Musculoskeletal structure
Acute injuries
Overuse injuries
Bone
Fracture
Stress reaction/fracture
Contusion
Osteitis/periostitis
Apophysitis
Cartilage
(Osteo)chondral lesion
Chondropathy
Fibrocartilaginous lesions
Osteoarthritis
Joint
Subluxation
Synovitis/capsulitis
Dislocation
Impingement
Ligament
Sprain/tear
Inflammation
Muscle
Strain/tear
Chronic compartment syndrome
Contusion
Focal tissue thickening/fibrosis
Myositis ossificans
Delayed-onset muscle soreness (DOMS)
Exercise-associated muscle cramp (EAMC)
Tendon
Tear (partial/complete)
Tendinopathy
Bursa
Traumatic bursitis
Bursitis
Nerve
Neuropraxia
Entrapment
4.2 Acute Injuries
Acute injuries occur suddenly and have a clearly defined cause or onset. An acute heavy load that exceeds the threshold of tissue tolerability suddenly irreversibly deforms the tissue (e.g., fracture, rupture). Acute injuries most commonly occur in sports characterized by high speed, high risk of falling, and contact sports (Bahr and Mæhlum 2004).
4.2.1 Bone
4.2.1.1 Fracture
Acute fractures are caused by acute traumata that exceed the bone’s tolerance. Fractures can occur due to direct trauma such as a kick to the leg or can result from an indirect trauma such as twisting of the lower leg. Avulsion fractures can occur at the site of tendon or ligament insertion, when a piece of bone attached to a tendon or ligament is torn away. In children and adolescent athletes, two particular fractures occur: (1) “greenstick fractures,” in which the bone is bent like a soft twig, and (2) growth plate fractures that require special attention.
The clinical features of a fracture are pain, tenderness, localized bruising, swelling, and, in some cases, malalignment, shortening of an extremity, and restriction of or unnatural movement. Fractures may be closed or open (compound), where the bony fragment punctures the skin. Radiographs are usually made to confirm the diagnosis and for reason of classification of the type of fracture (transverse, oblique, spiral, or comminuted) (McRae and Esser 2008).
Fractures are managed by anatomical and functional realignment. Non-displaced or minimally displaced fractures can be treated with bracing or casting. Displaced fractures require reduction and immobilization. A displaced, unstable fracture requires surgical stabilization. Delayed union or malunion of a fracture causes persistent pain and disability that may require bone grafting, with or without internal fixation.
Soft tissue injury, such as ligament or muscle damage, is often associated with a fracture and may cause more long-term problems than the fracture itself. Thus it is important to address the soft tissue components of any bony injury.
Occasionally a fracture may cause swelling of a muscle compartment that is surrounded by a non-distensible fascial sheath, usually in the flexor compartment of the forearm or the anterior compartment of the lower leg. This condition—acute muscle compartment syndrome—causes pain out of proportion to the fracture, pain on passive stretch, pulselessness, and paresthesia (Shadgan et al. 2010). This may require urgent fasciotomy. Other complications of fractures that require urgent action are infections, associated nerve or vessel lesions, and deep venous thrombosis/pulmonary embolism.
Particularly in athletes, one should realize that complete immobilization causes problems like deconditioning, muscle wasting, and joint stiffness, which are disadvantageous for the rehabilitation process. Muscle stimulation techniques, functional bracing, and internal fixation of fractures might be helpful to facilitate rehabilitation and to prevent these unwanted side effects in order to achieve quick return to play.
4.2.1.2 Contusion
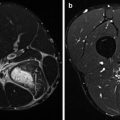
A direct blow from a kick, stick, or ball to, for example, the tibia or iliac crest (hip pointer) can cause a contusion of the bone, which can be extremely painful due to periosteal injury (Hall and Anderson 2013); bone contusion produces microfractures with water signal (bone marrow edema) on T2 or intermediate TE MRI.
4.2.2 Cartilage
The articular surface of most joints is covered by hyaline cartilage that is 1–5 mm thick.
It provides a low-friction gliding surface, acts as a shock absorber, and reduces peak pressures on the underlying bone. Due to increased participation in recreational and competitive sports, articular cartilage injuries are far more common than was previously realized (Flanigan et al. 2010). The articular cartilage can be injured through acute contusion or by shear forces applied to the joint, which frequently occur in relation to acute joint trauma, subluxation, and dislocation. Localized cartilage injuries are diagnosed in 20 % of patients with a rupture of the anterior cruciate ligament of the knee and in over 60 % of patients sustaining a lateral ligament injury of the ankle (Buckwalter 2002). Common sites of chondral and osteochondral injuries are the superior articular surface of the talus, the femoral condyles, the patella, and the capitellum of the humerus. When an apparently “simple joint sprain” remains painful and swollen for longer than expected, an osteochondral lesion must be suspected. Since a radiograph often shows no abnormalities in the acute phase, these injuries should be investigated with MRI. Arthroscopy may be required to assess the degree of damage and to remove loose fragments or to perform an intervention. Using MRI and/or arthroscopy, it is now possible to classify articular cartilage injuries based on size, depth, and surface (Bhosale and Richardson 2008):
1.
Disruption of the articular cartilage at its deeper layers with or without subchondral bone damage, while the articular surface itself remains intact
2.
Disruption of the articular surface only
3.
Disruption of both articular cartilage and subchondral bone
Due to lack of blood supply and low number of cells, articular cartilage has a limited intrinsic capacity to repair itself after an injury, which results in an increased risk that premature osteoarthritis will develop. The larger the lesion or defect, the lower is the probability of healing.
Prognosis is also related to the depth the injury extends toward the underlying bone. Factors affecting return to sport include age, duration of symptoms, number of previous injuries, associated injuries, lesion type, size, and location (Mithoefer et al. 2012).
Fibrocartilaginous structures like the menisci in the knee and the glenoid labrum are also frequently acutely injured. In the specific chapters on knee and shoulder injuries, this pathology will be discussed in more detail. The potential for repair in these lesions also varies with the blood supply. For example, the meniscus of the knee can be divided in a peripheral “red zone” with good blood supply and a central “white zone” with limited blood supply. Especially in younger patients, arthroscopic repair of meniscal lesions in the red zone may be successful (Laible et al. 2013).
4.2.3 Joint
4.2.3.1 Dislocation/Subluxation
The intrinsic stability of a joint depends on its anatomy (bone, cartilage, capsule, ligaments). The active stability is determined by the strength and coordination of the surrounding muscles. Traumatic injury to joint and supporting structures (capsule and ligaments) often results in an episode of instability referred to as dislocation or subluxation.
A dislocation is a complete displacement of joint surfaces so that they no longer make normal contact at all. A subluxation is a partial displacement of joint surfaces in which the articulating surfaces remain partially in contact with each other and is usually transient in nature. It is important to distinguish first time or recurrent dislocations/subluxations.
Joints with less intrinsic stability such as the shoulder and fingers are more likely to dislocate. More stable joints, such as the hip, elbow, and ankle, require much greater forces to dislocate. A dislocation or subluxation implies damage to the supporting structures of the joint like the surrounding joint capsule and ligaments. Complications of dislocations include associated vascular damage (e.g., brachial artery damage in elbow dislocations) and nerve damage (e.g., axillary nerve injury in shoulder dislocations). Radiographs of all dislocated joints should be made to exclude an associated fracture. Dislocated joints, in most cases, can be reduced relatively easily. After reduction, the joint needs to be protected to allow the joint capsule and ligaments to heal. Afterward exercise therapy (strength and coordination training) should be encouraged to increase active joint stability.
4.2.4 Ligament
Ligaments are made up of closely packed collagen fibers that connect one bone to another and provide passive joint stability. They also have an important proprioceptive function. Ligaments may be intra-articular (e.g., the cruciate ligaments), capsular (as a thickening of the joint capsule, e.g., the anterior talofibular ligament), or extracapsular (e.g., calcaneofibular ligament). Healing tendency of capsular ligaments is better because of their better blood supply (Frank 2004).
Injuries occur when a ligament is under excessive load. Typically there is a sudden overload, stretching the ligament, while the joint is in an extreme position. The most common example is traumatic ankle inversion, which causes the lateral ligaments—primarily the anterior talofibular ligament—to rupture. Partial or total tears may occur in the midsection of the ligament or at the ligament-bone junction. Avulsion fractures (a piece of bone pulled away by the ligament) also occur, more commonly in children.
Ligament injuries range from mild injuries involving the tearing of only a few fibers to complete tears of the ligament, which may lead to instability of the joint (Woo et al. 2006). Ligament injuries are divided into three grades (Table 4.2).
Table 4.2
Classification of ligament injuries
Severity | Injury | Signs and symptoms | Stress testing of the ligament |
|---|---|---|---|
Grade 1, mild | Sprain | Slight local tenderness | Normal range of motion |
Grade 2, moderate | Partial tear | Swelling | Increased laxity but definite end point |
Notable tenderness | |||
Grade 3, severe | Complete tear | Swelling | Instability, no end point |
Painful or pain-freea |
Ligament injuries can be visualized using ultrasound and MRI. Management of acute ligament injuries consists of the RICE principle (rest, ice, compression, and elevation) in the acute phase to minimize bleeding and swelling. For grade I and grade II sprains, treatment aims to promote tissue healing, prevent joint stiffness, protect against further damage, and strengthen muscle to provide additional joint stability. The healing of collagen in a partial ligament tear takes 6 weeks to 12 months. Pain subsides but many athletes continue to have objective mechanical laxity and subjective joint instability. Therefore, protection of the joint using a brace or tape for external support should be considered on return to sport in order to prevent reinjury. The treatment of severe grade 3 ligament injuries may be either conservative or surgical.
4.2.5 Muscle
Muscle injuries are common in athletes. The frequency of muscle injuries ranges from 10 to 55 % of all sustained sporting injuries (Delos et al. 2013). Muscle injuries can occur in two ways: (1) by distension leading to strains/tears and (2) by a direct blow leading to a contusion of the muscle.
4.2.5.1 Strain/Tear
Muscles that are commonly affected are the hamstrings, quadriceps, hip adductors, and gastrocnemius. Muscles are strained or torn when the load exceeds what some or all of the fibers can tolerate. A muscle is most likely to tear during a bout of maximal eccentric contraction (involving muscle contraction while muscle is lengthening). The athlete experiences acute pain during his action and sometimes feels a bump in the muscle directly after the injury moment. Pain reproduced with muscle contraction, swelling, and loss of strength are the clinical features which ensue. Muscle strains/tears can be classified into three grades (Table 4.3).
Table 4.3
Classification of muscle strain injuries
Severity | Injury | Signs and symptoms | Strength |
|---|---|---|---|
Grade 1 | Strain of small number of muscle fibers | Localized pain | No loss of strength |
Grade 2 | Tear of significant number of muscle fibers | Pain and swelling | Loss of strength |
Pain with contraction | Movement limited by pain | ||
Grade 3 | Complete tear of the muscle | Pain and swelling | Severe loss of strength |
Pain with contraction | Movement limited by pain |
MRI scans and ultrasound can be helpful in the elite athlete but should not replace important clinical assessment. In the specific chapter on muscle injuries, the classification model, predisposing factors, mechanisms of injury, and healing process of muscle strains/tears are described in more detail. Patients with grade 1 or 2 strains characteristically develop pain during active muscle resisted contraction. They do not present with rest pain.
After a significant muscle injury, there often is little muscle tissue regeneration. The injured muscle tissue is replaced by noncontractile scar tissue, which is more prone to re-rupture. Early return to sporting activities can cause re-rupture at the original muscle injury site and therefore appropriate assessment of severity and adequate rehabilitation are essential. Since re-ruptures cause the greatest amount of time lost from sporting activity, return to play should be determined by extent of muscle strain, muscle group, and demands of the sport placed on the individual athlete.
4.2.5.2 Contusion
Muscle contusions most commonly occur in the front of the thigh in the quadriceps muscle. This injury is known as a “charley horse,” “cork thigh,” and also “dead leg” (Trojian 2013). A muscle contusion usually results from a direct blow from an opponent (often the kneecap) or firm contact with equipment in high-contact sports such as football and basketball. The blow causes vascular damage and diffuse internal bleeding in the musculature, which is often highly vascularized at the moment of injury. Most of these injuries are relatively minor and do not limit sport participation. However, especially if the player continues to play after a severe contusion this may lead to a big hematoma. This results in swelling with characteristic muscle pain at rest. Muscle tear is not prominent in patients with muscle contusion.
4.2.5.3 Myositis Ossificans
An occasional complication of a muscle hematoma (and thus of muscle contusion and not of muscle strain) is myositis ossificans (Cushner and Morwessel 1992). This can be defined as ectopic ossification of the injured muscle tissue. The incidence is highest in collision sports and the location most frequently affected is the thigh. Myositis ossificans is most common following severe muscle contusions, but it can also occur in relatively minor muscle bleeding. The pathophysiology of ectopic bone formation has not been completely elucidated. If a muscle contusion does not resolve within 7–14 days, myositis ossificans should be suspected. Two to four weeks after the injury, characteristic ringlike calcifications of the muscle may already be visible on radiographs and ultrasound; not all patients with these calcifications will develop symptoms of pain and abnormal muscle function. Management of myositis ossificans is conservative and recovery is usually slow.
4.2.5.4 Cramp
A muscle cramp is a sudden, involuntary, painful contraction of a muscle or part of it, is self-extinguishing within seconds to minutes, and is often accompanied by a palpable knotting of the muscle. Muscle cramp either during or immediately after exercise is commonly referred to as “exercise-associated muscle cramping” (EAMC) (Minetto et al. 2013). Despite their “benign” nature, cramps are often very uncomfortable and can be temporarily debilitating. Moreover, exercise-associated muscle cramps may significantly impair athletic performance.
The lifetime prevalence of cramps in athletes has been reported to be as high as 30–50 % (Miller et al. 2010). Norris et al. reported a high prevalence of benign cramps in a wide group of healthy young subjects enrolled in an exercise class; 115 (95 %) of 121 had experienced spontaneous muscle cramps at least once (Norris et al. 1957). They preferably occur in calf and foot muscles, followed by the hamstrings and the quadriceps.
The etiology of EAMC remains unclear. The main risk factors for exercise-associated muscle cramps include family history of cramping, previous occurrence of cramps during or after exercise, increased exercise intensity and duration, and inadequate conditioning for the activity. Dehydration (and/or electrolyte depletion) often is given as an explanation for muscle cramps occurring in athletes, although this claim is not supported by scientific evidence. Recent experimental findings have proved unambiguously the relevance of spinal mechanisms and altered neuromuscular control in the generation and development of muscle cramps. However, several unresolved issues in cramp pathophysiology and management still remain and require further investigation (Minetto et al. 2013).
4.2.6 Tendon
Complete or partial tendon ruptures may occur acutely without a warning, usually in older athletes without a history of injury in that particular tendon. The two most commonly ruptured tendons are the supraspinatus tendon of the shoulder and the Achilles tendon (Longo et al. 2013; Murray and Gross 2013). Injuries to tendons generally occur at the musculotendinous junction. However, the Achilles tendon usually ruptures 2–5 cm above the insertion, which is considered the point of least blood supply. Partial tears are characterized by the sudden onset of pain and by localized tenderness, but they may be difficult to distinguish from tendinopathy. When investigation is indicated, ultrasound and MRI can be useful.
4.2.7 Bursa
The body contains many bursae situated usually between bony surfaces and overlying tendons and skin. A direct fall onto a bursa may result in acute traumatic bursitis due to bleeding into the bursa (Aaron et al. 2011). A septic bursitis may develop when bacteria enter through abrasions or a small wound over the bursa. The patient reports anterior knee pain and swelling. On physical examination, there is a prepatellar area of tenderness and a fluctuating swelling. In case of an infection, the area will be warm and red. Diagnosis can be confirmed by ultrasound.
4.2.8 Nerve
Acute nerve injuries are uncommon in athletes. The nerves most often injured are the ulnar nerve at the elbow and the common peroneal nerve at the neck of the fibula, as they are located superficially and susceptible to injury from a direct blow. Symptoms like tingling, numbness, and pain in the distribution of the nerve usually diminish quickly.
In case of “neuropraxia,” there will be paralysis or weakness of the muscles innervated by that nerve, in addition to sensory loss and/or pain in the sensory distribution of the nerve. These symptoms usually resolve spontaneously but slowly (Toth 2009).
4.3 Overuse Injuries
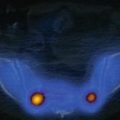
Overuse injuries occur gradually and their cause is not always evident. Repeated overloading causes an accumulation of small deformations of the tissue that finally lead to injury and pain when over time the tissue threshold is exceeded (Fig. 4.1).