commonly affected. MRI may confirm the presence of a disc herniation, but the specificity of the examination is very low because incidental disc herniations are detected in 20–36% of asymptomatic individuals. Selective segmental nerve blocks, whereby a specific nerve root is anaesthetised via an image-guided transforaminal injection of a small amount of lignocaine, may be helpful in excluding one level if negative, but positive blocks are considered non-specific because of significant overlap between innervation of adjacent segments. Transforaminal blocks may simultaneously block afferent input from the corresponding nerve root, the sinuvertebral nerve that innervates the intervertebral disc anteriorly and the dorsal ramus that innervates the facet joint and the muscles posteriorly at the same level. Therefore, differential diagnosis between true radiculitis, discogenic low back pain and mechanical facetogenic low back pain may be difficult. It is crucial that any red flags (trauma, cancer and infection) are excluded during diagnostic workup of the patient. Watch out for a previous medical history of cancer or unexplained weight loss, structural spinal deformities, symptoms appearing before the age of 20 or after 50 and acute neurological deficits that may require urgent surgical decompression. For example, a patient with acute cauda equina syndrome with saddle anaesthesia, sacral polyradiculopathy and sphincter dysfunction must be referred for emergent surgery. Spinal epidural injections with local anaesthetic and corticosteroids are generally indicated in patients with ongoing lumbosacral radicular pain who have failed conservative therapy with non-steroidal anti-inflammatory drugs (NSAIDS), early mobilisation and physiotherapy for at least 6–12 weeks. The primary indication is local compression of a nerve root or exiting spinal nerve by intervertebral disc herniation confirmed by CT or MRI. Spinal injections are also indicated for pain relief in patients with failed back surgery syndrome (FBSS) and degenerative spinal canal stenosis and in elderly patients who are not surgical candidates. The pathophysiology of sciatica combines mechanical nerve compression and the local release of pro-inflammatory mediators such as prostaglandins, nitrous oxide, phospholipase A2 and cyclooxygenase-2. The rationale for epidural corticosteroid injections is based on their potent anti-inflammatory properties. Epidural steroid injections are contraindicated in pregnancy, active peptic ulcers and uncorrectable coagulopathy and caution should be exercised in patients with diabetes and osteoporosis. Approaches to epidural peri-radicular injections include (1) the classical interlaminar, (2) the targeted transforaminal and (3) the caudal approach. Transforaminal epidural injection of steroids is reported to provide the best results in patients with segmental radicular symptoms. Compared to the posterior interlaminar approach, the transforaminal approach may achieve more precise delivery at the level of the inflamed root and the drugs may theoretically reach the interface between the disc hernia and the compressed nerve root at the ventral epidural space, more easily. The interlaminal approach may be chosen in posterolateral disc herniations, while the transforaminal approach is usually preferred for foraminal and extraforaminal herniations. However, transforaminal injections can be associated with rare neurological complications, including paraplegia in the lumbar spine and tetraplegia or death in the cervical spine (discussed later). Either fluoroscopy or computed tomography (CT) may be used for image guidance. The latter has the advantage of superb soft tissue contrast resolution, but fluoroscopic guidance is faster and allows for real-time control of needle advancement and drug injection to avoid complications (Fig. 93-4). When a fluoroscopic-guided interlaminal epidural injection is used, the patient is positioned in the prone position or in the decubitus foetal position based on operator preference. The correct intervertebral segment is identified using fluoroscopic guidance and bone landmarks. Cranial angulation of the tube usually helps to adjust for the lordosis of the lumbosacral junction. Typically, a 22G spinal needle (alternatively an 18- to 20G Tuohy needle) is used to enter the interspinous and the flavum ligaments. The latter consists almost entirely of collagen fibres and provides the greater resistance to the needle. Entry to the dorsal epidural space is confirmed with the loss of resistance technique and may be confirmed with the injection of an aliquot of contrast agent. Operators must be familiar with the different imaging features of contrast material patterns between intrathecal (myelography) and epidural (epidurography) injections (Fig. 93-5). The paramedian interlaminal approach with the needle pointing towards the affected side is recommended for more targeted injections (Fig. 93-6). In this case a contralateral oblique projection is used to monitor advancement of the needle and the needle tip enters the epidural space when it crosses the imaginary spinolaminar line (Fig. 93-7). When a fluoroscopic-guided transforaminal epidural injection is used, the patient is positioned prone and the C-arm is rotated to an ipsilateral oblique projection until the ipsilateral facet column is superimposed midway between the anterior and posterior wall of the vertebral bodies (‘scotty dog’ projection). The tube may also need to be angled cranially to align the superior and inferior vertebral endplates for the lower lumbar levels. Using tunnel collimation a 22- to 25G needle is advanced into the intervertebral foramen. The needle must slip along the lateral border of the respective facet joint and enter the dorsocranial quadrant of the intervertebral foramen (Figs. 93-8, 93-9). On scotty dog projections the needle target is actually below the junction of the pedicle and the ipsilateral transverse process (‘eye of the scotty dog’) and lateral to the inferior articular process of the respective facet joint. The depth of the needle is checked periodically in a lateral projection and elicitation of paresthesia (provoked by puncture of the spinal nerve) is best avoided. Some authors refer to the so-called ‘safe triangle’ when describing bone landmarks used for transforaminal periradicular nerve injections. On an ipsilateral oblique projection, the triangle is an imaginary triangular area formed cranially by the pedicle and transverse process, laterally by a line connecting the lateral edges of the superior and inferior pedicle and inferomedially by the spinal nerve root, which serves as the tangential base of the triangle. Once the needle tip is in the correct position, contrast medium is injected to outline the nerve sheath of the exiting root and exclude intrathecal, intra-arterial or intravenous injections (Fig. 93-10). After correct opacification of the epidural fat surrounding the spinal nerve, 1 mL of local anaesthetic is injected (bupivacaine 0.5% or lignocaine 1–2%) followed by a dose of steroid. In selective cases the caudal approach through the sacral hiatus may be chosen (Fig. 93-11).
Spinal Interventions
Introduction
Image-Guided Vertebral Biopsy
Patient Preparation
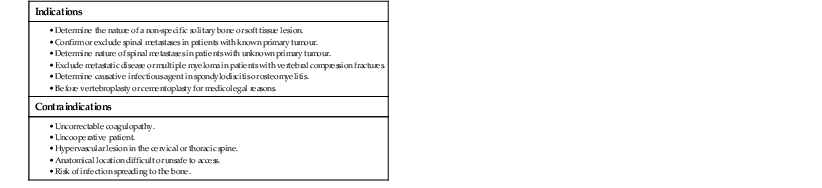
Image Guidance
Performing the Procedure
Results
Spinal Injection Procedures
Lumbar Disc Herniation
Indications
Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Spinal Interventions
Chapter 93