Spine
Case 3.1 Atlanto-Occipital Dislocation
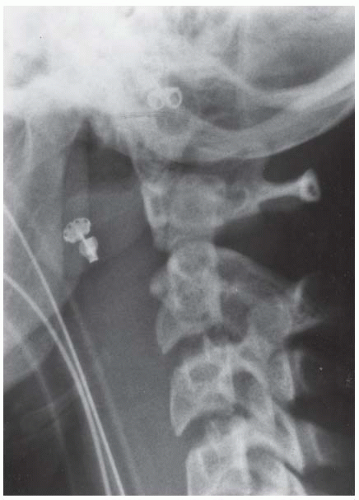
CLINICAL HISTORY An unconscious 13-year-old girl after a motor vehicle accident, and a companion case.
FINDINGS
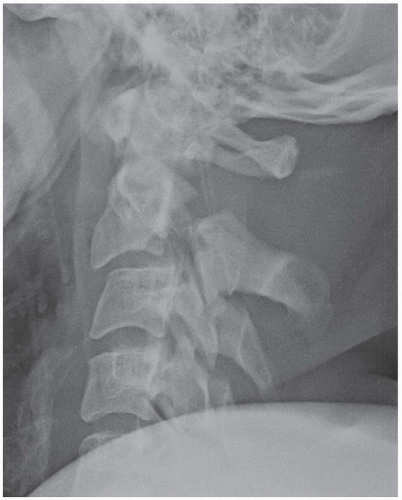
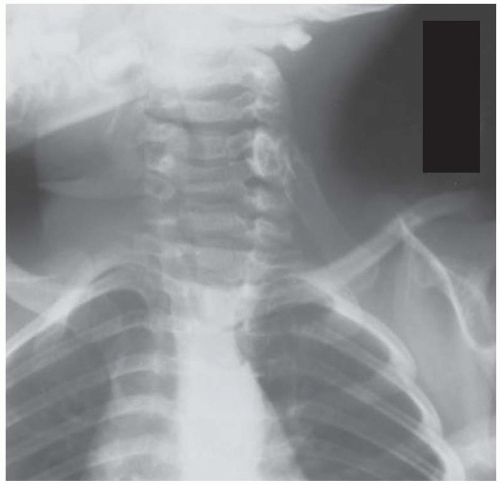
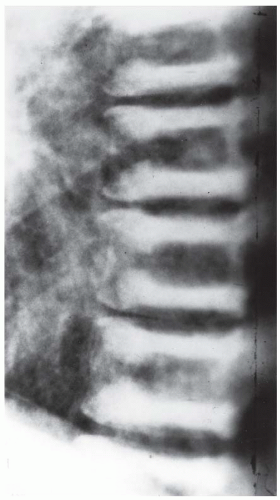
Lateral radiograph of the cervical spine. The prevertebral soft tissues are massively enlarged, even with intubation of the patient. The integrity of the craniocervical junction is difficult to assess, but the upper cervical spine appears intact.
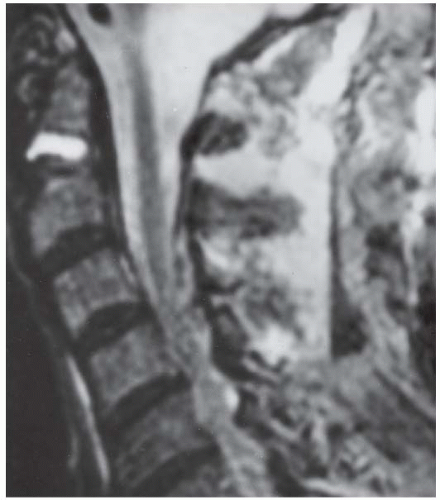
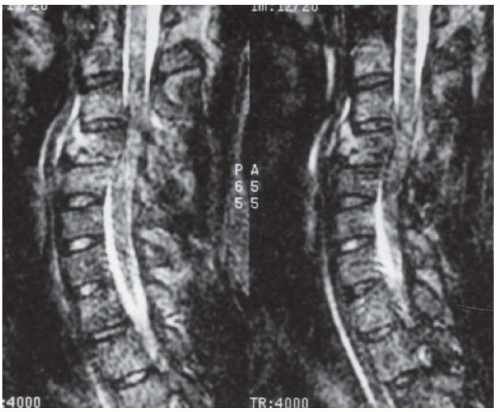
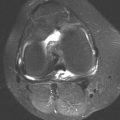
Companion case: A 42-year-old woman ejected from rollover motor vehicle accident. Sagittal T2-weighted magnetic resonance imaging (MRI) through the left atlanto-occipital joint demonstrates marked forward subluxation of the occipital condyle. The appearance of the right atlanto-occipital joint (not shown) is similar.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Atlanto-occipital dislocation.
DISCUSSION The craniocervical junction is evaluated on radiographs with lateral and open mouth views. Soft tissue swelling is an invariable finding in the acute presentation, as seen here. The superior facets of the lateral masses of C1 should articulate with the occipital condyles. Although there are several indirect radiographic methods for assessing the craniocervical junction, they depend on accurately positioned radiographs, which are often difficult to obtain in the acute setting with multiple injuries. When injury is suspected by the mechanism of trauma and the presence of soft tissue swelling, even if the relationship of the occipital condyles to the superior facets of the atlas appears normal on radiographs, direct imaging with cross-sectional methods (computed tomography [CT] or MRI) is still indicated.
Traumatic atlanto-occipital dislocation has generally been considered to be incompatible with life, but many patients have survived this injury [1,2,3,4]. As CT is being used more frequently to screen for cervical spine injuries, less severe forms of atlanto-occipital dislocation are being recognized. Early diagnosis is crucial in order to avoid life-threatening diagnostic manipulations, such as attempts at flexionextension views, and to provide adequate treatment. This is a particular concern in patients with multiple traumas. Unrecognized traumatic atlanto-occipital dislocation may contribute to deterioration and rapid demise of patients who arrive from the scene alert and neurologically intact. Patients who survive these injuries often have severe spinal cord injury, but there are reports of recovery with good neurologic outcome [5]. Cerebral trauma is frequently associated. Treatment is halo immobilization and surgical fusion of the occiput to C1 and C2.
Case 3.2 Hyperflexion Sprain
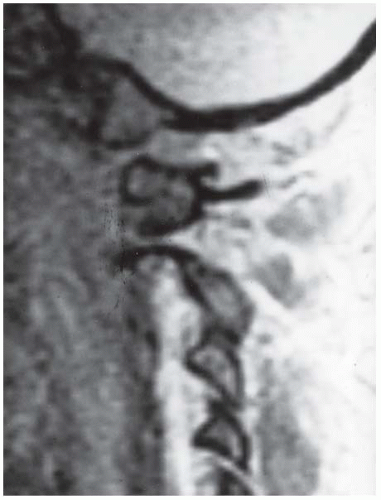
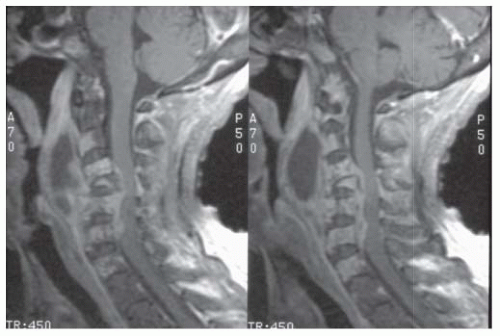
CLINICAL HISTORY An adult female automobile accident victim, acute presentation; companion case, man who fell off roof.
FINDINGS
Lateral radiograph of the cervical spine. There is narrowing of the C5-C6 anterior disc space and widening of the posterior disc space. Marked widening is present between the C5 and C6 spinous processes. Mild prevertebral soft tissue swelling is present. No fracture is identified.
Companion case. Sagittal T2-weighted MRI shows high signal in the posterior soft tissues at the C3-C5 levels indicative of hyperflexion sprain. There is also a fracture of the body of C6.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Hyperflexion sprain.
DISCUSSION When the neck is forcibly flexed, the cervical spine is distracted posteriorly and compressed anteriorly. If the forces are relatively small, the injury may consist of a posterior ligamentous sprain (hyperflexion sprain) and possibly a compression fracture of the vertebral body. The radiographic hallmarks of a hyperflexion injury are a focal kyphosis in conjunction with narrowing of the anterior disc space, widening of the posterior disc space, and splaying of the spinous processes [25]. Hyperflexion sprain results in a tear of the posterior longitudinal ligament complex (including the posterior longitudinal ligament, supraspinous and interspinous ligaments, joint capsule, and ligamentum flavum). This disruption allows anterior subluxation of the vertebral body by 1 to 3 mm in conjunction with mild subluxation of the facet joints. The radiographic findings may be subtle. Straightening of the cervical spine in the acute setting may be secondary to muscular trauma, and a focal kyphosis may ensue at a later time. Fluid-sensitive sequences on MRI may show high signal in the posterior soft tissues, corresponding to tears of the posterior ligaments. Injury may occur at more than one level, as demonstrated in the companion case presented here. If untreated, this type of injury may be associated with delayed instability [26].
Case 3.3 Complex C1-C2 Fractures
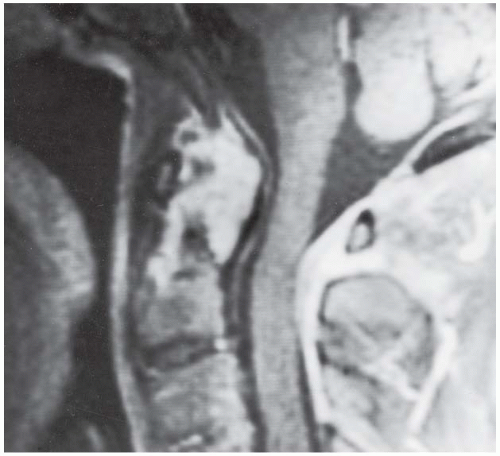
CLINICAL HISTORY A 70-year-old man who fell.
FINDINGS
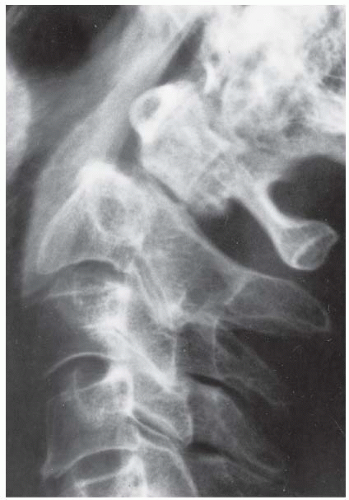
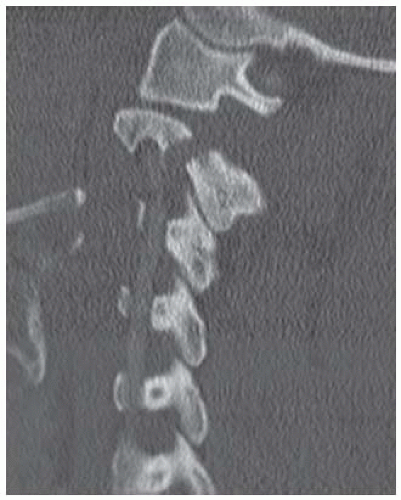
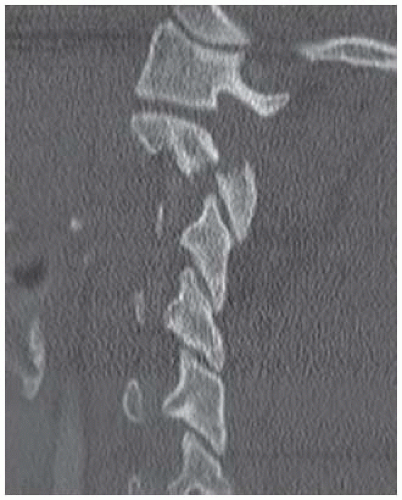
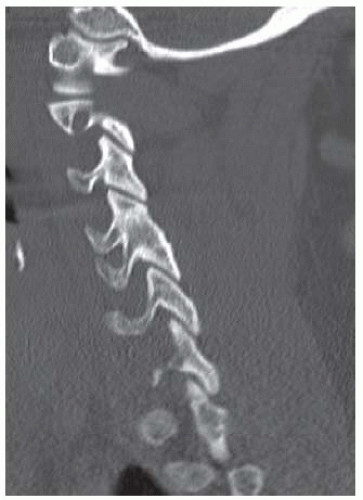
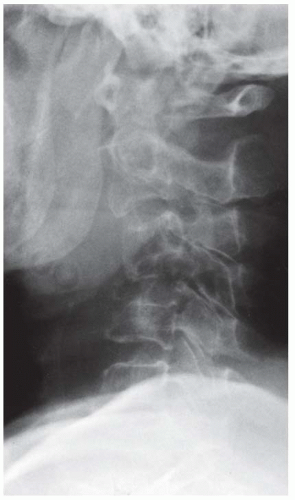
Lateral radiograph of the cervical spine demonstrates widening of the C1 ring. Increased distraction of the C2-C3 disc space is noted, with an accentuated, focal lordosis. There are incidental findings of diffuse idiopathic skeletal hyperostosis (DISH).
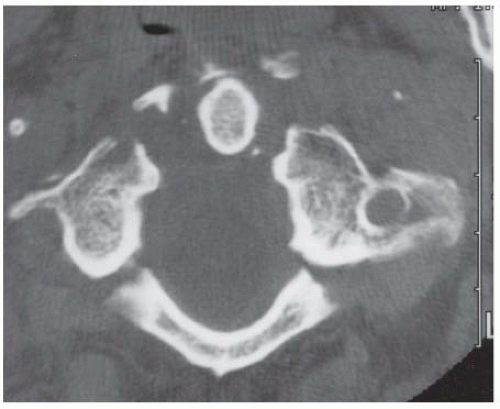
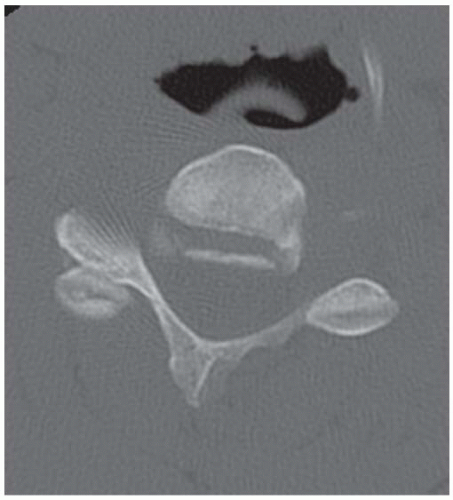
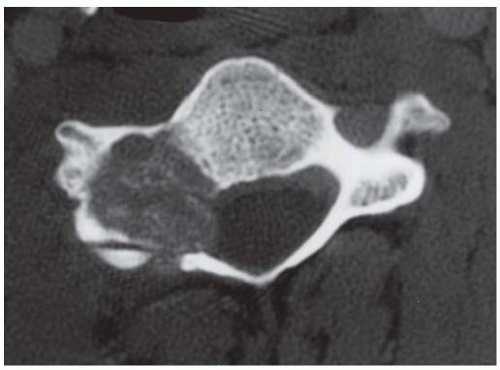
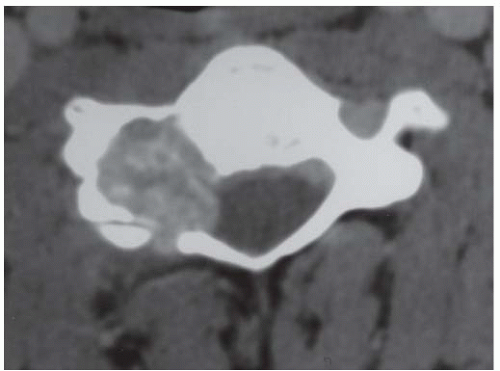
Axial CT demonstrates Jefferson burst fracture at C1.
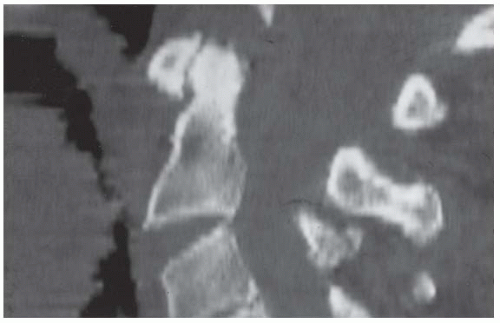
Detail of sagittally reformatted CT image shows the increased distraction and lordosis at C2-C3 and the displacement of the posterior arch of C1.
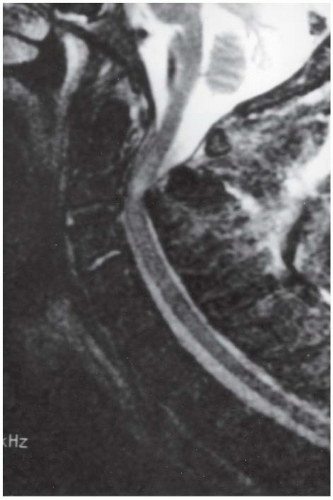
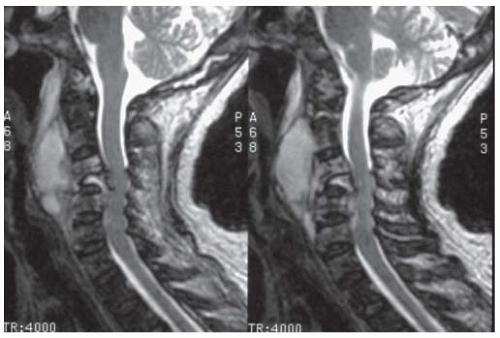
Sagittal T2-weighted MRI at the midline demonstrates mechanical impingement on the posterior aspect of the cervical spinal cord at the C2-C3 level. High signal in the cord itself indicates contusion.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Complex C1-C2 fractures.
DISCUSSION Mimics of a Jefferson fracture include the isolated posterior C1 arch fracture (which can be distinguished by the lack of prevertebral soft tissue swelling) and the congenital fusion failure of posterior C1 arch. These can be differentiated by CT. This case illustrates the importance of careful screening after identifying one injury [6]. Distraction of the C2-C3 disc space is most suggestive of a concurrent hyperextension injury. The classic axial load injury is the Jefferson fracture, which consists of a disruption of the anterior and posterior arches of C1. The fractures can be unilateral or bilateral. The transverse ligament can be intact or disrupted, resulting in widening of the anterior or lateral atlantodental interval. If there is a vertical fracture through one of the articular masses, the medial fragment may maintain its normal relationship with the dens while the lateral fragment migrates laterally. Cervical spine fractures in the elderly are relatively common, comprising 23% of cervical spine fractures in one study [7]. Virtually all fractures in the elderly age group involve the atlantoaxial complex [8], with the most common lesion being a fracture of the odontoid process or a combination of fractures of both C1 and C2, as in this case. The injuries are associated with considerable morbidity and mortality, mostly from coexisting respiratory disease [9]. Treatment with a rigid collar, a halo brace, or surgical stabilization may be successful according to circumstance.
Case 3.4 Nonunion of Odontoid Fracture (Os Odontoideum)
CLINICAL HISTORY A 54-year-old man with chronic neck pain. He was involved in an automobile accident at age 20.
FINDINGS
A, B. Lateral cervical spine flexion-extension series. There is gross instability of C1 over C2 in both flexion and extension, resulting from an ununited odontoid fracture. Sclerotic, remodeled fracture margins with pseudoarthrosis are evidence of the chronicity of the lesion. The margins of the spinal canal at C1 and C2 are malaligned.
C. Sagittal T2-weighted MRI demonstrates a neutral position of the dens at the time of imaging, with T2 hyperintense fluid interposed between the C2 body and the dens. Extensive ligamentous edema is noted in the posterior neck musculature.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Nonunion of odontoid fracture (os odontoideum).
DISCUSSION Fractures of the odontoid process of C2 (dens) occur transversely across the base, probably as a result of hyperextension, hyperflexion, or lateral flexion [10]. The Anderson classification for fractures of the dens is as follows: (type I) superolateral odontoid, avulsed by the intact alar ligament, an exceedingly rare lesion; (type II) base of dens, “high dens fracture;” (type III) superior axis, caudal to the odontoid base, “low dens fracture.”
The odontoid is composed primarily of cortical bone, so this fracture heals less well than fractures through portions of the vertebra that are primarily cancellous. Schatzker et al. [11] report nonunion in 64% of type II fractures, and 100% of those with 5 mm or more of distraction.
An odontoid fracture that has progressed to atrophic nonunion is called an os odontoideum. Like nonunions elsewhere, the margins of the fracture line become corticated; a fibrous union or a pseudoarthrosis may be present. Although some authorities argue that the os odontoideum is a developmental variant in which the odontoid process does not fuse to the body of C2, the site of the synchondrosis between the odontoid process and the body of C2 is not located here. Because of present or potential mechanical instability, surgical fusion of C1 and C2 is the common method of management.
This is a complex case because the sclerotic dens margin suggests chronicity, whereas the posterior soft tissue swelling indicates a superimposed acute injury. The instability of the upper cervical spine leaves the spine vulnerable to catastrophic injury with relatively minor trauma.
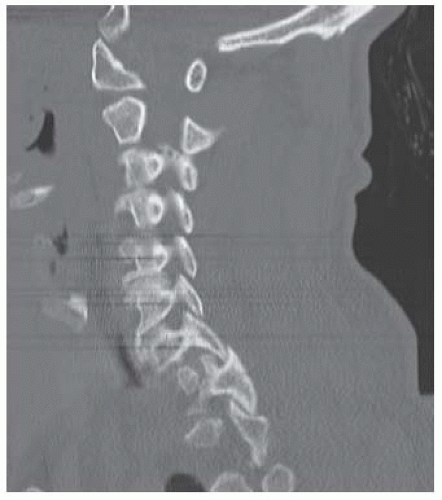
Case 3.5 Traumatic C2 Spondylolisthesis
CLINICAL HISTORY A 23-year-old man who was the front seat passenger in a high-speed automobile crash. There was no neurologic deficit.
FINDINGS
Lateral radiograph of the cervical spine. Horizontal fractures through the bilateral pars interarticularis have allowed the anterior portion of C2 to translate anteriorly. The posterior arch fragment of C2 is displaced posteriorly, resulting in segmental widening of the spinal canal.
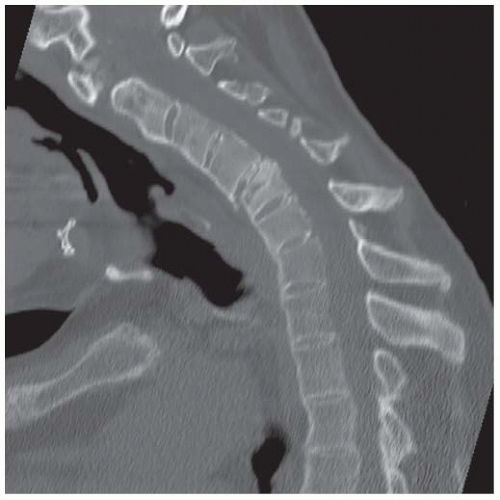
B-D. Sagittal CT reformations of the cervical spine (left to right). There is mild distraction at the fracture sites. The fractures have an oblique coronal morphology from tensile loading. There is approximately 3 mm anterolisthesis of C2 over C3, pulling the left vertebral artery forward. The C2-C3 disc space may be minimally narrowed.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Traumatic C2 spondylolisthesis.
DISCUSSION In traumatic C2 spondylolisthesis (hangman’s fracture), there are bilateral pars interarticularis fractures with forward subluxation of C2 over C3 [12]. The pars interarticularis is the bridge of bone that occupies the position in the articular mass between the superior and inferior articular facets.
An individual subjected to judicial hanging drops feet first through a trap door with a rope secured around the neck and the hangman’s knot located under the chin. When he or she reaches the end of the rope, the upper cervical spine is pulled violently into hyperextension and simultaneously subjected to massive distractive forces from the downward inertia of the body. The ligaments of the anterior column are torn at the C2-C3 level, and the posterior elements are fractured at the pars interarticularis, as C2 is grossly distracted from C3. Similar fractures of the C2 posterior elements may also occur when an axial load (compressive rather than distractive) is applied with the neck hyperextended, but the gross distraction of C2 from C3 does not occur. This mechanism of injury may occur in a motor vehicle accident in which the passenger slides forward and strikes the forehead, forcing the neck into hyperextension.
The Levine and Edwards modification of the Effendi classification for traumatic C2 spondylolisthesis is as follows [13]: (type I) less than 3-mm anterior C2 body translation and no angulation; (type II) greater than 3-mm anterior C2 body translation and angulation; (type IIA) minimal C2 body translation but severe angulation; (type III) severe displacement and severe angulation.
There are associated injuries in 14% of cases, half of which involve the C1 posterior arch or dens. With the exception of the type III variant, the resulting neurologic deficits are often absent or minimal because of the typically capacious spinal canal at the C2 level and the fact that the fragments spread circumferentially. Depending on the severity of the injury, treatment may be conservative or surgical [14].
Case 3.6 Unilateral Facet Dislocation (Unilateral Locked Facet)
CLINICAL HISTORY A 35-year-old woman in an automobile accident.
FINDINGS
Lateral radiograph of the cervical spine. There is 25% forward subluxation of C3 over C4. The interior facet of C3 is dislocated over the superior facet of C4, leaving it partially uncovered. Rotatory displacement is evident by the differences in the radiographic overlap of the facets above and below the level of injury. A focal kyphosis is present, and there is soft tissue swelling.
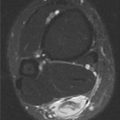
CT (bone windows) at the C3-C4 level shows the right inferior articular process of C3 is anterior to the right superior articular process of C4, but a normal relationship is present on the left.
Sagittal proton density (PD) MRI in the midline shows forward subluxation of C3 over C4 with a widening of the disc space.
MRI on the right shows the C3 facet dislocated over C4.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Unilateral facet dislocation (unilateral locked facet).
DISCUSSION The plain film is diagnostic in this case. C3 is anteriorly subluxated approximately 25% of a vertebral body width in conjunction with minimal distraction of the C3-C4 disc space and a solitary “jumped” facet (the more superior facet is anterior to its articulating inferior facet). These findings are corroborated on CT and MRI. Unilateral facet dislocation occurs with hyperflexion and rotation [15]. Axial rotation and lateral bending are normally coupled in the middle and lower cervical spine because of the angle of the facet joints. With lateral bending, the facet joint on the concave side of the bend is compressed and essentially fixed, and the contralateral articular mass rides forward and up and dislocates into the intervertebral foramen. The superior portion of the inferior facet is frequently fractured, presumably from impaction. The ligaments are disrupted on the side of the dislocation. Unilateral facet dislocation is recognized by forward subluxation of the vertebral body, as shown here, combined with the dislocation of the facet. Sometimes the dislocated inferior facet can be seen projecting into the vertebral foramen (not shown), and the superior facet of the level below is uncovered or “naked” (shown on the plain radiographs). Soft tissue swelling is often present. The fanning of the spinous processes and widening of the disc space are indicative of the hyperflexion component of the injury. The CT can show the clockwise rotation of one vertebral body relative to the level below. In addition, the “reverse hamburger bun” sign can be demonstrated as replacement of the normal, flat, articulating surfaces with the convex surfaces in apposition [16]. CT can also define an associated articular process fracture, seen in up to 73% of cases. MRI would show the associated hemorrhage tracking along the anterior and posterior longitudinal ligaments. MRI can also identify associated soft tissue injuries [17] and serve as a screen to identify intimal injury of the vertebral artery.
Case 3.7 Klippel-Feil Syndrome
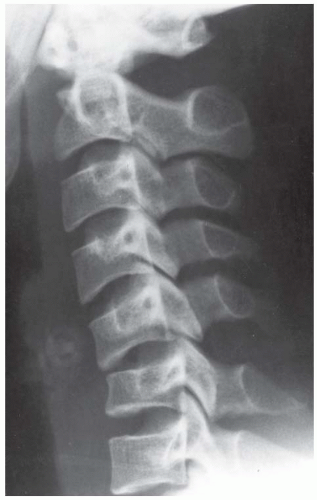
CLINICAL HISTORY A 22-year-old woman in a motor vehicle crash, and a companion case.
FINDINGS
A. Lateral cervical spine. Congenital fusion of C4-C5 is present.
B-D. Sagittal CT reformations of the cervical spine (left to right). The fusion includes the C4 and C5 bodies and posterior elements.
E. Companion case: 2-year-old girl. Anteroposterior (AP) view of the cervical spine shows dysplasia of the cervical vertebral bodies and an omovertebral bone.
DIFFERENTIAL DIAGNOSIS Klippel-Feil syndrome, juvenile chronic arthritis.
DIAGNOSIS Klippel-Feil syndrome.
DISCUSSION Klippel-Feil syndrome is a congenital condition of unknown cause [18]. Most patients present with a short neck and a decreased range of motion in the cervical region. Klippel-Feil syndrome may be associated with many other anomalies (cardiovascular, renal, and limb) and is not clearly genetic; it likely results from an insult to the circulatory system in the 6th week of embryologic development. Common findings are fusion of the cervical spine vertebral bodies and congenital scoliosis. Deformities of the craniocervical junction may cause severe neurologic impairment. Approximately one-third of patients will have an elevated and rotated scapula, known as a Sprengel deformity. An accessory bone extending from the medial border of the scapula to the spine—an omovertebral bone—is also commonly seen [19]. One classification system is based on the levels of fusion: type I, single-level fusion; type II, multiple noncontiguous fused segments; type II, multiple, contiguous fused segments [20].
Case 3.8 Hyperflexion Teardrop Fracture
CLINICAL HISTORY A 27-year-old man with quadriplegia after rescue from an automobile accident, and a companion case.
FINDINGS
Lateral radiograph of the cervical spine. A fracture of the body of C4 is present with anterior soft tissue swelling. The major portion of the C4 vertebra remains in normal alignment, whereas the anteroinferior teardrop fragment is rotated anteriorly. Mild soft tissue swelling is evident by a contour abnormality of the anterior prevertebral soft tissues.
Sagittal T2-weighted MRI at the midline shows the fracture at C4. The spinal canal is narrowed, with impingement on the spinal cord.
Companion case. Lateral radiograph of the cervical spine shows a displaced teardrop fragment of the body of C6, which is also compressed.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Hyperflexion teardrop fracture.
DISCUSSION The hyperflexion teardrop injury is the result of axial compression with hyperflexion caused by large forces, leading to a fracture dislocation [21]. An example of this type of loading might be diving into shallow water with the chin tucked, flexing the neck [22]. Massive posterior distractive forces disrupt the posterior ligament complex and dislocate the facet joints. The anterior and middle columns are disrupted, with tears of the longitudinal ligaments and the intervertebral disc. A triangular fragment (teardrop fragment) is sheared off the anteroinferior corner of the dislocating vertebral body. The result is complete disruption of the cervical spine, with the superior portion displaced posteriorly and angulated anteriorly. The injury is recognized radiographically by focal kyphosis, posterior dislocation, distraction of the posterior elements, and wedging deformity of the vertebral body with teardrop fragment off the anteroinferior corner. The teardrop fragment usually remains aligned with the vertebral column inferior to the level of injury, whereas the remainder of the vertebral body and the vertebral column superior to the injury will be displaced posteriorly. This retrolisthesis may result in widening of the facet joints and disruption of the spinolaminar line. Sagittal fractures of the vertebral body and laminae, caused by the axial loading, are commonly associated. Diffuse, marked, anterior prevertebral soft tissue swelling is always present. The most common site of involvement is C5. The hyperflexion teardrop fracture dislocation is a highly unstable injury, and the spinal cord is always injured. Although paraplegia or quadriplegia can result, the characteristic injury associated with this fracture is the anterior cord syndrome, which consists of complete motor paralysis coupled with a loss of pain, temperature, and touch, but preservation of the posterior column functions of vibration and position.
Case 3.9 Hyperextension Sprain at C5-C6 with Teardrop Fragment (Companion Case, Hyperextension Sprain at C2-C3 with Teardrop Fragment)
CLINICAL HISTORY A 36-year-old man in an automobile accident, and a companion case.
FINDINGS
Lateral radiograph of the cervical spine. Anterior soft tissue swelling is present. At the C5-C6 level, the intervertebral disc space is widened anteriorly and narrowed posteriorly. There is retrolisthesis of C5 relative to C6. A small fragment of the C5 body remains aligned with the anterior aspect of C6.
Sagittal CT reformation shows the misalignment of C5 over C6.
Companion case. Lateral radiograph of the cervical spine shows anterior soft tissue swelling and a nondisplaced fracture of the anteroinferior corner of the body of C2. Alignment is normal.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Hyperextension sprain at C5-C6 with teardrop fragment (companion case, hyperextension sprain at C2-C3 with teardrop fragment).
DISCUSSION Widening of the anterior disc space and narrowing of the posterior disc space is the hallmark for a hyperextension injury. Axial loading with hyperextension places the anterior column under tension, and the posterior column under compression [23]. Structures of the spine fail in sequence, depending on the magnitude of the loading: tear of the anterior longitudinal ligament, disruption of the intervertebral disc, and tear of the posterior longitudinal ligament. A tension fracture of the anterior inferior corner of the vertebral body may occur instead of disc disruption, as in this case. If present, the triangular fracture fragment may be called a teardrop fragment, and the injury may be called a hyperextension teardrop fracture, but the significance of this fragment is the accompanying ligamentous injury. The anteroinferior avulsion may remain undisplaced, or may be rotated anteriorly from the vertebral body on an intact hinge of anterior longitudinal ligament. If the spine reduces after the injury, the teardrop fragment may be the best radiographic clue to the presence of the more serious injury. Compression fractures of the posterior elements are common, including fractures of the lamina and lateral masses. One or both facet joints may become dislocated. If only ligaments are disrupted and the spine relocates on the rebound, radiographs may show a normally aligned spine without fracture in an acutely quadriplegic patient. Marked prespinal soft tissue swelling should be present.
This injury is most commonly seen in older patients with osteopenia or cervical spondylosis [24]. The prevertebral soft tissue swelling can be minimal in older patients.
Case 3.10 Ankylosing Spondylitis, with Fracture
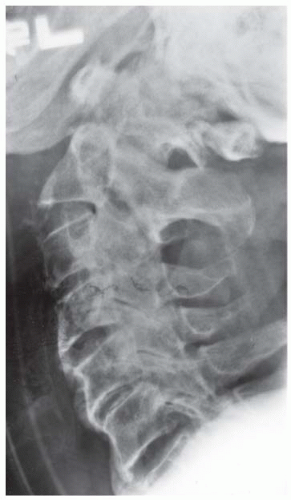
CLINICAL HISTORY A 57-year-old man with a stiff, painful neck.
FINDINGS
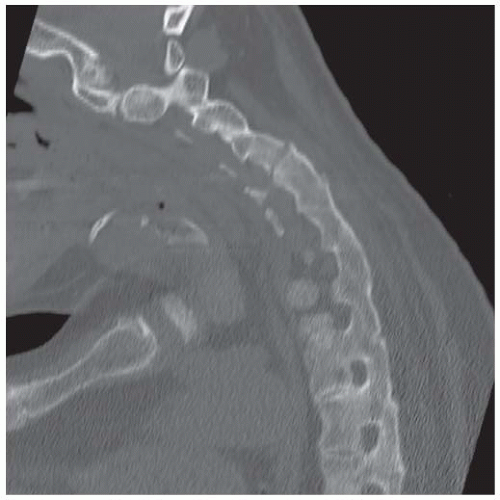
A. Lateral radiograph of the cervical spine shows severe cervical kyphosis, but vertebral heights are normal. There is ankylosis of the facet joints and intervertebral disc joints, and the anterior corners of the vertebral bodies are squared off. The bones are osteoporotic. In addition, there is a minimally displaced fracture that extends through the entire vertebral column at the C4-C5 level.
B, C. Sagittal reformatted images from CT show the fracture plane extending through the upper portion of the body of C5 and then through the fused posterior elements of C4 and C5.
DIFFERENTIAL DIAGNOSIS Ankylosing spondylitis, juvenile idiopathic arthritis, DISH.
DIAGNOSIS Ankylosing spondylitis, with fracture.
DISCUSSION The combination of ankyloses of the facet joints and syndesmophytes is diagnostic of this disorder. The delicacy of the syndesmophytes and the presence of osteopenia are key differential features relative to DISH. Preservation of vertebral body height and intervertebral disc spaces are key differential features relative to juvenile idiopathic arthritis. Syndesmophyte formation in ankylosing spondylitis is the result of inflammation that leads to ossification of the outer layers of the annulus fibrosis. The resulting bridges of bone that fuse the adjacent vertebral bodies should not extend beyond the endplates. Ankylosing spondylitis affects the synovial articulations, cartilaginous articulations, and entheses. In synovial joints, the inflammatory process is a synovitis that is pathologically similar to rheumatoid arthritis, but less intense. Inflammatory fibroplasia of synovium can transform into chondroid metaplasia that then ossifies, resulting in ankylosis; this is a major feature of this disease, unlike rheumatoid arthritis.
Similar pathologic abnormalities occur in cartilaginous articulations. Swollen fìbrocytes in the outer annulus fibrosis layers at the attachment of Sharpey’s fibers undergo chondroid metaplasia and ossify, resulting in the smooth, flowing appearance of syndesmophyte formation. Pain diminishes or disappears as the spine fuses, but the fused spine becomes osteoporotic and fragile and is subject to insufficiency fractures. Fusion usually begins at the lumbosacral junction and extends superiorly. The ankylosed spine is much more vulnerable to traumatic injuries than the normal spine; furthermore, these patients are at high risk for complications and death [27].
Case 3.11 Osteoblastoma
CLINICAL HISTORY A 25-year-old man with back pain in the upper cervical region for several months.
FINDINGS (A, B) CT (bone and soft tissue windows). CT shows an expansile lesion in the right lateral mass of a cervical vertebra (C4), extending into the spinal canal, transverse foramen, and vertebral body. Focal destruction of the cortex is present. The lesion is well circumscribed, but does not have reactive margin of bone. The lesion is mineralized.
DIFFERENTIAL DIAGNOSIS Osteoblastoma, aneurysmal bone cyst, osteosarcoma, brown tumor, fibrous dysplasia.
DIAGNOSIS Osteoblastoma.
DISCUSSION Differential considerations in this case include osteoid osteoma (if the lesion were less than 2 cm), osteosarcoma (if the lesion had a more aggressive appearance or associated soft tissue mass), aneurysmal bone cyst (which can be seen in conjunction with an osteoblastoma; therefore, the pathologist ultimately distinguishes between the two), giant cell tumor (if the lesion were less well defined), and a brown tumor (if the patient had other clinical evidence for hyperparathyroidism).
Osteoblastomas are uncommon lesions considered by some to be giant osteoid osteomas because of their histologic resemblance [28]. They affect young people—80% occur in patients younger than 30 years old—and there is a male predominance. About half are located in the spine and most of the remainder in the femur and tibia; 9% are located in the cervical spine [29,30]. Of those in the spine, most are in the posterior elements, but a few also involve the vertebral body, and very few involve the vertebral body alone.
The radiographic appearance is a partially lucent expansile lesion, with well-defined thin sclerotic margins and a variable amount of matrix mineralization. The lucent area of geographic bone destruction corresponds to replacement of bone by nonmineralized tumor tissue. The tumor osteoid may have densely solid or ground-glass mineralization. Large lesions may have an expanded cortical shell from slow endosteal cortical erosion, balanced against an enlarging layer of periosteal new bone. Cortical penetration into the soft tissues is absent, but tomography may be required to demonstrate the cortical shell. The tumor tissue may have high attenuation on CT from the diffuse mineralization. Osteoblastomas are hot on bone scan. They usually grow slowly and respond well to excision; radiation is useful when the lesion is difficult to excise. Very few have been reported to become locally aggressive. In the cervical spine, lesions in close proximity to the vertebral artery require complex therapeutic solutions [31].
Case 3.12 Tuberculous Spondylitis
CLINICAL HISTORY A 53-year-old man with neck pain for several weeks.
FINDINGS
Lateral radiograph of the cervical spine through a cervical collar. The C4 vertebral body has dissolved, and the C3-C4 and C4-C5 disc spaces are narrowed. Marked prevertebral soft tissue swelling is identified.
Sagittal T2-weighted MRI shows partial collapse of C4 and C5, with prevertebral fluid collection and posterior mass effect on the spinal cord. The abnormality extends along several levels.
Sagittal T1-weighted MRI after gadolinium shows enhancement involving most of the cervical spine, with no enhancement of the prevertebral collection.
DIFFERENTIAL DIAGNOSIS Pyogenic diskitis, tuberculous spondylitis, metastasis, lymphoma, massive vertebral osteolysis (Gorham disease), trauma.
DIAGNOSIS Tuberculous spondylitis.
DISCUSSION At first glance, one might suspect osteolytic destruction secondary to tumor or Gorham disease, but the large prevertebral fluid collection would be expected only with infection. Pyogenic infections typically arise in the disc space and provoke reactive bone formation, whereas tuberculosis tends to provoke little, if any, reactive bone formation. The large retropharyngeal abscess and the multilevel involvement would also be very unusual in pyogenic diskitis. Although tuberculosis is becoming more common in North America, involvement of the cervical spine remains rare, comprising only 3% to 5% of cases of tuberculosis of the spine. Patients present with neck pain and may have a kyphotic deformity. In children, the disease is frequently extensive, with paraspinal abscess formation [32], while in adults it is more commonly localized to one or two segments. Cord compression is common, and patients may develop reversible quadriparesis as a result [33]. The treatment of tuberculous spondylitis in the cervical spine is similar to treatment of tuberculosis elsewhere in the spine, and consists of antituberculous chemotherapy and, when necessary, surgical resection of abscesses and mechanical stabilization.
Case 3.13 Rheumatoid Arthritis
CLINICAL HISTORY A 43-year-old woman with polyarticular arthritis, and a companion case.
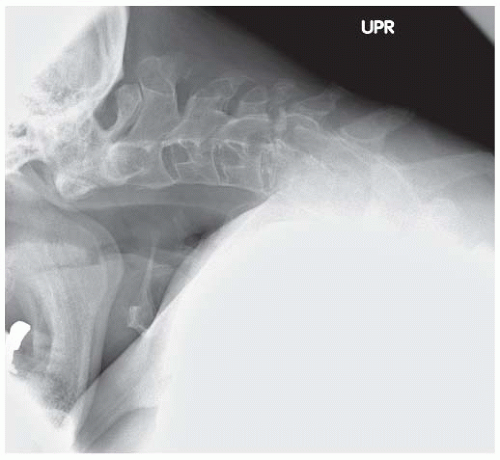
FINDINGS
Lateral cervical spine (neutral position). The atlantoaxial distance is difficult to assess since there is marked irregularity of the odontoid. Generalized osteoporosis is present. The visualized facets are fused.
Sagittal T1-weighted MRI with gadolinium demonstrates marked erosion of the odontoid, with an effective increase in the atlantoaxial distance. Marked enhancement of pannus is identified.
Companion case. Lateral cervical spine. There is axial migration of the C2 vertebral body with absence of the dens. Subluxation is most prominent at C5-C6. Whittling of the C3, C4, and C5 spinous processes is noted. Disc space narrowing with associated endplate is present at C6-C7, but also at the uncommon C3-C4 level.
DIFFERENTIAL DIAGNOSIS Rheumatoid arthritis, ankylosing spondylitis, juvenile idiopathic arthritis.
DIAG NOSIS Rheumatoid arthritis.
DISCUSSION In the cervical spine, multilevel subluxation, osteopenia, and erosions at sites of ligamentous attachments without evidence for reparative bone is characteristic of rheumatoid arthritis. Erosion of the odontoid and instability of the atlantoaxial articulation is a classic presentation for rheumatoid arthritis. Other etiologies for these two findings might include congenital hypoplasia of the odontoid with ligamentous instability, amyloid, or perhaps an atypical infection. Atlantoaxial subluxation is the dominant and the first cervical spine finding, and may occur without radiographic evidence for erosions [34]. A measurement of greater than 2.5 mm between the inferior aspect of the posterior C1 arch and anterior dens is diagnostic. It typically results from disruption of the transverse ligament by pannus formation, as demonstrated here by MRI. Axial migration of the C2 vertebral body is not uncommon as the odontoid dissolves and a potential space is created.
In the lower cervical spine, subluxations are most prominent at the C3-C4 and C4-C5 levels. Anterior subluxation is most common, and the levels of involvement are commonly discontinuous. Apophyseal joint space narrowing and erosions can lead to instability or fibrous union. Discovertebral narrowing, erosion, and late subchondral sclerosis without osteophyte formation can be seen. Whittling of the spinous processes at the insertion of the supraspinous ligaments may be identified. Generalized osteoporosis may be secondary to the disease process or the use of steroids. Compared with other patients with rheumatoid arthritis, those with cervical involvement tend to have a positive rheumatoid factor, higher C-reactive protein level, and progression of peripheral joint disease.
Case 3.14 Juvenile Idiopathic Arthritis
CLINICAL HISTORY A 42-year-old woman with polyarticular disease.
FINDINGS Lateral radiograph of the cervical spine demonstrates fusion of the C3, C4, and C5 facets, with hypoplasia of the respective vertebral bodies and calcification of the intervertebral discs.
DIFFERENTIAL DIAGNOSIS Ankylosing spondylitis, juvenile chronic arthritis, DISH.
DIAGNOSIS Juvenile idiopathic arthritis.
DISCUSSION Diffuse ankylosis of the facet joints in the cervical spine is associated with two conditions: ankylosing spondylitis and juvenile idiopathic arthritis. Distinguishing between the two on radiographs is often possible because ankylosing spondylitis is a disease that involves the mature skeleton, whereas juvenile idiopathic arthritis, by definition, involves the immature, growing skeleton. In the latter, stigmata of the disease process itself and of the effects of the disease on skeletal development should be evident. Thus, diffuse ankylosis of the facet joints in combination with hypoplasia of the vertebral bodies and intervertebral discs is virtually diagnostic for juvenile idiopathic arthritis. In ankylosing spondylitis, the vertebral body and intervertebral disc heights remain normal, even in the presence of ankylosis of the facet joints and syndesmophyte formation, because the spine has already developed fully at the time the disease process affects it.
The cervical spine is more commonly involved with juvenile idiopathic arthritis than other spinal levels [35]. The most common finding is that of atlantoaxial instability; however, other considerations for this finding in a child would include Down’s syndrome, odontoid hypoplasia, and Grisel’s syndrome (infectious laxity as an extension of a peripharyngeal process).
The apophyseal joint fusion is most common at the C2-C3 and C3-C4 levels, as seen in this case. Because this occurs before full growth potential, the constellation of ankylosis and vertebral body and disc hypoplasia is diagnostic.
Other etiologies of apophyseal joint fusion can be excluded by their secondary findings. In addition, enthesopathy and tarsal disease within the first year of presentation is diagnostic of juvenile ankylosing spondylitis, with or without the presence of axial disease. Klippel-Feil syndrome (congenital fusion anomaly) may be difficult to distinguish unless posterior element fusion is a dominant feature. Fibrodysplasia ossificans progressiva should have an element of soft tissue ossification.
Case 3.15 Bilateral Facet Dislocation (Bilateral Locked Facets)
CLINICAL HISTORY A 44-year-old automobile accident victim.
FINDINGS A-C. Sagittal CT reformations of the cervical spine (left to right). There has been previous anterior cervical discectomy and fusion, with anterior plate and screws fixing the C4 through C7 vertebral bodies. There is bilateral interfacetal dislocation at C7-T1, with approximately 50% of the body of C7 displaced anteriorly relative to T1. The inferior facets of C7 are dislocated anteriorly over the superior facets of T1. The superior articular facets of T1 are uncovered by the inferior articular facets of C7 (naked facet sign). There is a displaced avulsion fracture of the anterior superior corner of T1. There is a displaced fracture of the spinous process of C7. There is no rotatory displacement.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Bilateral facet dislocation (bilateral locked facets).
DISCUSSION The major injury vector in bilateral facet dislocation is hyperflexion of large magnitude without axial compression [36]. Bilateral facet dislocation is a tension injury that propagates from posterior to anterior. Complete disruption of the ligaments and forward displacement of one involved vertebra over another allows the inferior articular facets of the superjacent vertebra to dislocate into the intervertebral foramen. In addition to disruption of the posterior longitudinal complex, seen in unilateral facet dislocation, the disc and anterior longitudinal ligament are disrupted, allowing the superior vertebra to be subluxated anteriorly by about 50% of the width of its body. When the facets are subluxated (perched) but not completely dislocated (“partial dislocation”), the anterior subluxation is greater than the 3 mm seen in a flexion sprain, but less than the 50% seen in the complete dislocation. There may be accompanying fractures of the articular processes of the subjacent vertebra. The spine is unstable, and there is a high association with cord contusion, of variable severity. MRI is better than CT for demonstrating possible cord injury and other soft tissue abnormalities [37]. Traumatic injuries to a previously surgically fused spine usually occur at a level adjacent to the fusion [38], presumably due to the concentration of stress by the lever arm formed by the fused segments [39]. Fracture through the fused segment itself appears to be a rare event [40].
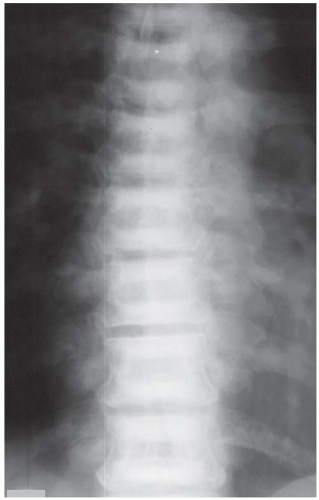
Case 3.16 Morquio Syndrome
CLINICAL HISTORY A 13-year-old boy with short stature.
FINDINGS
Lateral radiograph of the cervical spine. There is flattening of the visualized cervical vertebral bodies and hypoplasia of the odontoid process.
Lateral radiograph of the thoracic spine. There is hypoplasia of the T11 vertebral body with a central beak deformity.
DIFFERENTIAL DIAGNOSIS Mucopolysaccharidoses (dysostosis multiplex), spondyloepiphyseal dysplasia.
DIAGNOSIS Morquio syndrome.
DISCUSSION Morquio syndrome, or mucopolysaccharidosis IV A, is an autosomal recessive deficiency of the enzyme N-acetylgalactosamine-6-sulfatase and has a frequency of 1 in 100,000 births [41]. The key radiologic feature in this case is flattening of the cervical vertebral bodies at every level (universal platyspondyly). In addition, the findings of hypoplastic odontoid with secondary atlantoaxial instability are common in this condition. Although it would be unrealistic for a radiologist to make a specific biochemical and genetic diagnosis from these radiographs, one should recognize that a systemic, congenital disease is present. Morquio syndrome is one of the mucopolysaccharidoses, or diseases caused by inborn errors of complex carbohydrate metabolism. The skeletal features of all these conditions have been collectively called dysostosis multiplex, and are the manifestation of storage of abnormal complex carbohydrate substances that cannot be metabolized further because of enzyme deficiencies. The mucopolysaccharidoses share the findings of macrocephaly; “canoe paddle-shaped” ribs; focal kyphosis with distinctive centrally beaked, diminutive retrolisthesed L1 or L2 vertebral body; flared pelvis; and shortened, broadened long bones [42]. In Morquio syndrome, the platyspondyly tends to be more widespread and marked than in the other mucopolysaccharidoses, which is a possible clue to the specific diagnosis.
Case 3.17 Osteopetrosis
CLINICAL HISTORY An asymptomatic 11-year-old boy.
FINDINGS (A) AP and (B) lateral radiograph of the thoracic spine shows that the vertebral bodies have a uniform “sandwich” appearance, with sharply demarcated sclerosis abutting the endplates. The vertebral body heights and alignment are normal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree