PULMONARY ATRESIA, AND
DUCTUS ARTERIOSUS
CONSTRICTION
 PULMONARY STENOSIS
PULMONARY STENOSIS
Definition, Spectrum of Disease, and Incidence
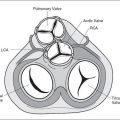
Pulmonary stenosis is defined as obstruction to right ventricular outflow due to pulmonary valve abnormalities, infravalvular (infundibulum) narrowing, or rarely supravalvular narrowing involving the main pulmonary artery or its branches. Valvular pulmonary stenosis, primarily due to fusion of the valve commissures, is the most common cause of pulmonary stenosis (Fig. 13-1). On occasion, pulmonary stenosis is due to unfused thickened dysplastic valve leaflets with associated pulmonary regurgitation. Unfused and dysplastic valve leaflets are seen in cases of pulmonary stenosis with Noonan syndrome (1). Infundibular thickening due to right ventricular wall hypertrophy is a common cause of pulmonary stenosis in the recipient twin of twin-to-twin transfusion syndrome. The severity of stenosis varies from mild lesions, typically missed prenatally, to severe lesions with associated hypertrophy of the right ventricle (Fig. 13-1) and tricuspid regurgitation. Pulmonary stenosis can progressively worsen in utero, resulting in critical pulmonary stenosis and atresia. Pulmonary stenosis can be associated with other cardiac anomalies such as tetralogy of Fallot. Isolated pulmonary stenosis, which occurs with an incidence of 0.73 per 1000 live births, is the second most common cardiac anomaly to ventricular septal defect and accounts for 9% of live births with congenital heart disease (2,3). Most cases of pulmonary stenosis are first diagnosed beyond the neonatal period probably due to the difficulty in the prenatal diagnosis of this lesion and its progressive
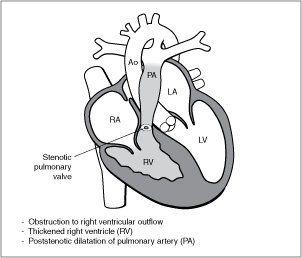
Figure 13-1. Pulmonary stenosis. LV, left ventricle; LA, left atrium; RA, right atrium; Ao, aorta.
nature in some cases (4). Recurrence of pulmonary stenosis is estimated at 2% for one affected sibling and 6% when two siblings are affected (5).
Ultrasound Findings
Gray Scale
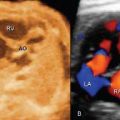
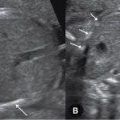
The four-chamber view in pulmonary stenosis shows right ventricular hypertrophy (Fig. 13-2) with bulging of the interventricular septum to the left ventricle. The right ventricular lumen may appear small due to the hypertrophied myocardium, and the tricuspid valve shows normal leaflet excursion with occasional tricuspid regurgitation, which may lead to right atrial dilation. Right ventricular wall hypertrophy is more commonly seen in the third trimester of pregnancy. Confirming the diagnosis of pulmonary stenosis is best performed by direct visualization of the pulmonary valve in the right ventricular outflow view, which shows abnormal excursion and thickening and doming of valve leaflets during systole (Fig. 13-3). Valve leaflets are visible within the pulmonary artery throughout the cardiac cycle in pulmonary stenosis as opposed to a normal pulmonary valve, where the leaflets abut the arterial walls during systole. The three-vessel view and the three-vessel-trachea view will also show poststenotic dilation of the pulmonary artery in many cases (Fig. 13-3). In mild to moderate pulmonary stenosis, ultrasound diagnostic signs are more subtle and primary detection is best achieved by the additional use of color Doppler.
Color Doppler
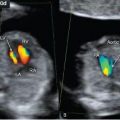
Color and pulsed Doppler are essential in confirming the diagnosis and in assessing the severity of pulmonary stenosis. Color Doppler of the pulmonary valve in the right ventricular outflow view typically shows turbulent antegrade flow with color aliasing (Fig. 13-4). Pulsed Doppler across the pulmonary valve demonstrates high-flow velocities exceeding 200 cm/sec (Figs. 13-5 and 13-6). Ductus arteriosus flow is antegrade in the majority of cases of pulmonary stenosis. The presence of retrograde flow across the ductus arteriosus, however, is a worsening sign associated with the development of pulmonary atresia and poor outcome (6). Tricuspid regurgitation, which may be absent in mild pulmonary stenosis and holosystolic in moderate or severe cases (Fig. 13-7), can be demonstrated using color Doppler in the four-chamber view. When the valve leaflets are dysplastic, pulmonary regurgitation is demonstrated on color Doppler and flow across the ductus arteriosus may be bidirectional in these conditions. Color and pulsed Doppler of the ductus venosus may show reverse flow during the atrial contraction phase of diastole (7).
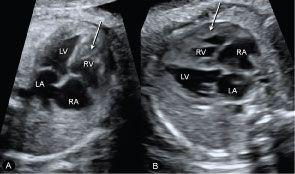
Figure 13-2. Apical (A) and lateral (B) four-chamber planes in two fetuses with pulmonary stenosis, showing hypertrophy of the right ventricular wall (arrows). LA, left atrium; RA, right atrium; RV, right ventricle; LV, left ventricle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree