Clinical Presentation
The patient is a 77-year-old man who presented with chronic low back pain. The patient has had progressive low back pain with radiation into both hips and buttocks over the last 5 years. The pain is made worse with movements and transitions from sitting to standing. He cannot walk more than 50 yards before he begins to feel deep low back aching. He states that he has to lean forward on a shopping cart to support himself while he does his grocery shopping. He also states that this forward flexed position tends to diminish his pain. The patient denies any bowel or bladder symptoms. On examination, straight leg raising maneuvers were negative. The patient was able to flex at the waist 90 degrees but extend only 10 degrees.
Imaging Presentation
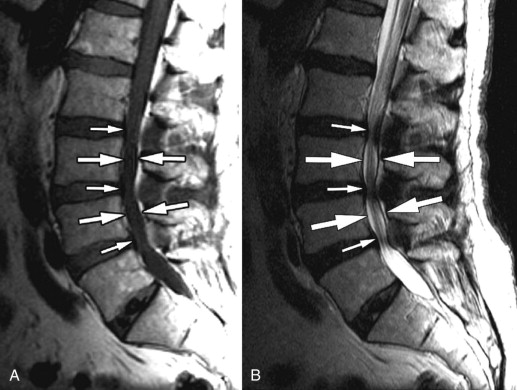
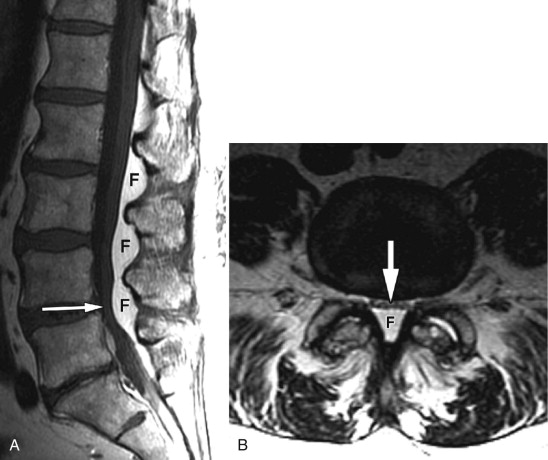
Sagittal T1-weighted and T2-weighted magnetic resonance (MR) images demonstrate a long segment of narrowing of the central spinal canal without evidence of disc herniation, discogenic degenerative changes, or prominence of the epidural fat. The patient’s underlying abnormality is congenital narrowing of the lumbar spinal canal secondary to short pedicles. This patient is at a disadvantage because his small disc bulges at L2-3, L3-4, and L4-5 has converted him from asymptomatic to severely symptomatic ( Fig. 72-1 ) .
Discussion
Lumbar spinal stenosis can be defined as any narrowing of the spinal canal that causes compression of its contents because of a mismatch between the available space in the spinal canal and its contents. There are three categories of lumbar spinal stenosis: congenital, developmental, and acquired. Most clinicians combine congenital and developmental stenosis. Congenital/developmental stenosis is usually caused by short pedicles. As a person ages, degenerative changes ensue. Normally, a person would not be symptomatic from degenerative changes until they were moderate or severe. However, with short pedicles, one tends to see symptoms with much milder degenerative changes because the available spinal canal space is already smaller in anterior-posterior diameter and area. Therefore, symptoms in patients with congenital/developmental stenosis tend to occur at a younger age; in the third to fifth decades of life.
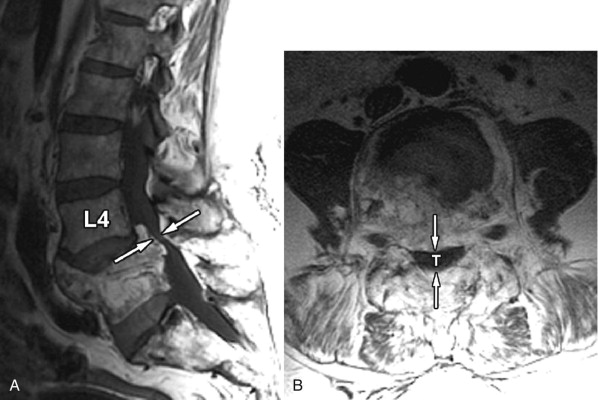
Acquired stenosis is much more common than congenital/developmental stenosis. Degenerative stenosis is the most common type of acquired stenosis. Degenerative arthritis often becomes symptomatic after the fifth decade of life. It is often due to arthritic changes of the intervertebral disc, facet joints, and surrounding ligaments. First, there is loss of disc height with bulging of the disc annulus and thickening/redundancy of the ligamentum flavum. Disc bulging then leads to ventral compression of the thecal sac. The ligamentous redundancy causes posterior/posterolateral compression of the thecal sac. Loss of disc height leads to foraminal compromise. This then leads to osteoarthritis and hypertrophy of the zygapophyseal joints with thickening of the joint capsule. Osteophytes form in order to stabilize the degenerating level, giving it more surface area. Osteophyte formation of the inferior articular processes results in posterolateral compression of the thecal sac. Osteophyte formation from the superior articular processes can result in stenosis of the lateral recesses or foraminal narrowing causing radicular pain. With severe facet joint arthritis, synovial-lined cysts can arise and protrude into the spinal canal, foramen, or lateral recess ( Fig. 72-2 ) .

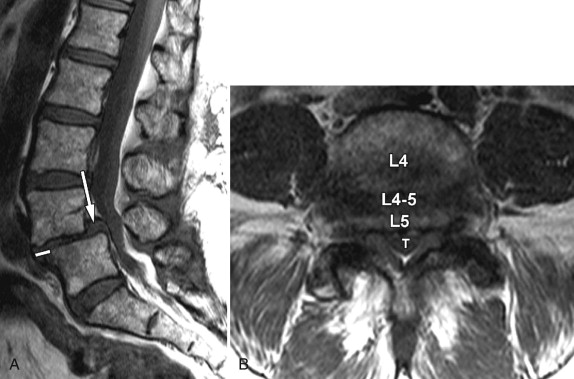
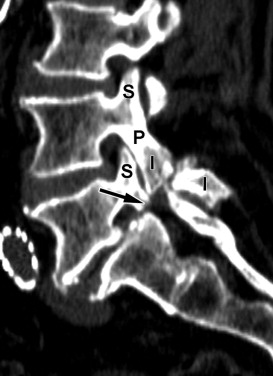
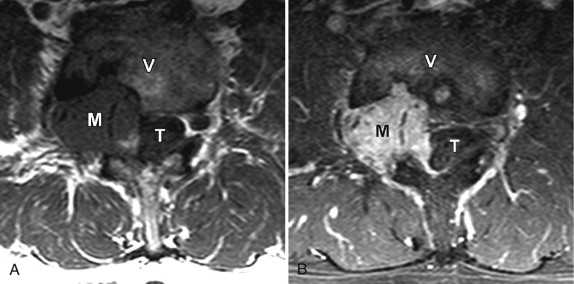
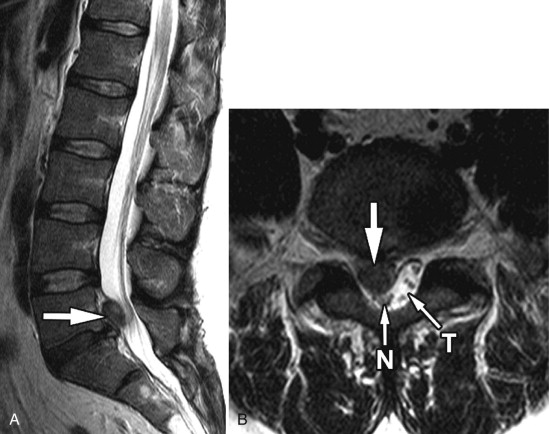
Other causes of acquired spinal stenosis include stenosis related to a degenerative spondylolisthesis ( Fig. 72-3 ) , spondylolisthesis associated with a spondylolysis ( Fig. 72-4 ) or at a level adjacent to a spinal fusion, increased intraspinal fat secondary to endogenous or exogenous steroids ( Fig. 72-5 ) , Paget’s disease ( Fig. 72-6 ) , epidural mass from metastatic disease ( Fig. 72-7 ) and acromegaly. Another very common cause of acquired stenosis is a disc herniation ( Fig. 72-8 ) .
The classic symptoms of lumbar spinal stenosis are those of neurogenic claudication: pain during walking, numbness, tingling, weakness, and pain that radiates from the lower back, frequently into the thighs and lower legs. The symptoms are exacerbated with lumbar extension and improved with lumbar flexion, felt to be secondary to the increase in cross-sectional area of the lumbar spinal canal in flexion. Patients can commonly ride a bike or walk uphill because these movements require being in lumbar flexion, but have difficulty walking downhill because of the required lumbar extension. Radicular symptoms are caused by foraminal or lateral recess stenosis.
Imaging Features
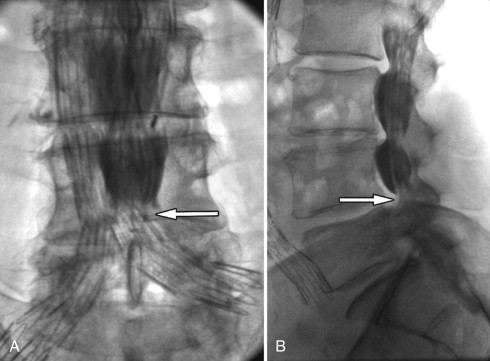
The role of imaging is not only to define whether spinal stenosis is present but also to determine the cause and the relative contribution of bony versus soft tissue spinal stenosis. Plain radiographs are often not useful because although they can demonstrate changes of disc space narrowing and osteophytes, the relative contribution of these abnormalities to spinal stenosis is not evident. Myelography has been used in the past but has been supplanted by less invasive cross-sectional imaging. Myelography indirectly demonstrates spinal stenosis as a narrowing of the contrast-filled thecal sac ( Fig. 72-9 ) . One then needs to deduce whether the narrowing is caused by soft tissue and/or bony causes. Myelography is very insensitive to abnormalities outside of the central canal and does not allow for visualization of abnormalities lateral to the midneural foramen. A combination of myelography and computed tomography (CT) can improve visualization of both the bony detail and nerve root compression ( Fig. 72-10 ) , but is invasive because myelography requires an intrathecal injection of contrast material.